Digital apothecaries: a vision for making health care interventions accessible worldwide
Introduction
Over the last 50 years, psychological interventions have been developed and tested in a large number of clinical outcome studies. The preponderance of the empirical evidence supports the efficacy and effectiveness of these interventions for a number of health conditions, including both mental and physical disorders. However, most people who suffer from these disorders do not have access to these evidence-based interventions. Thus, the prevalence of mental, emotional, and behavioral disorders for which there are demonstrated effective interventions has not decreased in the general population. Moreover, health disparities abound: individuals lower in the socioeconomic structure and in less industrialized countries often have less access to health care.
In the last 40 years, there has been a revolution in the development of digital technologies that have gradually penetrated the farthest reaches of the globe. In the 1980s, personal computers were introduced; in the 1990s, the World Wide Web began to provide information globally, and the introduction of smartphones in the 2000s brought the Web literally to our fingertips. Clinicians quickly recognized the potential of creating interventions that could be delivered digitally, using text, graphics, audio, and eventually video elements. Unlike printed matter or older mass media, such as radio, television, and audio and video recordings, which only allow one-way communication, internet-based websites and mobile applications have interactive features that allow users to input data that can be used to trigger appropriate responses from the program and that can also be used to track clinical progress. A number of digital interventions including web-based and mobile health applications are now available to anyone in the world with access to the internet. But, most of these digital interventions are not tested (1), nor are they designed by or with health care professionals (2). On the other hand, recent meta-analyses clearly show that guided and unguided digital interventions are effective for such disorders as depression (3-5), cause less deterioration in users than control conditions (6), and have even been shown to prevent new episodes of depression (7). Platforms to direct users to credible and effective digital interventions for specific health conditions should thus be a high priority.
This article describes and expounds on the concept of “digital apothecaries” (8), that is, internet portals that contain links to and evaluations of evidence-based digital interventions. The authors have experience in the development, evaluation, and dissemination of such interventions. What follows is their joint recommendations on enhancing the potential of digital apothecaries and cautionary advice about possible unintended consequences.
Digital apothecaries
The term “digital apothecary” refers to an online collection of digital interventions. It is intended to hark back to the image of an old-fashioned pharmacy that provided herbal and chemical ingredients as well as advice on how to use them to address health problems. The word is still in use in several European languages to denote licensed pharmacies. But, it stems from an Ancient Greek word meaning “a repository or storehouse.” Thus, digital apothecaries would be online repositories that provide ready access to a number of digital interventions, including websites, mobile apps, and other digital tools designed to have preventive or treatment effects. Unlike old-fashioned apothecaries, which relied on the pharmacist’s clinical judgement, digital apothecaries could prominently provide the basis for each offering’s effectiveness based on empirical data. Ideally, the digital interventions or the apothecaries themselves would continually collect and transparently present outcome data, so that users would have a basis for choosing which to use.
There are already examples of pioneering digital apothecaries. Many of these examples have functioned primarily to direct people to potential options for specific symptoms or disorders. For example, the United Kingdom’s National Health Service (NHS) sponsors a digital app library (https://apps.beta.nhs.uk/) that currently promotes tools for cancer, chronic obstructive pulmonary disease, dementia, dental health, diabetes, healthy living, learning disabilities, mental health, and pregnancy and child health. Apps are vetted prior to their inclusion but no specific details are provided about effectiveness. A similar effort is supported by the U.S. Department of Veterans Affairs. The Veteran’s Health Administration National Center for Posttraumatic stress disorder (PTSD) system has developed a set of many apps focused on specific health topics that are in the public domain. These apps, among others, are available in the VAMobile App store (https://mobile.va.gov/appstore/veterans) and include apps and Internet interventions addressing PTSD, depression, sleep problems, anger, smoking cessation, alcohol use, parenting, and emotion regulation, and is intended for use by veterans and mental health providers within the Veterans Health Administration as well as others, globally, who may find them useful. This digital apothecary is useful because all apps have been created and vetted by a reliable and trusted source. However, it fails to include the vast array of tools developed outside of Veteran Affairs and the Department of Defense.
Other models of digital apothecaries are those that identify and evaluate digital interventions from diverse sources and disseminate information based on these evaluations to consumers. An early effort in this domain is the Beacon website (https://beacon.anu.edu.au/), which aims to help health care consumers and clinicians find high-quality digital interventions (9). It was launched in 2009 at the Australian National University with funding from the Australian government. Interventions included in Beacon were reviewed by two researchers to determine the strength of the research evidence and rated on a seven-point scale. Although Beacon was last updated in 2016, it currently consists of 445 listings (340 websites, 59 mobile apps, 46 support groups) in 40 health categories including 28 mental health categories. Users were also invited to contribute reviews. The Beacon site is currently being updated and undergoing expert review of its processes to ensure that it can optimally feed in to the Australian Government’s Head to Health digital mental health services portal (https://headtohealth.gov.au) and will therefore commence reviewing additional interventions in the future.
PsyberGuide (www.PsyberGuide.org) is an active version of a digital apothecary. Founded in 2013, PsyberGuide is a non-profit project of One Mind, a philanthropic organization promoting research on brain health. The goal of PsyberGuide is to empower consumers to make responsible and informed decisions about internet sites and mobile applications for mental health. PsyberGuide achieves this goal through two functions: identification and evaluation of digital interventions. Inclusion on PsyberGuide does not represent an endorsement of those products, but rather is meant to provide a thorough review of the research evidence supporting an app, user experience and usability, and issues related to data security and privacy. As such, rather than producing a single score, each product is rated on multiple facets including credibility, user experience, and transparency of data security and privacy. Credibility and user experience ratings actually only correlate at an r=0.22 (1), suggesting that products that have the most research evidence supporting their efficacy are not necessarily the most usable or user-friendly. This demonstrates the usefulness of multi-faceted assessments within digital apothecaries as the real-world effectiveness of digital interventions is likely driven by multiple aspects (e.g., use of evidence-based behavior change techniques, ease of use, user appeal and persuasiveness).
