Mobile-based blended learning for capacity building of health providers in rural Afghanistan
Introduction
In Afghanistan, redevelopment of health systems and difficult security and geographic conditions have resulted in gaps in the availability, training, and capacity building of the health workforce (1). In response to a 2006 World Health Organization Report highlighting the importance of health human resources (HHR) for the functioning and performance of a labor-intensive healthcare system, more attention has been directed towards ensuring that the healthcare system is more responsive to the needs and expectations of the population (1).
Afghanistan has gone through difficult times with internal conflicts and natural disasters over the past three decades. Most Afghans have witnessed unbearable violence and atrocities at some point in their lives. As a consequence, mental health problems in Afghanistan are far more profound than seen in other countries (2). Many mental health disorders are connected to such experiences. Experts estimate that 60% of the Afghan population suffers from mild to severe mental illness (3). Mental health and treatment of mental illnesses have been identified by the Afghan government as important priorities within health system improvement (4,5).
The state of mental healthcare resources in Afghanistan has been quite dismal. In a study conducted with Afghan refugees migrating to Pakistan, nearly 80% of patients have had a diagnosis of post-traumatic stress disorder (PTSD). Nearly half (47.9%) reported family history of mental illness, while almost a quarter (23.3%) had a physical disability or long term illness (4). There are only two qualified psychiatrists, 61 other doctors, 37 nurses and 40 other mental health workers in Afghanistan (5). Improving awareness related to mental health problems in the community and ensuring effective delivery of mental health care remain essential in order to reduce stigma and for the early identification of those who require attention for mental health problems. Accomplishing this goal also requires capacity building of health providers working in the community or in health facilities in the areas of mental health. Due to difficulties in arranging regular face-to-face sessions, blended learning is seen as a practical and cost-effective solution for capacity building.
Blended learning is a term increasingly used to describe the way eLearning is being combined with traditional classroom methods and independent study to create a new, hybrid teaching methodology (3). It characterizes a fundamental variation in the way facilitators and learners approach the learning experience. There is a general consent between education innovators that blended learning has three prime components:
- In-person classroom activities facilitated by a qualified educator/doctor;
- Online learning resources, often including pre-recorded lectures, video clips, online articles, pictorial presentations given by experienced doctors and experts;
- Designed independent study time directed by material learned in the lectures and skills established during the face to face sessions.
Blended Learning can provide improvement in access to information, ease in updating, distribution, and standardization of content, personalized tutoring, and accountability. A comparative cross-sectional study showed that blended learning is statistically and significantly better than traditional learning in domains of the educational environment, such as access to material and comfort of updating and distribution, and in all types of examination: written, objective structured clinical, and case scenarios (6). Learners have more control over the content, learning sequence, pace of learning, time, and often, media, which allows them to tailor their experience to meet personal learning objectives. Internet technologies permit the widespread distribution of digital content to many users simultaneously anytime and anywhere (3).’’
Background of the project
The reported initiative is a multi-organizational collaboration between Aga Khan Health Service, Afghanistan (AKHS, A); Tech4life Enterprises; and the University of Calgary, Canada to improve mental health among young adults in Afghanistan. Digital health solutions are used for reducing stigma, educating community members about mental health, empowering local health providers with interactive guidelines and blended learning programs, and to improve referrals through teleconsultations (7,8). For the project, Tech4Life Enterprises developed a mobile-based learning platform, while the content was developed collaboratively by the partners. The main objectives of the Mental Health Blended Learning application were to:
- Improve the knowledge of health providers based in the community and health facilities about common mental health problems.
- Empower and enable the health providers to screen patients for common mental health problems and provide appropriate advice.
The blended learning component of the project used a combination of:
- Face-to-face interaction with senior health providers and mental health experts in order to convey knowledge about the specific health problems and their treatments.
- Live and/or recorded sessions conducted in an online learning environment that allow for digital content, personalized learning, pre and post assessments, and collaboration with instructor and fellow learners (9).
The learning takes place with the help of mobile version of Moodle (moodle.com) and Skype (skype.com) as these solutions are highly cost effective and accessible. Moodle is a learning platform designed to provide educators, administrators, and learners with a single robust, secure, and integrated system to create personalized learning environments (10). Moodle can be used to conduct online courses and to support face-to-face teaching, learning, and training.
