MyHealthyGut: development of a theory-based self-regulatory app to effectively manage celiac disease
Introduction
Celiac disease is a chronic autoimmune disorder that affects approximately 1% of the North American population (1). Individuals with celiac disease typically report a range of physical (i.e., gastro-intestinal upset, migraines, body pain) and/or psychological (e.g., depression, anxiety) symptoms (2,3). Strict adherence to a gluten-free (GF) diet is currently the only treatment for preventing both short- and long-term consequences from celiac disease (e.g., infertility, intestinal cancers, osteoporosis) (4) and is usually (5-9), but not always (10) associated with improvements in quality of life. However, following a strict GF diet is difficult, and the evidence suggests that there is variation in rates of strict adherence (11-13). Furthermore, many individuals with celiac disease report reduced quality of life due to the burden of a restricted diet (14). Many individuals with celiac disease report persistent symptoms (e.g., gastrointestinal distress) despite being on a strict GF diet (15). As such, development of effective strategies to help people follow a strict GF diet, manage symptoms and cope with celiac disease is prudent.
Self-regulation is considered a crucial skill necessary for adherence to a medical regimen among people with chronic diseases (16,17). Findings from recent work highlight the importance of self-regulation to assist in the management of celiac disease (18,19). Indeed, higher self-regulatory efficacy (SRE; one’s confidence in one’s abilities to self-manage their behaviours to eat a strict GF diet) predicts fewer instances of accidental gluten consumption (18). Research suggests that self-regulation is a skill that can be taught (11), which involves self-monitoring, goal-setting and planning (17). Findings from recent studies demonstrate that self-monitoring is an essential component for changing dietary behaviours for weight loss (20-23). Furthermore, Michie and colleagues’ (24) comprehensive review revealed that the most effective interventions utilize self-monitoring in combination with one other control-theory based behaviour change technique (e.g., goal-setting, review of goals and/or progress). As such, an evidence-based tool that includes self-monitoring (i.e., of dietary behaviours and subsequent disease symptoms) and another control-theory derived technique (such as reviewing one’s diet and symptoms through a weekly progress report, a method of reviewing one’s goals to follow a GF diet) could be particularly effective in helping people living with celiac disease follow a strict GF diet.
Self-monitoring tools
Paper diaries have been the most frequently used tool for self-monitoring dietary behaviours (23). However, paper diaries can be tedious, time consuming and often inaccurate because participants can retrospectively backfill data (23). Drawing from the mobile health (mHealth) literature, the use of technology (i.e., smartphones) to self-monitor behaviours and promote health and fitness is gaining empirical evidence as an effective and efficient means to assist in self-monitoring dietary behaviours and disease symptoms (20-22,25,26). Indeed, 68% of Canadians own a smartphone (27) and 78% of smartphone owners do not leave home without their mobile device (28). Furthermore, apps that focus on diet, food or calorie counting are the second most commonly downloaded health and wellness apps (29). Interestingly, between June 2013–2014, health and fitness app usage grew 62%, whereas overall app usage only grew by 33% (29). Compared to paper diaries, the main benefits of e-diaries include (I) higher likelihood the data will be accurate because the user is more likely to fill in at the time of the behaviour (or symptom); (II) lesser burden on users because the app guides users through data to enter; and (III) reduced burden on researchers because the data are input in a useable and readable format (23). As such, smartphones provide an ideal opportunity for users to self-monitor dietary behaviours and disease symptomatology through e-diaries.
mHealth interventions
Preliminary findings of successful evidence-based mHealth interventions come from the field of weight loss and management of type 1 diabetes. For example, Burke and colleagues (20,22) report the findings of using personal digital assistants (PDA) compared to paper diaries to assist in a weight loss intervention for obese adults. Participants who lost the most weight were those who used the PDA and received individualized feedback. In addition, compared to participants who used paper diaries, participants who used PDAs had better adherence to self-monitoring records. Overall, regardless of how participants self-monitored (PDA or paper), self-monitoring and weight loss were positively related. In addition, an evaluation of a recent theory-based app (Motivation Engine) designed to increase exercise behaviour among inactive adults found that participants engaged in significantly more exercise and self-monitoring behaviour after using the app for an 8-week period compared to the control group that did not use the app (30). These findings highlight the importance of regular self-monitoring in order to change behaviour. Cafazzo (25) found similar results in an mHealth study designed to help adolescents manage type 1 diabetes through an app. Results indicated that using the app may have encouraged adolescents with type 1 diabetes to self-monitor their blood glucose more often, as measurements increased by 50% from pre-post intervention.
Free and colleagues (31) conducted a systematic review of mHealth technology-based interventions for disease management or behaviour change. To date, the majority of chronic diseases studied include cardiovascular disease, chronic obstructive pulmonary disease, HIV infection, diabetes, and lung cancer which can all be prevented by lifestyle choices (i.e., not smoking/smoking cessation, healthy behavioural choices including pertaining to diet, physical activity and safe sex). Findings from this systematic review provided some support for mHealth technology interventions to aid in the management of HIV and smoking cessation, however further high-quality trials are needed to adequately assess the effect of this new technology as an intervention strategy (31). Wang and colleagues’ integrative review (32) of smartphone interventions for the management of chronic diseases including diabetes, obesity, mental health and cancer, revealed three main positive findings, “patients with chronic conditions (I) felt secure in the knowledge that their illnesses were closely monitored; (II) participated in their own health management more effectively; and (III) felt that they had not been forgotten by their doctors and were taken good care of even outside the hospital/clinic”. As such, use of smartphones offer a promising avenue in chronic disease management and warrants future research. Despite the high prevalence of chronic gastrointestinal disorders today, there is currently a lack of evidence-based user-centered apps to support patients (33).