None of these examples, however, fully realize the dream of providing wide-ranging access to a broad range of digital interventions, and consistently compiling detailed information regarding their effectiveness. These examples, however, demonstrate several challenges for digital apothecaries moving forward including balancing comprehensiveness vs. usefulness for a given user base, identifying new products, keeping reviews current (both in terms of changes to the knowledge supporting the intervention and updates to the intervention itself), and reaching consensus on the process for identifying and evaluating products.
Digital apothecaries and traditional clinical practice
Digital interventions can be offered on their own but can also be great aids for providers. Digital apothecaries could help clinical practitioners identify digital interventions to either augment their traditional therapeutic methods or suggest evidence-based interventions their clients could use to address additional issues, use while waiting for services, or to help prevent relapse after in-person care has ended.
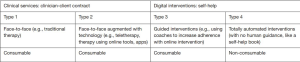
Figure 1 presents four types of possible health interventions: type 1 consists of traditional in-person clinical services that do not use digital interventions; type 2 consists of in-person clinical services augmented by digital interventions or what has been referred to elsewhere as “blended care” (10). Both type 1 and type 2 services involve a clinician-client/patient contract, in which a licensed professional provides therapeutic services to an individual and assumes responsibility for the conduct of treatment.
Types 3 and 4 are self-help interventions, which do not involve a therapeutic contract. Let’s begin with describing type 4 interventions, which, being self-help, totally automated interventions, are most similar to the use of self-help books. Though the interactive elements that digital interventions make possible may enhance the power of the intervention, the user is not offered official clinical care. Authors of self-help books are not expected to take on clinical responsibility for the reader once they present materials they believe will be helpful. Similarly, the developers of such self-help tools are not entering into a therapeutic relationship with the user, though this should be made explicit. Type 3 interventions are often referred to as “guided” interventions (11). They add human support to the digital intervention to increase adherence, provide additional explanation of the digital content, and encourage the user to complete the intervention. Human support could be in the form of phone calls, emails, texts, video conferencing, or in-person sessions. The individuals providing this support are typically not licensed professionals although when they are it does raise ethical and legal questions as to whether a therapeutic contract is established.
Digital apothecaries could include a range of type 2, 3, and 4 interventions. The question of which interventions would be “good enough” to include is a challenging issue, which we consider in the next section.
Threshold for inclusion in evidence-based digital apothecaries
We would argue that, regardless of the exact threshold for inclusion that is selected (e.g., specific number of studies, required samples sizes, etc.), there should be some minimum criteria for inclusion in evidence-based digital apothecaries. What the threshold should be for inclusion is an interesting challenge. On the one hand, making the threshold for entry easy to achieve will allow for a multitude of options which could be investigated within the context of the apothecary. If the threshold for entry were high, e.g., allowing only products with effectiveness established through numerous large randomized controlled trials, then only programs originating from very well-funded groups (i.e., those that can afford to run large treatment trials) would be included. Further, it can take years to accumulate the necessary outcome data, and slow evaluation is especially problematic for digital interventions where the technology is constantly evolving (12,13). An easy entry bar could thus foster innovation and more widespread evaluation of new programs. On the other hand, it is essential that the public have access to those programs with the best available research support and that it is protected from programs that are likely to have iatrogenic effects. There are potentially serious costs to offering programs that are totally untested. These include both direct costs from programs that cause harm (e.g., worsening mood) and more indirect opportunity costs because a person who is completing an unhelpful intervention at the apothecary may then not receive a more helpful intervention (e.g., because they assume all programs will be similarly ineffective). Thus, finding the right middle ground of making entry for new programs into the apothecary feasible, but also incorporating safeguards, is essential. There are many entry models to consider. Evaluating a new program’s evidence base and keeping that evaluation up-to-date as new evidence accumulates is not a simple undertaking. For instance, both the American Psychological Association’s new Clinical Practice Guidelines initiative (http://www.apa.org/ptsd-guideline/index.aspx) and the United Kingdom’s well-established National Institute for Health and Care Excellence (NICE) guideline development process (https://www.nice.org.uk/) follow the Institute of Medicine’s guideline standards (14). The guideline development process involves an extremely rigorous—but thus also expensive and very time consuming—independent systematic review process that requires considerable evidence from high quality research studies before an intervention can receive a recommendation from a panel of experts (15). A more moderate threshold for entry could be modeled on the Society of Clinical Psychology, which followed Chambless and Hollon’s (16) recommendation that a treatment can be deemed “efficacious” if its efficacy has been established in two well-designed studies from independent research groups (typically randomized controlled trials, though there are other methods that can meet the criteria; see https://www.div12.org/psychological-treatments/).
By setting minimum standards for inclusion and reporting of evidence and focusing on the information needs of program users and referring clinicians, a digital apothecary may encourage standardization across research groups to facilitate comparisons across interventions. For example, it may encourage researchers to use best practice guidelines in reporting outcomes (17), to routinely measure and report negative effects in a systematic manner (18), to report real-world data, as well as data from controlled studies, and to include analyses that are meaningful to clinicians including program completion rates, clinical significance, and reliability of change (19).
Where it is not feasible to provide controlled outcome research for individual interventions, content analyses can assess the degree to which such interventions are consistent with clinical best practice and incorporate components that are likely to be “active”. Taxonomies provide standardized language and classifications to assist comparisons. For example, the behavior change technique taxonomy (CITATION) (20) classifies 93 behavior change techniques within 16 categories and has been used to evaluate mobile apps (21) and in the design of new interventions (22). An earlier iteration of this taxonomy has been incorporated into ratings of mobile app quality provided in a government portal (https://www.vichealth.vic.gov.au/media-and-resources/apps-rating-process).