Common mental health problems were identified during the baseline survey conducted with the health providers. Four modules of blended learning were then created for these key areas which include depression, PTSD, anxiety, and drug abuse. The training material for each module was developed based on the guidelines suggested by the World Health Organization’s Mental Health Gap Action Programme (mhGAP) guidelines, and the related curriculum suggested by the Ministry of Public Health, Afghanistan. Each module was taught over 12–16 weeks period.
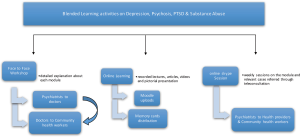
Activities performed during each module included:
- A pre-assessment at the beginning of each module to get information about the initial knowledge of health providers.
- Smartphones were provided to all the health providers in the intervention districts.
- Moodle IDs were generated for all registered users involved in the project.
- Delivery of online learning material including recorded lectures, videos, supporting articles, and pictorial and animated presentations. This material was uploaded on the Moodle site, and also provided in the form of memory cards so that every health worker with a Moodle ID could easily access the material.
- Face to face sessions conducted by the consultant doctors and other facility-based health providers at the primary health care centers. In these sessions, doctors delivered information in the form of power-point presentations.
- Weekly Skype sessions on different topics, conducted by the psychiatrist based at the provincial hospital to the facility-based health providers in their case area. The session were followed by a question & answer period during which relevant cases were discussed.
- A second post-assessment at the end of the module.
- Results of these assessments were statistically analyzed in order to evaluate each specified module.
This paper presents the process and results of ‘Depression’ module.
Methods
The team in Afghanistan conducted pre and post intervention assessments for each module in order to assess improvement in the level of knowledge of health providers. The post implementation assessment was conducted with reference to the information outlined in the mhGAP guidelines. The assessments took place under the supervision of AKHS, A management and project advisors to avoid bias from the project team. Paired t-tests were then used to equate pre- and post-intervention marks. The results are reported using the effect size calculated by the standard deviation method, i.e., standardized mean differences.
Study districts
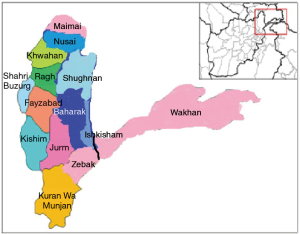
The study took place in seven districts of Badakhshan province. Four districts were used as case sites (Baharak, Ishkashem, Shughnan, and Nusai), while three districts acted as control sites (Wakhan, Zebak, Maimai). The trainings were coordinated by the project teams located in the provincial capital Faizabad. Figure 1 shows the map of Badakshan province with all the districts.
Activity workflow
The process of blended learning for each module is described above and also shown in the following diagram. A questionnaire using a set of multiple choice questions was developed by the psychiatrists associated with the project. The same questionnaire was used for pre-assessment at the beginning of the module and post- study after the completion of the module. Figure 2 shows the details of blended learning activities:
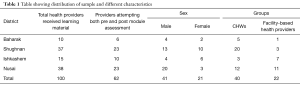
This blended learning study was initiated on 1st November, 2014. By end of December 2015 the depression and psychosis module were introduced in all four case districts. Material recommended by the experts was translated into English and Dari languages, and shared with the team members based in Faizabad. The material was also transferred into memory cards, which were distributed to CHWs and facility-based health providers. Blended learning material was distributed to 60 community based health workers (CHWs), 30 facility based health providers (HPs), 10 physicians & support staff members, and 5 MOPH observers. A total of 6 pre- and post-assessment responses from Baharak district, 10 from Ishkashem district, 23 from Nusai district, and 23 from Shughnan district were received.
The study was approved by national Ethics Review Committee of the Ministry of Public Health, Afghanistan and the institutional ethics board of University of Calgary. Informed consent was obtained from all participants.
Analysis
After the confirmation of assumptions, the paired t-test was found to be suitable for comparison of pre- and post-intervention scores. An effect size value of significance <0.3 was considered weak, whereas higher than this is considered as moderate or strong. We also calculated the degree of freedom in order to know the accuracy of the sample population used in research. Researchers from Tech4Life Enterprises and AKHS, A conducted the analysis together to avoid any bias.