Objectives
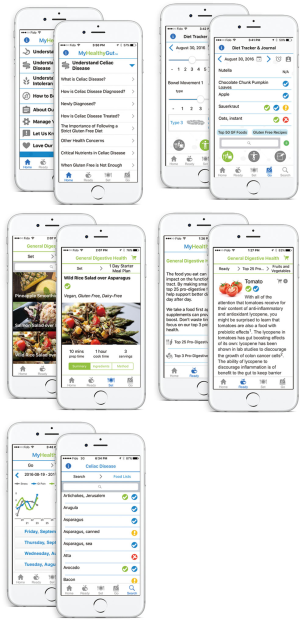
The overall goal of this study was to design, develop and pilot test a smartphone app to promote effective self-management of celiac disease and promote gut health. The purpose of Part 1 was to gather feedback from end-users (adults with celiac disease) regarding the desired functions, features and content of an app for celiac disease. The purpose of Part 2 was to pilot test the app (MyHealthyGut; see Supplement I and II for more information) with end-users and healthcare professionals.
Methods
Survey
Part 1—market research
Participants
One hundred and eighteen participants (Mage =39.25 years, 91.5% female, 94.9% Canadian) were recruited via the Canadian Celiac Association (CCA) webpage, CCA regional chapters’ emails, Facebook pages and Twitter postings. See Table 1 for additional participant characteristics. In order to maximize the representativeness and generalizability of the sample, we strove to fulfill three criteria: (I) to obtain responses from people across Canada in urban and rural communities; (II) to track the response rate so that we were aware of the demographics to which the findings can be generalized; and (III) to assure that data saturation was reached (i.e., no new responses coming up regarding desired content and features in the app). Recruitment materials advertised for people who had a confirmed diagnosis of celiac disease through blood test and/or biopsy.
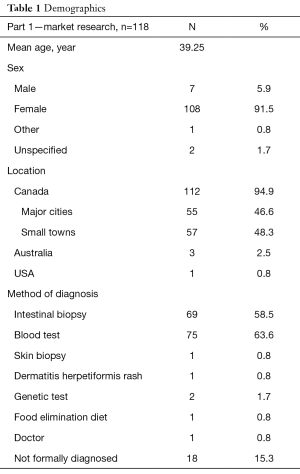
Full table
Procedure
Feedback was obtained through online surveys using the Drupal 7 online portal. Specific questions pertained to (I) how participants manage their celiac disease; (II) if participants felt there is a need for an app to help them cope with celiac disease; (III) the style of feedback participants would like to receive (i.e., a ‘coach’ that is assertive, fun, or supportive); and (IV) desired features, functions and content that should be provided in an app. All feasible suggestions obtained through survey responses were used to guide development of the content, features and functionality of the app. A registered dietician and specialist in integrative nutrition (Desiree Nielsen), behavior change specialist and diagnosed celiac (A. Justine Dowd), and an IT specialist (Darlene Higbee Clarkin) collaborated on the development of the app features, functionality and content. Due to budgetary constraints, the app was initially only designed for the iOS platform.
Part 2—pilot testing & feedback from end-users and healthcare professionals
End user participants
Thirty adults with a confirmed diagnosis of celiac disease (through blood test and/or biopsy) were recruited through social media (Twitter, Facebook), the Calgary CCA website, and word of mouth, to participate in pilot testing the MyHealthyGut app. All participants were required to own an Apple mobile device (iOS interface—iPad, iPhone or iPod), be diagnosed with celiac disease (blood test and/or biopsy) speak English, have access to computers, be over the age of 18, and to live in the Calgary, AB area. Based on McCurdie and colleagues’ (34) model for user-centered design of mHealth consumer apps, the participants were then asked to attend a focus group meeting after using the app for a 1-week period. Of the 30 recruited, 15 signed up for Wave 1 of the focus groups, of whom 7 attended [1 no show, 1 medical reasons (broken ankle the day before), 1 broke device during the trial, 1 no response after allocated to focus group, 4 too busy]. Wave 1 consisted of three focus groups with 2–3 participants allocated to each group, which is a common sample size for this type of pilot study (Mage =49.43 years; % female =100). A second round of pilot testing and Wave 2 of focus groups were conducted after integrating feedback from the first round. Twenty-two participants were recruited for Wave 2 of focus groups, of whom 5 attended (1 opted to switch to the healthcare professional part of the study, 2 had android devices, 4 were too busy, 10 did not sign up for a focus group after initial interest and consent). All five participants came to the same focus group (Mage =42.0 years; % female =40). All participants were provided free parking and paid $10.00 CDN for participating in the focus group.