Interventions for what? Disorder-focused vs. symptom-focused tools
Linked with the concept of what to include is the question of what the tools within a digital apothecary should be focused on and how the apothecary should be organized. Although early digital interventions were developed with disorder-specific purposes, an increasing number of interventions are now available or being developed for common symptoms or problem areas such as sleep (23), procrastination (24), or relationship distress (25). Relatedly, many digital health interventions have begun to take a transdiagnostic focus to be relevant for a host of psychological disorders (26,27). This is consistent with trends in behavioral and cognitive therapies more generally which have been moving towards transdiagnostic approaches (28), “common elements” (29), or evidence-based kernels (30) to create tools that might be useful for a variety of people experiencing different mental health conditions. Two important considerations impact the decision on how to approach disorder-focused vs. symptom-focused tools. First, how might people search for tools within an apothecary and second, how might this distinction impact the evaluation of such tools.
Little information is known about how and why people seek digital interventions for mental and behavioral health. It is very likely that many of these individuals, however, have not pursued traditional treatment resources. In a large web-based global smoking cessation trial over two-thirds of the visitors (68.6%) had not used any other methods to stop smoking prior to visiting the website (31). As such, it is unclear if people would know the right disorder-focused search terms to assess relevant resources. We recently conducted a survey that asked people what terms they would use to search for mental health apps. About a third of the sample indicated disorder-focused terms such as anxiety, depression, or bipolar. Another third of the sample indicated treatment-focused terms such as mood tracker, mindfulness, or cognitive-behavioral therapy (CBT). The remaining sample either focused on outcome terms like calm or happy, or indicated they really did not know where to start. As such, it that appears when it comes to intervention discovery, that disorder- and symptom-focused terms are pathways through which people search for appropriate products. Digital apothecaries could approach this issue in a variety of ways: by including screening tools that assess a variety of symptoms and point people to specific option or by tagging an intervention with a variety of labels to allow for discovery in multiple ways.
It is also important to consider different ways of presenting information, including effectiveness information, to the users of the interventions. Users of an apothecary would likely want to know: will this intervention work for me? In light of this, evaluation questions focused on general benefit or perceived usefulness might help provide users answers to this question irrespective of a disorder or symptom-focus. Another way to approach this question is what are the disorders or symptoms that an intervention can be expected to address and what is the magnitude of the expected benefit. Users could also be provided with easy-to-interpret ratings of strength of recommendations, based on established criteria. One advance that could help people understand likely benefit in both disorder and symptom paradigms would be evaluation tools that could draw from open text reports of benefit through methods like natural language processing. This has been demonstrated in the context of depression using chart review (32), and additional efforts could apply similar logic to benefits from digital interventions.
As sample sizes increase sufficiently, outcomes for subgroups of users could be made available. For example, outcomes by gender, age, socioeconomic status, education, ethnicity, language, religion, and so on.
Description of what digital apothecaries are intended to do
Digital apothecaries are intended to increase the reach of evidence-based health interventions to reach many more people than are served by traditional health care. Ideally, these individuals would include difficult-to-reach and underserved populations. See section on addressing diversity, below, for an expanded discussion of this goal.
They are also intended to provide low-cost alternatives to traditional health care, which relies almost entirely on consumable interventions. Consumable interventions are those that once used are spent forever and can never be used to serve another patient—such as a psychotherapy hour or dose of medication. Non-consumable interventions are those that can be used again and again without losing their therapeutic power. Type 4 digital interventions, such as totally automated websites or mobile apps, are non-consumable interventions that be used anytime and anywhere. This means that their marginal cost, that is, the cost of providing it to one more person, gradually approaches (though never reaches) zero. A website or an app that costs $100,000 to create costs $1,000 per user if 100 people use it, $100 per user if 1,000 people use it, $1 per user if 100,000 use it, and 10 cents per user if one million people use it. Psychotherapy sessions (type 1 or type 2 interventions) generally cost one hour of a professional’s time, no matter how many clients seek therapy (notwithstanding the relative efficiencies of group therapy). Similarly, guided interventions (type 3 interventions) require human intervention, which makes them consumable, and thus substantially more expensive than type 4 interventions. We display the consumable vs. non-consumable distinction as the final row in Figure 1.
Digital apothecaries are also intended to provide information on the efficacy of the interventions, so that users can rely on empirical evidence to make their decisions. Ideally, digital apothecaries would encourage developers of these interventions to present outcome data on adherence, clinical outcomes, and clinical outcomes for key demographic groups (gender, age, language, education, income, religion, ethnicity, and so on).
In addition, digital apothecaries have the potential to set standards for digital interventions by encouraging developers to abide by whatever guidelines are set for inclusion.
Digital interventions will not have much impact at the population level unless they are actually tested in a way that allows anyone from the intended audience to participate in the outcome studies. This will increase the likelihood that the outcome study findings will be generalizable when scaled up for routine use. However, in order to reach large segments of the population, methods to increase utilization rates will need to be developed. Some of these methods might be innovative ideas for direct-to-consumer dissemination. For example, we envision the possibility of requiring printing the URL of evidence-based smoking cessation websites or apps on all cigarette packs. It is obvious that merely increasing the “supply” of such interventions has not been sufficient and so other advances in the field should focus on novel ways to increase the “demand” for and engagement with the interventions, possibly borrowing theories and concepts from marketing, gamification, or related fields. Much work needs to be done on both the recruitment and retention side for digital interventions to fulfill their promise of delivering adequate doses of care to those in need of services.
Apothecary applications for practice
An interesting application of a digital apothecary is its potential to contribute in real-world settings such as private practice and corporate or institutional settings. A digital apothecary could encourage clinicians in private practice settings to integrate evidence-based practices, could optimize care for those being seen in private practice settings, and provide behavioral health resources to individuals in large organizations without a need to see someone in specialty mental health practice.