Comparison of gains in knowledge scores between health providers living in the intervention sites and the control sites was only done for the depression module. The difference was calculated between the pre and post intervention knowledge scores to find the gain. The gains in both groups were compared using one-way Anova. For other modules, only pre and post module assessments were done in the case districts. These results will be reported in a separate paper.
Results
Descriptive analysis
Table 1 provides the overall sample size & distribution by districts, gender, and level of service. The facility-based health providers were mainly doctors and nurses who were based at the district-level health centers, while the CHWs were located in the communities. The average age of facility-based health providers was lower (30 years), compared to that of CHWs (41 years).
Full table
Pre & post module scores of depression in intervention districts
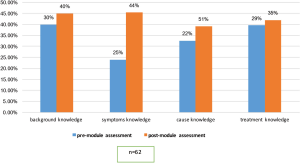
Comprehensive analysis of all four case districts in Badakhshan province showed that the knowledge in all four specific areas of depression, i.e., background, symptoms, cause, and treatment improved from pre-module test to post-module test (Figure 3). In the assessment of knowledge, several questions related to the etiology of depression, common symptoms and recommended treatment were asked. Significant change was noticed in the case districts, where overall knowledge scores changed from 45% in pre-intervention test to 63% in post-intervention test (P value ≤0.001, DF =61).
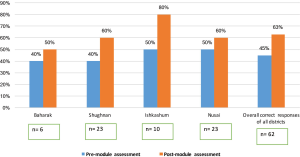
Similar results were obtained in each study district where a significant change in total knowledge of depression was observed. In Baharak district pre to post module test scores changed from 40% to 50% respectively (P value =0.007, DF =5). Shughnan district showed correct responses raised from 40% to 60% in pre to post module tests (P value =0.001, DF =22). In Ishkashem, 80% correct responses were submitted in post-module analysis compared to 50% in pre-module (P value =0.003, DF =9). Finally, in Nusai district, around 60% people responded correctly to the questions asked in post-module assessment, while 50% correct responses were observed in the pre module test (P value =0.003, DF =22).
In addition to comparing the overall knowledge scores, the pre and post intervention scores were also compared for the four categories of questions, namely background, symptoms, causes and treatment. Overall background knowledge of pre to post module test scores changed from 30% to 40% respectively (P value =0.001) (see Figure 4). Overall knowledge of symptoms showed correct responses raised from 25% to 44% in pre to post module tests. This is a significant change in knowledge of symptoms of depression where its (P value =0.001). Knowledge related to causes of depression from overall districts showed 51% correct responses in post-module analysis compared to 22% in pre-module (P value =0.008). Finally, in treatment knowledge of depression, around 35% people responded correctly to the questions asked in post-module assessment, while 29% correct responses were observed in the pre module test (P value =0.01).
Comparison was done for the depression scores between 62 results obtained from the intervention districts (Baharak, Ishkishim, Shugnan and Nusai) and 32 results obtained from control districts (Wakhan, Maimai and Zabak). Significant difference was seen between the gain (increase in total scores) in intervention districts compared to the gains in control districts (16.06 vs. 6.80; P value=0.009). Table 2 describes the overall results
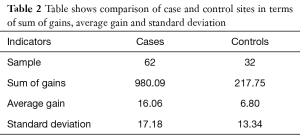
Full table
Significant differences between the gains were also observed in different categories of questions within the depression module. The knowledge gains about background and causes of depression showed significantly higher improvement in cases compared to controls. The knowledge gains for symptoms and treatment of depression were also higher in cases, but the results were not statistically significant. The results are shown in the Table 3.
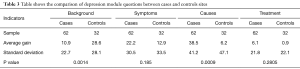
Full table
Discussion
The evaluation has shown that there was significant improvement in the awareness of health providers about mental health problems. The intervention also helped in overcoming mental health issues by referring cases through teleconsultation, and showed high degree of acceptance for continuing these types of interventions.
The key points that strengthen this study include:
- Participation of each member in the pre & post module assessments from community health workers [40] and facility-based health providers [22].
- Use of standardized training material for empowering health providers.
- Provide information efficiently and effectively through eLearning sites and on a smart phones.