Health care professional participants
Seventy-nine healthcare professionals interested and/or commonly involved in the diagnosis, treatment, and health of individuals with celiac disease (e.g., gastroenterologists, dietitians, naturopaths, and general practitioners) who had an iOS mobile device, responded to advertisements to provide feedback on the MyHealthyGut app. Recruitment was performed via direct emails to professional organizations and dieticians, postings on the CCA website, and social media postings (i.e., Twitter, Facebook). Of the 79 professionals who initially indicated eligibility and interest in the study, 4 dropped out because they did not have an iOS device, another 4 officially dropped out (2 no reason, 1 too busy, 1 found too much effort to participate), 1 tried to participate after the pilot was over and the full demo version of the app was no longer available and 63 did not complete the online feedback questionnaire). Participants were all female, and consisted of 5 dietitians, 1 physician and 1 medical student, 3 were diagnosed with celiac disease or reported gluten intolerance, had been practicing for an average of 8.86 years (range, 0–17 years), and 55% had patients who struggle with gastrointestinal disorders.
Procedure
The purpose of Part 2 of this study was to conduct a series of pilot testing on the MyHealthyGut app. During this phase, participants used the app for a 1- or 2-week period, after which they provided feedback through an online questionnaire and focus groups (end-users only). After all possible end-user feedback had been integrated from Wave 1 of pilot testing of testing, Wave 2 of pilot testing with targeted end-users (adults with celiac disease) occurred. For the final round of testing, healthcare professionals were recruited to provide feedback regarding the content and utility of the app in a healthcare setting through an online questionnaire.
End-user participants were provided access to the app for a 1-week period, in which they were instructed to explore and use the app as they would in day-to-day life and keep track of any thoughts, frustrations and comments on the content, features and functionality of the app. Participants were instructed to contact the app developer directly if any technological issues were encountered during the testing period. Focus groups occurred in small boardrooms at the University of Calgary and were conducted by the primary investigator (A. Justine Dowd), with research assistants (Colleen Jackson, Karen T. Y. Tang) attending to take notes throughout. Semi-structured focus group questions focused on the functionality, ease of use, and content of the app, as well as a discussion of the feedback raised by prior focus group(s). See Supplement III for the semi-structured focus group question guide.
After the focus groups from Wave 1 of pilot testing had been conducted, the investigators (A. Justine Dowd, Colleen Jackson and Karen T. Y. Tang) separately reviewed and summarized notes from the sessions, condensing into the top immediate and long-term changes needed for the app to be useful for users. The investigators then met and reviewed their findings, corroborating and discussing any discrepancies. These findings were then discussed with the app developer (Darlene Higbee Clarkin) and dietitian (Desiree Nielsen), and as many changes that were feasible based on finances and time were implemented prior to the second round of pilot-testing. The same process was followed for the Wave 2 focus group.
Healthcare professionals were given access to the app for a 2-week period, after which they were invited to provide feedback through an online questionnaire.
Measures
All measures were created for the current study and followed guidelines for an mHealth user-centered design process (34).
Part 1—market research
Celiac disease management strategies
Participants were asked to indicate how often they used the following strategies to manage celiac disease on a 1 (never) to 5 (always) scale, diet, medication, supplements, physical activity and mind-body therapies. An open text box was available to write down other celiac disease management strategies used. Participants were also asked if they felt there was a need for an app to assist in the self-management of celiac disease (yes/no).
Desired content, features and functions
Participants were asked to rank how important the following potential components of an app were to influence using the app, cost, ease of use, available functions, ability to connect with others, rewards or incentives, diet tracking, symptom tracking, nutritious GF recipes, meal plans, cooking tips, list of supplements, list of 100 nutritious GF foods. An open text box was available to write down other desired content, features and functions in an app for the management of celiac disease.
Type of health coach
Participants were asked to indicate which type of health coach they would prefer when using an app to help manage celiac disease: assertive, supportive, or fun. An open text box was available to write down other preferences on the type of health coach preferred in an app.
Part 2—pilot testing and feedback from end-users and healthcare professionals
The following measures were completed by the end user participants before [celiac dietary adherence test (CDAT) and SRE] or after (app usability and satisfaction) using the app for a 7-day period of time.
CDAT (35)
The 7-item CDAT was used to assess adherence to a GF diet. Four different aspects of adherence to a GF diet (i.e., celiac symptoms, self-efficacy, reasons to follow a GF diet, perceived adherence to a GF diet) with four different scales are assessed via the CDAT. An exemplar item is “I am able to follow a GF diet when dining outside my home” assessed on a 1 (strongly agree) to 5 (strongly disagree) scale. Responses to items are summed for a total score where lower scores indicate stricter adherence to a GF diet. Leffler (35) provides evidence of face validity and test-retest reliability (Pearson r=0.82).
SRE
A revised 6-item measure developed by Strachan and Brawley (36) was used to assess participants’ confidence in their ability to self-regulate their behavior to consume a GF diet. Participants were asked to respond to items regarding their self-regulatory abilities for healthy eating on a standard 0 percent (not at all confident) to 100 percent (completely confident) self-efficacy scale (37). An exemplar item is “How confident are you that you can motivate yourself to eat a strict GF diet over the next month?”. Data derived from this instrument have demonstrated acceptable reliability in assessing SRE for eating a GF diet among adults with celiac disease adults (38). In the present study, scores derived from this instrument displayed acceptable levels of internal consistency (Cronbach α=0.87).