Ideally, digital apothecaries would highlight for clinicians innovative methods to evaluate their clinical outcomes. Digital tools can provide unique and possibly unobtrusive methods to enhance care (33,34). Technology approaches can provide ongoing treatment assessment, address client adherence/attendance, provide options for peer support, and allow for in-between session client/therapist communication, which can all supplement or enhance the therapeutic process (see Figure 1, type 2, face-to-face augmented with technology). The capacity for technologies to track outcomes and other process variables can greatly enable the movement toward “Measurement-Based Care” (35-37), in which mental health providers and managers use outcomes information to guide their decision making and monitor progress during treatment. Ambulatory assessment of mood, anxiety, activity level, sleep, cognitive functioning, and social behavior can enhance a clinician’s knowledge of client’s real-world, in situ, functioning. Such assessment approaches can also provide feedback to the client about their own functioning, enhance their awareness, and further engage them in the therapeutic process. For example, an ecological sampling method via smartphone can inform both the clinician and client how mood/anxiety symptoms fluctuate and what circumstances/contexts may be associated with those changes such as when a client is in a social situation, or exercising, or engaged in meaningful hobby, or when they are alone. Technology can also provide a novel framework for clinicians and clients to interact, provide quick reinforcement or feedback, and track/record triggers to address during the next in-person meeting.
An apothecary can also provide a fascinating opportunity to bring evidence-based programs that could address the well-being of employees of large institutions or corporations. A digital delivery system could help address common barriers to care such as stigma about seeking mental health care; a need to train clinicians in evidence-based approaches; and address the logistics of where to go for care and finding the time to go to a clinician’s office (38). An evidence-based digital apothecary could provide well-being programs that address general behavioral health skills and may serve as preventive trainings addressing areas like stress management, resilience training, and mindfulness training (39-41). It could help extend our focus beyond treatment into prevention, for example, by teaching users skills (e.g., mood management methods) before they develop problems.
Addressing diversity
Evidence suggests that Internet and mobile technologies hold much promise for under resourced communities which experience significant burden from mental health problems as well as numerous contextual stressors such as poverty, war, conflict, natural disasters and other types of trauma (42,43). Mental health service use in these communities is often limited by clinician shortages, clinic availability, inadequate training of providers, and attitudinal and logistic barriers that prevent access to much needed treatment. Existing models of service delivery that require intensive and consumable resources are failing to meet the needs of these communities, and disparities in mental health care continue to rise. At present, there is limited but growing evidence to support the use of digital interventions in these communities, such as studies examining massive open online interventions (MOOIs) in lower middle income countries (44), telemedicine with rural communities (45,46), Internet interventions (47,48), and mobile based interventions with ethnic minorities (49-51). Some of these interventions have been used as stand-alone treatments while others leverage the use of community health workers to facilitate delivery of interventions. The use of a paraprofessional workforce may be an important adjunct to a digital apothecary, given data suggesting that some interventions may require at least minimal human contact to be effective (52,53). The growth of task sharing interventions (54,55), in which lay helpers are trained to offer evidence-based mental health interventions, presents an opportunity to explore integration of layperson delivery enhanced by use of effective technology interventions.
Although a digital apothecary has the potential to address many barriers that deter use of evidence-based treatments for diverse communities, the cultural appropriateness of these interventions will remain a topic of debate. The dilemma is whether to withhold interventions from any group on which the intervention has not been tested versus making interventions accessible to all, hoping that, even if there are differential outcomes, enough people will benefit to make universal access the preferable option. Digital apothecaries could contribute to providing answers to this conundrum based on empirical evidence. Specifically, our call to provide users with outcome information for various demographic groups will result in users’ ability to make data-based decisions on which interventions are likely to benefit individuals with their demographic characteristics. Eventually, sufficient data could provide increasingly accurate predictions of potential benefit at the individual level. It will also be critical to track iatrogenic effects as a function of group memberships and identities, so that there is ongoing evaluation for the possibility of differential rates of harm following from interventions.
A digital apothecary may integrate digital technologies, data science, and the mental health field, to function globally, transcend cultural factors (56), and enable “advanced personalized care” (57). A digital apothecary allows more people to access services, generating large scale datasets that could extend standard data sources (e.g., self-report) with potentially millions of data points from diverse users to inform machine learning based algorithms and assist with decision making (58).
Big data can inform cultural and linguistic adaptations of digital interventions with more diverse populations than are typically included in randomized trials. Data inputs may include images, GPS, voice-samples, etc. Machine learning may identify subtypes of conditions, encapsulate how conditions are experienced in diverse cultures and languages, flag risks, and recognize voice and text patterns as predictors of cognitions (e.g., suicidal thinking), behaviors or disease (59). It would be interesting, for example, to determine if the same voice patterns reflect clinically significant mood changes even if people speak different languages. Machine learning could also enhance the efficiency and accuracy of the adaptation and translation of digital content.
As data from “environmental sensors, wearables, and biofeedback devices” are integrated, services may be better customized for the patient’s clinical needs (59). Virtual human mental health providers may be sensitive to and adapt to cultural aspects, including mannerisms (e.g., eye contact) and language, in order to establish better rapport and facilitate effective communication (59,60). Algorithms such as artificial neural networks may enhance predictions that could improve the ability to “match patients with the most effective treatments” (61).
Disparities in health care may persist in machine learning and artificial intelligence. Access to digital services is essential to ensure the broadest inclusion in data points that inform algorithms. Proposed solutions include policies to enable underserved populations to access and utilize “mobile and other health apps, personal health records, and/or participate in population-based research without incurring network data charges” (62).
Given the amount of resources needed to create culturally adapted evidence-based treatments, the feasibility of tailoring every digital intervention to every community that needs it is limited. Using existing adaptation frameworks, one approach might be to only tailor digital interventions when there is evidence to suggest that the intervention is not effective or does not engage the intended population (63). Such a data-driven approach might assume universal effects until evidence suggests otherwise. Some of the kinds of cultural adaptation identified (64) are relatively straightforward: language of the intervention, use of cultural symbols and sayings (metaphors), incorporation of cultural knowledge or content, and consideration of treatment context. In a review of cultural adaptations of CBT interventions for depression (65), adaptations focusing on the enhancement of acceptability (as opposed to more substantial changes in content) were associated with large effect sizes. Other research suggests that CBT interventions can work with those in very different cultural contexts, if adapted for the culture and situation of participants (66). However, while cultural adaptations may be necessary to a greater or lesser extent, we propose that technology may offer other alternatives.