- Analyzing the results under the supervision of joint partners.
- Initiative was undertaken in discussion with the Ministry of Public Health and therefore was consistent with their goals
Some difficulties encountered during this study include:
- Initially, low access of e-learning website ‘Moodle’ in some areas limited the loading of heavy files. To overcome this barrier, teaching material was provided in the form of memory card chips, which resolved the problem.
- Unfavorable weather situation of case districts limited the activities, such as face-to-face lectures. This situation delayed the completion of the modules on time.
- The study was controlled such that the statistical tests compared pre- and post-module-intervention scores to confirm the effectiveness of the intervention. Those health providers who only completed either pre or post module assessment had to be excluded. Since over 60% providers completed both surveys from all intervention areas, there should be no major impact on the results.
- Clinical outcomes of the capacity building program have not been assessed as part of this study. This will be done in the longer term.
- The questionnaire was not independently validated.
The results will be disseminated globally to raise knowledge about the program in other parts of the world.
Conclusions
Mental health is often a neglected area of human health care. Improved mental health care depends on effective professional development, which is challenging in conflict zones and remote areas like Afghanistan. Blended learning offers an effective solution to these problems and our data suggests that effective interventions are possible. Further research is needed to confirm that the gains in knowledge reported here translate into better practice and improved mental health.
Acknowledgements
This project is funded by grand challenges Canada.
The authors are thankful to the Aga Khan Health Service, Afghanistan (AKHS, A) and the Ministry of Public Health, Afghanistan for their support and guidance. The authors wish to thank all the project and field staff for their support. Special thanks to Dr. Ebadullah Hedayat, Dr. Faqir Faqiri, and Mr. Mir Wais Abdullah (Aga Khan Health Services Afghanistan) for their help in project activities.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by national Ethics Review Committee of the Ministry of Public Health, Afghanistan and the institutional ethics board of University of Calgary. Informed consent was obtained from all participants.
References
- Al-Sawai A, Al-Shishtawy MM. Health Workforce Planning: An overview and suggested approach in Oman. Sultan Qaboos Univ Med J 2015;15:e27-33. [PubMed]
- Sayed GD. Mental Health in Afghanistan: Burden, challenges and the way forward. Available online: http://documents.worldbank.org/curated/en/692201467992810759/Mental-health-in-Afghanistan-burden-challenges-and-the-way-forward
- Salehi Z. Over 60pc Afghans suffer from mental health problems. Available online: Read more: http://www.rawa.org/temp/runews/2010/10/10/over-60pc-afghans-suffer-from-mental-health-problems.html
- Naeem F, Mufti KA, Ayub M, et al. Psychiatric morbidity among Afghan refugees in Peshawar, Pakistan. J Ayub Med Coll Abbottabad 2005;17:23-5. [PubMed]
- World Health Organization. Who-Aims Report On Mental Health System In Afghanistan. Available online: http://www.who.int/mental_health/evidence/Afghanistan_WHO_AIMS_Report.pdf
- Makhdoom N, Khoshhal KI, Algaidi S, et al. ‘Blended learning’as an effective teaching and learning strategy in clinical medicine: a comparative cross-sectional university-based study. Journal of Taibah University Medical Sciences 2013;8:12-7. [Crossref]
- Improving mental healthcare of the youth of Afghanistan, using mHealth and Telemedicine. Accessed on 17 January 2017. Available online: http://tech4lifeenterprises.com/mental-health-project-afghanistan/
- Khoja S, Scott R, Husyin N, et al. Impact of simple conventional and Telehealth solutions on improving mental health in Afghanistan. J Telemed Telecare 2016;22:495-8. [Crossref] [PubMed]
- Poon J. Blended learning: An institutional approach for enhancing students' learning experiences. Journal of Online Learning and Teaching 2013;9:271-88.
- Bothe M, Fischer-Lescano A. Protego et obligo. Afghanistan and the paradox of sovereignty. German Law Journal 2002;3:5.
Cite this article as: Tirmizi SN, Khoja S, Patten S, Yousafzai AW, Scott RE, Durrani H, Khoja W, Husyin N. Mobile-based blended learning for capacity building of health providers in rural Afghanistan. mHealth 2017;3:14.