App usability and satisfaction
Participants were asked to respond to the following questions: (I) “How easy is the MyHealthyGut app to use?” on a 1 (not at all easy) to 5 (very easy) scale; (II) “How likely are you to use the MyHealthyGut app in the future?” on a 1 (not at all likely) to 5 (very likely) scale; (III) “How satisfied are you with each of the following functions of the MyHealthyGut app (i) diet tracking, (ii) symptom journaling, (iii) 7-day meal plan content, (iv) meal planning, (v) cooking tips, (vi) supplements, (vii) 100 nutritious GF food list?” on a 1 (very unsatisfied) to 5 (very satisfied) scale; (IV) “How much do you agree with the following statement? The MyHealthyGut app will improve my health”, on a 1 (strongly disagree) to 5 (strongly agree) scale; (V) “What was your first reaction to the MyHealthyGut app?” on a 1 (very negative) to 5 (very positive) scale; (VI) “How would you rate the quality of the MyHealthyGut app overall?” on a 1 (very low quality) to 5 (very high quality) scale; (VII) “How well did the MyHealthyGut app meet your needs?” on a 1 (not at all well) to 5 (extremely well) scale; (VIII) “How likely would you be to purchase the MyHealthyGut app?” on a 1 (not at all likely) to 5 (very likely) scale; (IX) “How likely are you to use the MyHealthyGut app to monitor your diet and/or track symptoms?” on a 1 (not at all likely) to 5 (very likely) scale; (X) “Did anything about the MyHealthyGut app confuse you?” on a Yes or No response scale, (XI) “Do you have any favorite apps or features within an app that you would like us to include in the MyHealthyGut app?” on a Yes or No response scale; and (XII) “How likely is it that you would recommend MyHealthyGut to a friend or colleague?” on a 1 (not at all likely) to 5 (very likely) scale.
The following measures were completed by the healthcare professionals at before (demographics) or after (app feedback) using the app for a 7-day period of time.
Demographics
Participants were asked to report the following demographic information: profession, practice area, length of time practicing, sex/gender and approximate percentage of patients with gastrointestinal disorder.
App feedback
Healthcare professionals were asked to respond to the following open-ended questions: (I) What was your overall impression of the MyHealthyGut app? (II) Does the nutrition information provided fall in line with what you advise your patients? (III) Would you recommend the app to another healthcare provider? (IV) How easy is the MyHealthyGut app to use? (V) How satisfied are you with the diet tracking feature in the MyHealthyGut app? (VI) How satisfied are you with the symptom journaling feature in the MyHealthyGut app? (VII) How satisfied are you with the educational information provided in the MyHealthyGut app? (VIII) How satisfied are you with the evidence-based supplements provided in the MyHealthyGut app? (IX) How satisfied are you with the food recommendations feature in the MyHealthyGut app? (X) What are the top 3 things (functionality, content, usability) that need to be changed or modified in the app and why? and (XI) What are the top 3 things (functionality, content, usability) that you liked about the app and why?
Results
Part 1—market research
Market research findings
Participants most commonly managed celiac disease daily through diet (95.8%) and supplements (35.6%), and weekly through physical activity (35.6%). The majority of participants indicated that they never used medication (62.7%) or mind-body therapies (58.4%) as management strategies for celiac disease (see Table 2 for frequency of management strategies). The majority of participants indicated that they felt there was a need for an app for those with celiac disease (90.7%; 107/118). When asked which attributes they would most like in a health coach (i.e., style of writing in a health app), participants indicated that a supportive coach would be preferred (83.9%), followed by fun (45.8%), and 24.6% of participants indicating a preference for an assertive health coach.
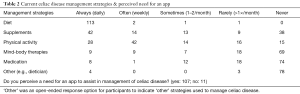
Full table
When asked to prioritize factors that influence use of a smartphone app, participants indicated that ease of use (60.2%; 71/118), available functions (53.4%; 63/118), nutritious GF recipes (40.7%; 48/118) and cost (39.8%; 47/118) were very important determinants of using an app to manage celiac disease (see Table 3 for summary of responses). Following the top four most important components, 33.9% (40/118) of participants felt a list of 100 most nutritious foods was a very important determinant of using an app, 28.0% (33/118) felt evidence-based supplements were very important, 28% (33/118) also thought that the ability to track symptoms was very important, 24.6% (29/118) felt cooking tips were very important, and fewer than 20% of participants felt that the ability to connect with others, track diet, or have meal plans were very important determinants of using an app. Eight participants indicated the following ‘other’ (i.e., not listed on our questionnaire) features were very important: lists of GF restaurants, barcode scanning ability, and education about celiac disease and gut health. A feature that the majority of participants reported as low importance was inclusion of rewards/incentives (5.9%; 7/118).
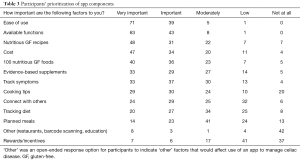
Full table
Part 2—pilot testing and feedback from end-users and healthcare professionals
Sample characteristics of end-users
The mean CDAT score was 12.33 (SD =1.63), indicative of an excellent to very good adherence to a GF diet (35). Participants reported very high confidence to self-manage behaviours to follow a strict GF diet (i.e., SRE; M =97.50, SD =3.98).