As an example, some digital interventions, such as attention bias modification (ABM) for anxiety disorders (67), may be inherently less culturally and linguistically influenced than others. ABM uses a probe detection task to retrain one’s implicit attentional bias away from threat. Visual stimuli, such as neutral and negative (anxious, scared, worried, etc.) faces, are used in this context. ABM is brief, requiring only 4–6 weeks of computer/tablet-based practice, and requires minimal literacy (ability to read instructions). Alternatively, there are other interventions such as mindfulness-based meditation or breathing exercises which can be largely image and/or demonstration based and also not require much in regard to cultural or linguistic adaptations.
A second method is to use existing and future technologies to more easily tailor digital interventions to fit the cultural background and life circumstances of an individual or group. For instance, a digital depression intervention could be introduced in an urban-based health clinic that primarily serves African-Americans with diabetes. Digital interventions could allow practitioners or consumers to tailor visual images, clinical examples or educational material to fit the experiences of minority group members with a chronic illness. Future digital interventions would benefit from technology that would allow for simple tailoring of content without requiring extensive reprogramming and involvement of computer experts. Simple, low-cost methods to adjust digital interventions with respect to language, imagery, examples, etc. would greatly increase the reach of these interventions to underserved individuals across the globe. Certain groups may not have access to or may be not be inclined to use interventions found in a digital apothecary. However, recent data suggest that the digital divide is not as vast as it once was. A recent comprehensive survey of individuals from lower-income communities indicated that 85% of families below the poverty line have some kind of digital device, smartphone and/or tablet, in their household (68). Furthermore, 73% had one or more smartphones relative to 84% for families living above the poverty line. The accelerated growth curve of mobile devices across the socioeconomic spectrum is not only found in the US, but globally with 75% of the world estimated to have access to a mobile phone and 77% of mobile subscriptions located in poorer countries in 2010 (69,70). Thus, digital connectivity may be less of an issue than previously thought. Attitudes and comfort with digital interventions may be a bigger issue. This is an empirical question warranting further investigation.
In addition to the promise of digital interventions as a method to reduce disparities in terms of access, there is a possibility that the increasing availability of these interventions may have an unintended negative effect on the ongoing struggle to deploy well-trained interventionists into underserved areas. As we envision them, digital interventions are not intended to supplant face-to-face treatments for all individuals who need them. It is clear that for some individuals, face-to-face treatment from well-trained professionals is required. There is a risk that the proliferation of digital interventions may reduce urgency to close the unacceptable access gap with respect to face-to-face therapy for individuals living in underserved urban and rural areas. From a social justice perspective, it is critical that the benefits of providing evidence-based digital interventions to underserved individuals not overshadow the need to continue to push for access to the full-range of mental health treatment resources for all (71). As Isaac Marks and coauthors point out (71): “patients should get all the time, expertise, and individual attention they need, but not more.” Giving patients more consumable care than they need implies that others who need the care will not receive it.
Open questions and future directions
Many of us envision digital apothecaries that would make available evidence-based MOOIs (44), to anyone in the world at no charge. Those of us who share the goal to make health care a universal human right believe that having these tools accessible to all who need them is a goal worth pursuing. However, some in our group have pointed out that while the savings resulting from economies of scale of “non-consumable interventions” are real, our goal of free interventions does not take into account the costs involved in developing quality digital tools, updating them, adding new features, bug fixes, security fixes, obtaining and maintaining regulatory compliance, scaling servers and customer service, keeping content current with science, legal aspects, and oversight of data repositories. Nor does it yet provide a comprehensive model of the human supports needed to ensure effective engagement with the technologies and the associated costs as the model is expanded to accomplish widespread global delivery. In addition, driving ongoing engagement (“build it and they will come”—and actually use the websites or apps as intended) clearly is not the case with most interventions, except in very rare “hit it out of the park” game apps. Business models that will allow us to provide free digital interventions in our envisioned apothecaries have yet to be developed. Examples in other fields include such websites as Wikipedia and the Khan Academy.
Issues of privacy and ownership of health data are also of concern to us. Ideally, we would develop digital apothecaries that allow users to access the interventions anonymously. How to do so and still allow the sites to reach out to these users to reduce attrition is an unsolved problem. Email addresses and phone numbers for sending them texts automatically identify them. Methods to allow users who want their data deleted from the system should also be developed.
Similarly, issues of intellectual property need to be considered. Websites or apps can obtain traditional copyright protection. Alternatively, they can obtain a creative commons license, which specifies which parts of the website are available for re-use, as long as this is done without seeking commercial compensation. Proprietary websites or apps will certainly be part of the universe of digital interventions. They are likely to navigate the process of being approved for routine use in health care systems more often than open access digital interventions. The advantage of open access offerings in digital apothecaries is that they will be available to both those not served by health care systems and those within health care systems who choose to use them.
An important unanswered question concerns whether the samples tested in the trials that determined efficacy will correspond to the apothecary’s eventual end users. For instance, in some cases, trial participants are paid or the recruitment methods might result in sampling biases that would introduce other differences between trial participants and eventual end users. Given enough users, especially those of diverse characteristics, one might be able to explore this through moderation analyses which are urgently needed not just in digital interventions but mental health interventions more generally. However, there will always be a challenge to bring people to digital interventions who are not interested in such resources, so user interests and needs need to be considered at the design phase. We see these challenging issues as part of why a digital apothecary that includes transparent and dynamic (i.e., regularly updated) reporting of outcome data could be especially clinically useful. Unlike lengthy clinic-based trials, the apothecary can enroll participants rapidly and have the sample sizes to do moderator analyses, meaning that visitors to the apothecary can learn quickly and iteratively which subpopulations seem to benefit most from a given intervention. This may ultimately allow personalization and matching of interventions in a way that has not been possible thus far in the clinic.