App usability and satisfaction
Overall, there was a range of positive and negative responses regarding the perceived usability and satisfaction with the MyHealthyGut app (see Table 4 for full summary of findings). Participants felt the MyHealthyGut app was relatively easy to use (M =3.60, SD =1.12), generally satisfied with the features (Ms ≥3.00, except for symptom journaling, M =2.80), felt the app would help improve their health (M =4.00, SD =0.92), of satisfactory quality (M =3.33, SD =1.12), likely to use to monitor diet and/or symptoms (M =3.07, SD =1.16), and likely to recommend to a friend or colleague (M =3.27, SD =1.22). In terms of negative responses, participants reported less than the neutral (i.e., value of 3; on a 1–5 scale) response to the following items: being unlikely to use the app to manage celiac disease in the future (M =2.46, SD =1.12), negative first reaction to the app (M =1.20, SD =0.94), the app did not meet their needs (M =2.27, SD =1.22), relatively unlikely to purchase the app (M =2.73, SD =1.28), and the majority of participants were confused about some aspect of the app (10 out of 15).

Full table
End-user focus groups—Wave 1
The recommended changes in the first wave of focus groups fit into three broad themes pertaining to the functions, features and content of the app; as well as overall general feedback. This resulted in six key recommended changes to improve the app (see Table 5 for summary of recommended changes). The first and most prominent feedback to emerge was that participants’ enjoyment of the app increased with time and use. Participants indicated that initially they weren’t aware of the full capabilities of the app, and found navigation of the app confusing and frustrating. Given that app use was not as intuitive as participants would like, they suggested having engaging and simple instructions (e.g., improved onboarding) to simplify using the app and accelerate their enjoyment of it.
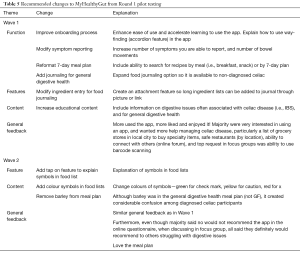
Full table
The second recommended change pertained to the symptom tracking feature that tracks the severity of three celiac related symptoms (fatigue, bowel movements, and GI pain), over time and in relation to diet. While this feature was lauded as crucial to the newly diagnosed and those still experiencing uncontrolled symptoms, participants felt that the three symptoms did not include symptoms that all participants experienced or wished to track. Therefore, it was suggested that adding additional symptoms (e.g., fatigue, hair loss), or keeping the label general (e.g., celiac related symptoms) with an open text box, would increase the applicability of the diet and symptom tracking feature.
The third recommended change was regarding the 7-day GF meal plan. While the feedback regarding the recipes and the visual appeal of the page was overwhelmingly positive, participants didn’t feel it was clear that it was a meal plan, instead it seemed an amalgamation of recipes. It was suggested that a more user-friendly approach would allow the user to select recipes by meal (e.g., breakfast, entree, snacks), in a 7-day format, or by favourites.
The fourth and fifth recommendations pertained to the diet journaling functioning and feature. This feature was seen as a key part of the app, and participants highlighted that while other diet journaling apps exist, the focus of MyHealthyGut on food types, rather than quantities was appreciated. However, it was felt that inputting the ingredients of a complicated recipe was tedious. Participants suggested that the ability to attach a file to your diet tracker, such as an image of the recipe in question, would allow all ingredients to be tracked and diminish the time required for entry. Participants felt that given the current attention to healthy diets and the increased prevalence of obesity and digestive issues, that the diet journaling function would be beneficial to more than just a diagnosed celiac population. It was therefore suggested that this function be available through a separate package, not exclusively in the celiac package.
The sixth category highlighted by participants was that given the high prevalence of other digestive issues, such as irritable bowel syndrome and lactose intolerance among individuals with celiac disease, it would be beneficial to include additional information on these issues. Specific education topics that were suggested included: signs that something still isn’t right, information on common digestive issues, and diet changes recommended for those issues. Based on the first round of focus groups the main change made to the app was to improve the onboarding experience (i.e., provide a guided tour of the app when users first download and open the app).
Focus group—Wave 2
The recommended changes in the second wave focus group fit into two broad themes pertaining to the content and features of the app; and overall general feedback. This resulted in three key recommended changes to improve the app (see Table 5 for summary of recommended changes). While participants found the food lists helpful, and thought the lists would be particularly helpful for people who are newly diagnosed with celiac disease, they were unclear of what the symbols meant. It was recommended that each symbol have a specific color (easier to see differences; recommended change one) and when you touch it, a pop up box explains what each symbol means in the food search categories (i.e., blue check mark means “it’s gluten-free”, green check mark means the food is “good for digestion”, yellow exclamation mark means “be cautious—high cross-contamination risk”, and a red x means “don’t eat… contains gluten”; recommended change two).
The third main recommended change was to remove barley from the meal plan. Although barley was not in the GF meal plan, it was in the general digestive health meal 1-day meal plan (i.e., not recommended for those with celiac disease, recommended for people trying to improve general digestive health); nevertheless, the presence of barley created considerable confusion for most participants, and thus it was recommended to replace barley with another GF grain.
Interestingly, while the majority of participants indicated online that they would not recommended the app to other people, in the focus groups participants explained that while they did not typically discuss health apps or digestion with friends and colleagues, if they knew someone struggling with digestive health they would recommend the MyHealthyGut app. Further, the second wave focus group thoroughly enjoyed the meal plan. After discussing the findings from the second wave focus group with the app development team, all three recommended changes were implemented in the subsequent version of the app.
Pilot testing and feedback from healthcare professionals
A summary of the feedback from the online questionnaire completed by healthcare professionals is shown in Table 6. Similar to the end-users, there was a range of positive and negative feedback provided by the healthcare professionals on their experiences using the MyHealthyGut app. The majority of healthcare professionals reported positive perceptions of the app (5 of 7) and felt that the nutrition information provided was in line with what they advised their patients (5 of 7). One healthcare professional noted that she “was not well enough informed—the app provided even more information”, while another suggested that there were “too many high FODMAP foods for this population” (FODMAP stands for fermentable oligosaccharides disaccharides monosaccharaides and polyols and refers to the recommended diet for individuals suffering from irritable bowel syndrome). In addition, 6 out of the 7 healthcare professionals indicated there was not any evidence-based information missing from the app (1 highlighted the need for more information on FODMAPs and irritable bowel syndrome). The majority (5 of 7) of healthcare professionals said they would recommend the app to a colleague. Furthermore, participants overall reported being more satisfied than not with the features of the app, the diet tracking (M =3.86, SD =0.70), symptom journaling (M =3.71, SD =0.76), 7 day meal plan (M =3.14, SD =1.36; main feedback was to include more recipes low in FODMAPs), educational information (M =3.86, SD =1.46; constructive feedback from 1 participant was she felt the information was better suited for a website), supplements (M =4.00, SD =0.58), and food recommendations (M =4.43, SD =0.58).

Full table
Findings from the healthcare professionals’ experiences using the app were discussed with the developer (Darlene Higbee Clarkin) and dietitian (Desiree Nielsen). Based on this round of pilot testing, a considerable amount of content was added to the education sections pertaining to irritable bowel syndrome and the low FODMAP diet.
Discussion
The purpose of this study was to create and pilot test a theory-based smartphone app to help people to effectively manage celiac disease and promote gut health. End-users—adults with celiac disease—reported a need for an app to help manage the disease and that ease of use, available functions, nutritious GF recipes and cost were the top four factors in determining potential use of an app. End-users also wanted the ability to track diet and symptoms, lists of nutritious GF foods, supplements to promote gut health, cooking tips for the GF diet and the ability to connect with others. The app was created based on findings from market research in Part 1 of this study. The evidence-based information in the app was written by a registered dietitian (Desiree Nielsen) and a health psychology researcher and diagnosed celiac (A. Justine Dowd). Pilot testing the app led to constructive feedback from end-users and healthcare professionals regarding the content, features and functionality of the app. The current version of the app is based on the feedback from pilot testing and is available to download in the iTunes store.
Smartphones provide the opportunity to enable users to use technology to enhance their ability to effectively and efficiently monitor behavior (39). Given the strong link between chronic diseases and lifestyle choices (i.e., behaviour), smartphones can thus assist in management of chronic diseases. The MyHealthyGut app was created based on the large body of research supporting the importance of self-regulation in (I) behaviour change (17,40,41) and (II) chronic disease management (42). By using the MyHealthyGut app on a regular basis, users will be (I) informed (by the educational content) about their condition or potential causes or gastrointestinal distress, (II) provided with a list of gut health promoting foods to consume (III) have the ability to easily track diet and corresponding symptoms and share this information with healthcare providers. These functions are all key components of successful behaviour change (17,41).
There are several key strengths of this study that deserve attention. First, a participatory approach was utilized to create the app, which included involvement of end-users from the beginning and through an iterative process of pilot testing and revising the app. Specifically, we obtained feedback from adults with celiac disease regarding the content, functionality and features that created the app so that it would be useable by the target market. After creating the app based on end-user feedback, we then completed two waves of pilot testing and focus groups with end-users, followed by a final wave of pilot testing by healthcare professionals to ensure the app met users’ needs and wants. This process is recommended by McCurdie and colleagues in order to follow the user-centered design approach to increase user engagement and thus maximize the likelihood of a successful intervention (i.e., the app used on a regular basis) (34). Compared to only gathering feedback via self-report questionnaires, the inclusion of focus groups enabled us to capture rich data regarding the users’ experiences with the app. Second, the content in the app is evidence-based and referenced in the app.
Several weaknesses of this study should also be acknowledged. While we recruited 52 end-users and 79 healthcare professionals, 12 end-users (23%) and 7 healthcare professionals (9%) actually participated in the study. A number of end-users and healthcare professionals indicated that they had intended to participate, however, with the pilot test occurring in the summer, it was difficult to participate as intended because of reduced summer hours and vacation. It is possible that if the pilot had been run another time of year we may have been able to obtain feedback from a larger group of participants; unfortunately, this was not financially or logistically feasible for this study. Nonetheless, evidence of data saturation was present as the same themes for factors participants liked and wanted changed were evident and no new major changes came up during subsequent focus groups. One should also take into account that the majority of end-users who participated in focus groups reported very good to excellent adherence to a GF diet and high SRE to follow a GF diet. If we had been able to recruit newly diagnosed adults with celiac disease or those struggling with disease management, other modifications or requests may have been elicited.
From a technology developmental perspective, it was challenging to balance user requests with the available budget. For example, the majority of focus group participants reported that they would very much like the ability to search for safe GF restaurants and grocery stores within the app as well as the ability to scan the barcode of food items to see if they are safe to consume (i.e., GF and no cross contamination). While the developers plan to add these functionalities, current budget constraints prohibit the addition of these user-identified helpful features.
A future direction for this research is a randomized controlled trial investigating the effects of using the app on adults diagnosed with celiac disease key psychological outcomes (e.g., quality of life, SRE for GF diet) and adherence to a GF diet. This trial was conducted in 2016 and the results are currently under analysis. Future versions of the app will be revised based on the findings from this randomized controlled trial.