Another interesting issue related to thresholds for inclusion concerns how to integrate cost-effectiveness data into the criteria. A key long-term goal will be conducting cost-effectiveness analyses that directly compare in-person to guided to fully independent interventions, and how those costs and benefits change as the interventions are scaled up. As evident in the United Kingdom’s NICE use of the “incremental cost-effectiveness ratio” to guide health care policy and treatment recommendation decisions, there are important real-world implications to decisions about cost-effectiveness thresholds. We do not believe the state of the literature is at the point where we have data on cost-effectiveness for enough interventions to use this as an initial inclusion criterion for the apothecary. However, we hope this will one day change; just as far more work is needed in the United States to evaluate cost-effectiveness of in-person mental health interventions, we hope that analogous attention will be paid to examining these issues in digital interventions.
Although the use of machine learning is an obvious next step, we are aware that “black box” algorithms can sometimes result in unintended discrimination against subgroups in the population (72,73). Several examples of such algorithms denying access to loans to minorities, or providing limited information to users because of their gender have recently been made public. We need to balance the potential benefits of deep learning and other such methods with human oversight to prevent negative effects on our society.
Conclusions
We envision the creation of digital apothecaries as a way to expand health service delivery globally. We believe such portals could contribute to the reduction in health disparities. In this article, we have listed many of the potential benefits, while also making sure that we do not assume that all outcomes of such a vision will result in positive outcomes. We want to make sure that we are on the lookout for unintended negative consequences. At the same time, we are aware that there may also be unintended positive consequences if we move in this direction. Increasing access to evidence-based interventions to people worldwide is a goal worth pursuing. We invite kindred spirits to contribute to actualizing this vision.
Acknowledgements
We would like to thank the Association for Behavioral and Cognitive Therapies for convening a Think Tank on “Digital CBT Technologies to Provide Care to Difficult-to-Reach and Underserved Populations” in San Diego, November 16, 2017. Most of the coauthors (with the exception of JI Ruzek) participated in the Think Tank and began discussing the ideas in this article at that venue.
Funding: This project was partially supported by funds provided by The Regents of the University of California, Tobacco-Related Diseases Research Program, Grant Number No. 24RT-0027 to RF Muñoz. The opinions, findings, and conclusions herein are those of the authors and not necessarily represent those of The Regents of the University of California, or any of its programs. It was also supported in part by NIMH Grant R01MH113752 to BA Teachman and by NIMH Grant R34MH109601 to DA Chavira. SM Schueller receives funding from One Mind to direct and lead PsyberGuide. SM Schueller is an investigator with the Implementation Research Institute (IRI), at the George Washington University in St. Louis; through an award from the National Institute of Mental Health (5R25MH08091607) and the Department of Veterans Affairs, Health Services Research & Development Service, Quality Enhancement Research Initiative (QUERI).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Neary M, Schueller SM. State of the field of mental health apps. Cogn Behav Pract 2018. [Epub ahead of print]. [Crossref]
- Mohr DC, Weingardt KR, Reddy M, et al. Three problems with current digital mental health research and three things we can do about them. Psychiatr Serv 2017;68:427-9. [Crossref] [PubMed]
- Karyotaki E, Riper H, Twisk J, et al. Efficacy of Self-guided Internet-Based Cognitive Behavioral Therapy in the Treatment of Depressive Symptoms: A Meta-analysis of Individual Participant Data. JAMA Psychiatry 2017;74:351-9. [Crossref] [PubMed]
- Andersson G. Internet-Delivered Psychological Treatments. Annu Rev Clin Psychol 2016;12:157-79. [Crossref] [PubMed]
- Hedman E, Ljotsson B, Lindefors N. Cognitive behavior therapy via the Internet: a systematic review of applications, clinical efficacy and cost-effectiveness. Expert Rev Pharmacoecon Outcomes Res 2012;12:745-64. [Crossref] [PubMed]
- Ebert DD, Donkin L, Andersson G, et al. Does Internet-based guided-self-help for depression cause harm? An individual participant data meta-analysis on deterioration rates and its moderators in randomized controlled trials. Psychol Med 2016;46:2679-93. [Crossref] [PubMed]
- Buntrock C, Ebert DD, Lehr D, et al. Effect of a Web-Based Guided Self-help Intervention for Prevention of Major Depression in Adults With Subthreshold Depression: A Randomized Clinical Trial. JAMA 2016;315:1854-63. [Crossref] [PubMed]
- Muñoz RF. The efficiency model of support and the creation of digital apothecaries. Clin Psy Sci Pract 2017;24:46-9. [Crossref]
- Christensen H, Murray K, Calear AL, et al. Beacon: a web portal to high-quality mental health websites for use by health professionals and the public. Med J Aust 2010;192:S40-4. [PubMed]
- Wentzel J, van der Vaart R, Bohlmeijer ET, et al. Mixing Online and Face-to-Face Therapy: How to Benefit From Blended Care in Mental Health Care. JMIR Ment Health 2016;3:e9. [Crossref] [PubMed]
- Riper H, Blankers M, Hadiwijaya H, et al. Effectiveness of guided and unguided low-intensity internet interventions for adult alcohol misuse: a meta-analysis. PLoS One 2014;9:e99912. [Crossref] [PubMed]
- Mohr DC, Cheung K, Schueller SM, et al. Continuous evaluation of evolving behavioral intervention technologies. Am J Prev Med 2013;45:517-23. [Crossref] [PubMed]
- Patrick K, Hekler EB, Estrin D, et al. Rapid Rate of Technological Development and Its Implications for Research on Digital Health Interventions. Am J Prev Med 2016. [Epub ahead of print].
- Steinberg E, Greenfield S, Wolman DM, et al. editors. Clinical practice guidelines we can trust. National Academies Press, 2011.