The MyHealthyGut app provides affordable content, functions and features designed to assist in the management of celiac disease and optimization of general gut health. Additional resources are needed for people struggling with gut health issues as they are multi-faceted and often need a multidisciplinary approach. The app is a beneficial first step in management of a complicated and frustrating disease and in promotion of optimal gut health for the general public.
Supplement I Screenshots of the main features of MyHealthyGut
Supplement II Summary of the app
The app is free to download and provides a wealth of information free of charge including basic education on gut health, top 25 pro-digestive foods and top 3 pro-digestive supplements and 1-day digestive health meal plan. Users can opt for an in-app purchase ($8.49 USD for everything described below, smaller packages also available depending on which features users want in an app) to obtain detailed information on celiac disease, how to follow a strict GF diet, and other information in dealing with celiac disease (e.g., potential health concerns, critical nutrients in celiac disease and what to do when feeling unwell despite being on a GF diet), gluten intolerance (e.g., non-celiac gluten sensitivity, wheat allergy and irritable bowel syndrome), the top 50 pro-digestive foods and top 10 pro-digestive supplements, 7 day digestive health meal plan, and comprehensive food and symptom journal and food database. As of February 2018, there have been 7,990 downloads of the free version of the app, 340 of the all-in-one package, 15 of the meal plan and tracker only and 9 of the top food lists and search safe food database.
Supplement III Semi-structured focus group question guide
Start with building rapport. Explain who you are, why interested in the study. Grateful for participants’ time and help. Then ask each participant to give a brief intro, say name, how long been diagnosed with celiac disease, how they find it to be coping with celiac (encourage to be about 1 min intros).
- Please tell me about your general experience with using the app over the past week.
- Tell me what you thought about the following features of the app:
- Diet tracking;
- Symptom journaling;
- 7-day meal plan;
- Meal planning;
- Supplements;
- Tips on cooking for people with celiac disease;
- 100 most common nutritious GF foods.
- What else can we do to simplify downloading and using the app?
- What did you think of the pricing/bundle options?
- What is the most important component of the app (e.g., functionality, content, usability) that need to be changed and why?
- What is the best component of the app (e.g., functionality, content, usability) that you liked about the app and why?
- Would you recommend that someone else with celiac disease use the app? Why or why not?
Acknowledgements
This work was supported by the Calgary, Vancouver and Kamloops Chapters of the Canadian Celiac Association in collaboration with a Mitacs Accelerate Internship and a Strategic Opportunity Grant from the Calgary Foundation. Special thanks to KORE Digital Health Therapeutics and Stephen Drozdik for developing the app and to Terry Walters for creating the meal plans.
Footnote
Conflicts of Interest: A. Justine Dowd, Desiree Nielsen and Darlene Higbee Clarkin are co-founders of the MyHealthyGut app.
References
- Lionetti E, Gatti S, Pulvirenti A, et al. Celiac disease from a global perspective. Best Pract Res Clin Gastroenterol 2015;29:365-79. [Crossref] [PubMed]
- Green PH, Jabri B. Celiac disease. Annu Rev Med 2006;57:207-21. [Crossref] [PubMed]
- Guandalini S, Assiri A. Celiac disease: A review. JAMA Pediatr 2014;168:272-8. [Crossref] [PubMed]
- Green PH, Cellier C. Celiac disease. N Engl J Med 2007;357:1731-43. [Crossref] [PubMed]
- Mustalahti K, Lohiniemi S, Collin P, et al. Gluten-free diet and quality of life in patients with screen-detected celiac disease. Eff Clin Pract 2002;5:105-13. [PubMed]
- Nachman F, del Campo MP, Gonzalez A, et al. Long-term deterioration of quality of life in adult patients with celiac disease is associated with treatment noncompliance. Dig Liver Dis 2010;42:685-91. [Crossref] [PubMed]
- Nachman F, Maurino E, Vazquez H, et al. Quality of life in celiac disease patients: Prospective analysis on the importance of clinical severity at diagnosis and the impact of treatment. Dig Liver Dis 2009;41:15-25. [Crossref] [PubMed]
- Roos S, Karner A, Hallert C. Psychological well-being of adult coeliac patients treated for 10 years. Dig Liver Dis 2006;38:177-80. [Crossref] [PubMed]
- Burger JPW, de Brouwer B. Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin Nutr 2017;36:399-406. [Crossref] [PubMed]
- Zingone F, Swift GL, Card TR, et al. Psychological morbidity of celiac disease: A review of the literature. United European Gastroenterol J 2015;3:136-45. [Crossref] [PubMed]
- Hall NJ, Rubin G, Charnock A. Systematic review: Adherence to a gluten-free diet in adult patients with coeliac disease. Aliment Pharmacol Ther 2009;30:315-30. [Crossref] [PubMed]
- Lovik A, Skodje G, Bratlie J, et al. Diet adherence and gluten exposure in coeliac disease and self-reported non-coeliac gluten sensitivity. Clin Nutr 2017;36:275-80. [Crossref] [PubMed]
- Hall NJ, Rubin GP, Charnock A. Intentional and inadvertent non-adherence in adult coeliac disease. A cross-sectional survey. Appetite 2013;68:56-62. [Crossref] [PubMed]
- Casellas F, Rodrigo L, Lucendo AJ, et al. Benefit on health-related quality of life of adherence to gluten-free diet in adult patients with celiac disease. Rev Esp Enferm Dig 2015;107:196-201. [PubMed]
- El-Salhy M, Hatlebakk JG, Gilja OH, et al. The relation between celiac disease, nonceliac gluten sensitivity and irritable bowel syndrome. Nutr J 2015;14:92. [Crossref] [PubMed]
- Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav 2001;28:769-82. [Crossref] [PubMed]
- Bandura A. The primacy of self-regulation in health promotion. Appl Psychol Int Rev 2005;54:245-54. [Crossref]
- Dowd AJ, Chen MY, Jung ME, et al. Prediction of adherence to a gluten-free diet using protection motivation theory among adults with coeliac disease. J Hum Nutr Diet 2016;29:391-8. [Crossref] [PubMed]
- Sainsbury K, Halmos EP, Knowles S, et al. Maintenance of a gluten free diet in coeliac disease: The roles of self-regulation, habit, psychological resources, motivation, support, and goal priority. Appetite 2018;125:356-66. [Crossref] [PubMed]
- Burke LE, Styn MA, Sereika SM, et al. Using mHealth technology to enhance self-monitoring for weight loss: a randomized trial. Am J Prev Med 2012;43:20-6. [Crossref] [PubMed]
- Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc 2011;111:92-102. [Crossref] [PubMed]
- Burke LE, Conroy MB, Sereika SM, et al. The effect of electronic self-monitoring on weight loss and dietary intake: a randomized behavioral weight loss trial. Obesity (Silver Spring) 2011;19:338-44. [Crossref] [PubMed]
- Burke LE, Warziski M, Starrett T, et al. Self-monitoring dietary intake: current and future practices. J Ren Nutr 2005;15:281-90. [Crossref] [PubMed]
- Michie S, Abraham C, Whittington C, et al. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol 2009;28:690-701. [Crossref] [PubMed]
- Cafazzo JA, Casselman M, Hamming N, et al. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res 2012;14:e70. [Crossref] [PubMed]
- Higgins JP. Smartphone Applications for Patients' Health and Fitness. Am J Med 2016;129:11-9. [Crossref] [PubMed]
- Catalyst. Infographic: The 2015 Canadian smartphone market. 2015. Available online: http://catalyst.ca/infographic-2015-canadian-smartphone-market/. Accessed September 8, 2015.
- The Canadian Press. Smartphone use way up in Canada, Google finds. CBC News, 2013, July 29.
- Flurry Insights Blog. Health and fitness apps finally take off, fueled by fitness fanatics. 2014. Available online: http://flurrymobile.tumblr.com/post/115192181465/health-and-fitness-apps-finally-take-off-fueled
- Voth EC, Oelke ND, Jung ME. A Theory-Based Exercise App to Enhance Exercise Adherence: A Pilot Study. JMIR Mhealth Uhealth 2016;4:e62. [Crossref] [PubMed]
- Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013;10:e1001362. [Crossref] [PubMed]
- Wang J, Wang Y, Wei C, et al. Smartphone interventions for long-term health management of chronic diseases: an integrative review. Telemed J E Health 2014;20:570-83. [Crossref] [PubMed]
- Spiegel B. Mobile health apps: E-wave of the future. GiHealth. ND. Available online: https://mygihealth.io/expert-opinions/mobile-health-apps-e-wave-of-the-future. Accessed April 9 2018.
- McCurdie T, Taneva S, Casselman M, et al. mHealth consumer apps: the case for user-centered design. Biomed Instrum Technol 2012.Suppl:49-56. [Crossref] [PubMed]
- Leffler DA, Dennis M, Edwards George JB, et al. A simple validated gluten-free diet adherence survey for adults with celiac disease. Clin Gastroenterol Hepatol 2009;7:530-6, 536.e1-2.
- Strachan SM, Brawley LR. Reactions to a perceived challenge to identity: A focus on exercise and healthy eating. J Health Psychol 2008;13:575-88. [Crossref] [PubMed]
- McAuley E, Mihalko SL. Measuring exercise-related self-efficacy. In: Duda JL. editor. Advances in sport and exercise psychology measurement. Morgantown, WV: Fitness Information Technology, 1998:371-81.
- Dowd AJ, Jung ME. Self-compassion directly and indirectly predicts dietary adherence and quality of life among adults with celiac disease. Appetite 2017;113:293-300. [Crossref] [PubMed]
- Ernsting C, Dombrowski SU, Oedekoven M, et al. Using Smartphones and Health Apps to Change and Manage Health Behaviors: A Population-Based Survey. J Med Internet Res 2017;19:e101. [Crossref] [PubMed]
- McClelland MM, Geldhof J, Morrison FJ, et al. Self-Regulation. In: Halfon N, Forrest CB, Lerner RM, et al. editors. Handbook of Life Course Health Development. Cham: Springer, 2017:275-98.
- Bandura A. Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes 2004;50:248-87. [Crossref]
- Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Educ Behav 2014;41:499-508. [Crossref] [PubMed]
Cite this article as: Dowd AJ, Jackson C, Tang KT, Nielsen D, Clarkin DH, Culos-Reed SN. MyHealthyGut: development of a theory-based self-regulatory app to effectively manage celiac disease. mHealth 2018;4:19.