- Hollon SD, Arean PA, Craske MG, et al. Development of clinical practice guidelines. Annu Rev Clin Psychol 2014;10:213-41. [Crossref] [PubMed]
- Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol 1998;66:7-18. [Crossref] [PubMed]
- Proudfoot J, Klein B, Barak A, et al. Establishing guidelines for executing and reporting Internet intervention research. Cogn Behav Ther 2011;40:82-97. [Crossref] [PubMed]
- Rozenthal A, Andersson G, Boettcher J, et al. Consensus statement on defining and measuring negative effects of Internet interventions. Internet Interv 2014;1:12-9. [Crossref]
- Titov N, Dear BF, Staples LG, et al. The first 30 months of the MindSpot Clinic: Evaluation of a national e-mental health service against project objectives. Aust N Z J Psychiatry 2017;51:1227-39. [Crossref] [PubMed]
- Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013;46:81-95. [Crossref] [PubMed]
- Crane D, Garnett C, Brown J, et al. Behavior change techniques in popular alcohol reduction apps: content analysis. J Med Internet Res 2015;17:e118. [Crossref] [PubMed]
- Cook L, Watkins E. Guided, internet-based, rumination-focused cognitive behavioural therapy (i-RFCBT) versus a no-intervention control to prevent depression in high-ruminating young adults, along with an adjunct assessment of the feasibility of unguided i-RFCBT, in the REducing Stress and Preventing Depression trial (RESPOND): study protocol for a phase III randomised controlled trial. Trials 2016;17:1. [Crossref] [PubMed]
- Ritterband LM, Thorndike FP, Ingersoll KS, et al. Effect of a Web-Based Cognitive Behavior Therapy for Insomnia Intervention With 1-Year Follow-up: A Randomized Clinical Trial. JAMA Psychiatry 2017;74:68-75. [Crossref] [PubMed]
- Rozental A, Forsell E, Svensson A, et al. Overcoming procrastination: one-year follow-up and predictors of change in a randomized controlled trial of Internet-based cognitive behavior therapy. Cogn Behav Ther 2017;46:177-95. [PubMed]
- Doss BD, Cicila LN, Georgia EJ, et al. A randomized controlled trial of the web-based OurRelationship program: Effects on relationship and individual functioning. J Consult Clin Psychol 2016;84:285-96. [Crossref] [PubMed]
- Newby JM, Twomey C, Yuan Li SS, et al. Transdiagnostic computerised cognitive behavioural therapy for depression and anxiety: A systematic review and meta-analysis. J Affect Disord 2016;199:30-41. [Crossref] [PubMed]
- Mohr DC, Tomasino KN, Lattie EG, et al. IntelliCare: An Eclectic, Skills-Based App Suite for the Treatment of Depression and Anxiety. J Med Internet Res 2017;19:e10. [Crossref] [PubMed]
- Barlow DH, Farchione TJ, Bullis JR, et al. The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders Compared With Diagnosis-Specific Protocols for Anxiety Disorders: A Randomized Clinical Trial. JAMA Psychiatry 2017;74:875-84. [Crossref] [PubMed]
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: a distillation and matching model. Ment Health Serv Res 2005;7:5-20. [Crossref] [PubMed]
- Embry DD, Biglan A. Evidence-based kernels: fundamental units of behavioral influence. Clin Child Fam Psychol Rev 2008;11:75-113. [Crossref] [PubMed]
- Muñoz RF, Aguilera A, Schueller SM, et al. From online randomized controlled trials to participant preference studies: morphing the San Francisco Stop Smoking site into a worldwide smoking cessation resource. J Med Internet Res 2012;14:e64. [Crossref] [PubMed]
- Perlis RH, Iosifescu DV, Castro VM, et al. Using electronic medical records to enable large-scale studies in psychiatry: treatment resistant depression as a model. Psychol Med 2012;42:41-50. [Crossref] [PubMed]
- Bruehlman-Senecal E, Aguilera A, Schueller SM. Mobile Phone-Based Mood Ratings Prospectively Predict Psychotherapy Attendance. Behav Ther 2017;48:614-23. [Crossref] [PubMed]
- Litvin EB, Abrantes AM, Brown RA. Computer and mobile technology-based interventions for substance use disorders: an organizing framework. Addict Behav 2013;38:1747-56. [Crossref] [PubMed]
- Dubad M, Winsper C, Meyer C, et al. A systematic review of the psychometric properties, usability and clinical impacts of mobile mood-monitoring applications in young people. Psychol Med 2018;48:208-28. [Crossref] [PubMed]
- Sliwinski MJ, Mogle JA, Hyun J, et al. Reliability and Validity of Ambulatory Cognitive Assessments. Assessment 2018;25:14-30. [Crossref] [PubMed]
- Carpenter RW, Wycoff AM, Trull TJ. Ambulatory Assessment: New Adventures in Characterizing Dynamic Processes. Assessment 2016;23:414-24. [Crossref] [PubMed]
- Mohr DC, Ho J, Duffecy J, et al. Perceived barriers to psychological treatments and their relationship to depression. J Clin Psychol 2010;66:394-409. [PubMed]
- Roepke AM, Jaffee SR, Riffle OM, et al. Randomized Controlled Trial of SuperBetter, a Smartphone-Based/Internet-Based Self-Help Tool to Reduce Depressive Symptoms. Games Health J 2015;4:235-46. [Crossref] [PubMed]
- Birney AJ, Gunn R, Russell JK, et al. MoodHacker Mobile Web App With Email for Adults to Self-Manage Mild-to-Moderate Depression: Randomized Controlled Trial. JMIR Mhealth Uhealth 2016;4:e8. [Crossref] [PubMed]
- Rose RD, Buckey JC Jr, Zbozinek TD, et al. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behav Res Ther 2013;51:106-12. [Crossref] [PubMed]
- Ruzek JI, Yeager CM. Internet and phone technologies: Addressing the mental health of trauma survivors in less resourced communities. Glob Ment Health (Camb) 2017;4:e16. [Crossref] [PubMed]
- Ruzek JI, Kuhn E, Jaworski BK, et al. Mobile mental health interventions following war and disaster. Mhealth 2016;2:37. [PubMed]
- Muñoz RF, Bunge EL, Chen K, et al. Massive open online interventions: A novel model for delivering behavioral health services worldwide. Clin Psychol Sci 2015;4:194-205. [Crossref]
- Chavira DA, Bustos CE, Garcia MS, et al. Delivering CBT to Rural Latino Children with Anxiety Disorders: A Qualitative Study. Community Ment Health J 2017;53:53-61. [Crossref] [PubMed]
- Pyne JM, Fortney JC, Tripathi SP, et al. Cost-effectiveness analysis of a rural telemedicine collaborative care intervention for depression. Arch Gen Psychiatry 2010;67:812-21. [Crossref] [PubMed]
- Wang Z, Wang J, Maercker A. Chinese My Trauma Recovery, a Web-based intervention for traumatized persons in two parallel samples: randomized controlled trial. J Med Internet Res 2013;15:e213. [Crossref] [PubMed]
- Knaevelsrud C, Brand J, Lange A, et al. Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: randomized controlled trial. J Med Internet Res 2015;17:e71. [Crossref] [PubMed]
- Barrera AZ, Wickham RE, Muñoz RF. Online prevention of postpartum depression for Spanish- and English-speaking pregnant women: A pilot randomized controlled trial. Internet Interv 2015;2:257-65. [Crossref] [PubMed]
- Pratap A, Anguera JA, Renn BN, et al. The feasibility of using smartphones to assess and remediate depression in Hispanic/Latino individuals nationally. 2017 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2017 ACM International Symposium on Wearable Computers ACM, 2017:854-60.
- Muroff J, Robinson W, Chassler D, et al. Use of a Smartphone Recovery Tool for Latinos with Co-Occurring Alcohol and Other Drug Disorders and Mental Disorders. J Dual Diagn 2017;13:280-90. [Crossref] [PubMed]
- Kaltenthaler E, Brazier J, De Nigris E, et al. Computerised cognitive behaviour therapy for depression and anxiety update: a systematic review and economic evaluation. Health Technol Assess 2006;10:xi-xiv, 1-168. [PubMed]
- Spek V, Cuijpers P, Nyklicek I, et al. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med 2007;37:319-28. [Crossref] [PubMed]
- Collins PY, Patel V, Joestl SS, et al. Grand challenges in global mental health. Nature 2011;475:27-30. [Crossref] [PubMed]
- Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med 2013;97:82-6. [Crossref] [PubMed]
- Bone D, Chaspari T, Audkhasi K, et al. Classifying Language-Related Developmental Disorders from Speech Cues: the Promise and the Potential Confounds. 14th Annual Conference of the International Speech Communication Association (Interspeech 2013), 2013:182-6.
- Torous J, Baker JT. Why Psychiatry Needs Data Science and Data Science Needs Psychiatry: Connecting With Technology. JAMA Psychiatry 2016;73:3-4. [Crossref] [PubMed]
- Chekroud AM. Bigger Data, Harder Questions-Opportunities Throughout Mental Health Care. JAMA Psychiatry 2017;74:1183-4. [Crossref] [PubMed]
- Luxton DD. Artificial intelligence in behavioral and mental health care. London: Academic Press, 2016.
- Vergyri D, Knoth B, Shriberg E, et al. Speech-based assessment of PTSD in a military population using diverse features classes. Proceedings of the Annual Conference of the International Speech Communication Association, 2015.
- Acion L, Kelmansky D, van der Laan M, et al. Use of a machine learning framework to predict substance use disorder treatment success. PLoS One 2017;12:e0175383. [Crossref] [PubMed]
- Fridsma DB. AMIA Response to FCC Notice on Accelerating Broadband Health Tech Availability. American Medical Informatics Association (AMIA), 2017. Available online: www.amia.org/public-policy/
- Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: Examples from parent training. Clin Psychol (New York) 2006;13:295-310.
- Bernal G, Saez-Santiago E. Culturally centered psychosocial interventions. J Community Psychol 2006;34:121-32. [Crossref]
- Chowdhary N, Jotheeswaran AT, Nadkarni A, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorder: A systematic review. Psychol Med 2014;44:1131-46. [Crossref] [PubMed]
- Bolton P, Lee C, Haroz EE, et al. A transdiagnostic community-based mental health treatment for comorbid disorders: development and outcomes of a randomized controlled trial among Burmese refugees in Thailand. PLoS Med 2014;11:e1001757. [Crossref] [PubMed]
- MacLeod C, Mathews A. Cognitive bias modification approaches to anxiety. Annu Rev Clin Psychol 2012;8:189-217. [Crossref] [PubMed]
- Rideout V, Katz VS. Opportunity for all? Technology and learning in lower-income families. A report of the Families and Media Project. New York: Joan Ganz Cooney Center at Sesame Workshop, 2016.
- Farrington C, Aristidou A, Ruggeri K. mHealth and global health: still waiting for the mH2 wedding? Global Health 2014;10:17. [Crossref] [PubMed]
- Bank W. Information and Communications for Development: Maximizing Mobile. Washington, DC: World Bank, 2012.
- Marks IM, Cavanagh K, Gega L. Hands-on help: Computer-aided psychotherapy. New York, NY: Taylor & Francis, 2007.
- Eubanks V. Automating Inequality: How High-Tech Tools Profile, Police, and Punish the Poor. New York, NY: St. Martin’s Press, 2018.
- Noble SU. Algorithms of Oppression: How search engines reinforce racism. New York, NY: New York University Press, 2018.
Cite this article as: Muñoz RF, Chavira DA, Himle JA, Koerner K, Muroff J, Reynolds J, Rose RD, Ruzek JI, Teachman BA, Schueller SM. Digital apothecaries: a vision for making health care interventions accessible worldwide. mHealth 2018;4:18.