A comparison between paper-based and m-Health tools for collating and reporting clinical cases of lymphatic filariasis and podoconiosis in Ethiopia
Introduction
Lymphatic filariasis (LF) and podoconiosis are neglected tropical diseases (NTDs) endemic to Ethiopia which cause chronic and debilitating swelling of the limbs. In podoconiosis (non-filarial lymphoedema), the swelling is primarily of the lower limbs and is caused by chronic long-term exposure to irritant red clay soils (1). Conversely, LF is a mosquito-borne parasitic disease, caused by Wuchereria bancrofti in Ethiopia, which can lead to hydrocoele (scrotal swelling) and lymphoedema; the latter most commonly of the leg but also the arms, breast and genital organs (2).
The debilitating chronic conditions caused by both LF and podoconiosis can result in an enormously complex range of physical, social, economic and psychological hardships. In Ethiopia, it is estimated that podoconiosis patients lose 45% of total working days per year (3) and suffer from discrimination and prejudice so severe that over 50% of the patients consider suicide (4). Similarly, for LF, studies in Malawi have shown that those affected by LF lymphoedema experience a lower quality of life as confirmed by both subjective and objective mobility measures, and a lower income, in comparison to their unaffected peers (5). Earlier studies in Haiti and Ghana have also shown that the risk of dysfunction and unhappiness is greater in marriages where the female partner was the one who had the physical manifestations of LF (6,7). With an estimated 36 million people worldwide thought to be disfigured by LF (8) and an estimated 4 million cases of podoconiosis worldwide (9-11), a rapid and cost-effective tool may be a valuable method of obtaining clinical cases estimates.
In Ethiopia, there are 70 LF endemic woredas (districts), 345 podoconiosis endemic districts, and 29 co-endemic districts (12). With geographical overlap of both diseases, and a similar clinical presentation of lymphoedema, the Federal Ministry of Health (FMOH) promotes integrated morbidity management and disability prevention (MMDP) services for LF and podoconiosis patients. Such MMDP services aim to provide access to basic recommended care for all people with lymphoedema, as required by the Global Programme to Eliminate LF (GPELF) (2). This includes simple hygiene measures such as basic skin care to prevent acute attacks (acute inflammatory episodes) and to prevent progression of lymphoedema to elephantiasis (hardening and thickening of the skin), as well as psychological and socio-economic support to ensure all clinical cases have equal opportunities for health, education and income (2). Hydrocoele patients should have access to safe surgery (2). As a pre-requisite to equitable and accessible patient care, information on the number of patients (lymphoedema and hydrocoele) in each implementation unit (IU) or similar health administrative unit is essential and part of the World Health Organisation (WHO) dossier requirements (13,14).
In Ethiopia, health extension workers (HEWs) are at the frontline of community-based preventative and curative services. HEWs are largely female, salaried employees of the FMOH, who are recruited from their local community and trained to deliver sixteen packages of care focussed on family health, disease prevention and control, and hygiene and environmental sanitation (15,16). Working at the community-level, with an average of two HEWs per health post, together serving an average population of 5,000 individuals (16), HEWs play a crucial role in the delivery and uptake of services and represent an important opportunity for gathering information directly from local communities.
As part of their support to the LF Programme at the FMOH in Ethiopia, the Centre of Neglected Tropical Diseases (CNTD) at the Liverpool School of Tropical Medicine (LSTM) supported a morbidity burden assessment by HEWs in twenty LF and podoconiosis co-endemic districts in the Southern Nations, Nationalities, and Peoples’ Region (SNNPR) and Amhara Region in collaboration with the National Podoconiosis Action Network (NaPAN) (17). This study was conducted using a standard paper-based method of data collection which can be both time consuming and costly. With the rapid increase in mobile phone usage and accessibility across the world, mHealth approaches offer an exciting alternative to the standard, paper-based patient identification to provide real-time validated data for prompt response and delivery of MMDP services (18,19).
The SMS mHealth tool ‘MeasureSMS-Morbidity’ has been developed by the CNTD, and is used to collate and report morbidity information, collected by community health workers, including lymphoedema and hydrocoele cases at the village and health post level (20,21). Therefore, to pilot the feasibility of using this mHealth tool in Ethiopia and to compare its utility with the standard, paper-based method of reporting patients, a study of the ‘MeasureSMS-Morbidity’ tool was conducted concurrently in two districts with the paper-based burden assessment study (17).
Methods
Study site characteristics
The pilot study was conducted in Bensa and Hawella Tula districts of SNNPR. SNNPR is administratively divided into nine zones and 77 districts, and has borders with Kenya in the South, the Republic of Sudan in the South-West and the Ethiopian regional states of the Gambella Peoples’ in the North-West and Oromia in the North and East. Bensa and Hawella Tula are both located in the Sidama zone of SNNPR. The population of Bensa and Hawella Tula districts are 307,878 (50.6% male) and 152,844 (50.4% male); respectively (22,23).
Study design and tools
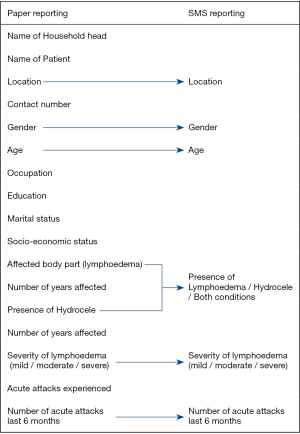
The community-based cross-sectional survey was conducted over a ten-day period using HEWs to identify all cases of lymphoedema and hydrocoele (17). A household registration form was completed to ensure all households and kebeles (the smallest administrative unit of Ethiopia) were covered in each district. If a patient was identified, a paper-based standard patient information collection form was used to record patient information by the HEWs. This included general demographic information such as the name, age, gender, location (i.e., kebele), occupation, education, marital and socio-economic status of the patient. It also included clinical information such as the condition (lymphoedema, hydrocoele or both conditions), affected body part of the lymphoedema swelling, number of years affected by condition, severity of condition, experience and number of acute attacks in the last six months. As LF and podoconiosis have different methods of staging the severity of lymphoedema (24,25), for simplicity, the HEWs staged lymphoedema severity as either mild, moderate or severe using the pictorial depiction shown in Figure 1, and did not stage hydrocoele.
To pilot the feasibility of MeasureSMS-Morbidity as a reporting tool, following the completion of the standard paper-based patient identification form, selected information was transferred to a SMS reporting form, including the location (i.e., kebele), gender, age, condition, severity of condition and number of acute attacks in the last six months (Figure 2). HEWs were instructed to send this information by SMS using their own mobile phones, and were provided with enough airtime to cover the cost. The MeasureSMS-Morbidity tool was able to validate the data reported by SMS by sending an automated response to the data reporter (i.e., the HEW) indicating whether or not the message had been sent in the correct format (20). The tool also allowed the rapid collation of data, which was accessible via a web browser and could be monitored in real-time.
Training
One HEW per kebele and two district health office staff per district attended the one-day training session. The training was conducted in the local language by country-based collaborators, with the support of staff from the collaborating institute (CNTD, LSTM). The attendees were trained on: (I) different causes and forms of lymphedema and staging lymphedema; (II) identifying people affected by lymphoedema (both LF and podoconiosis) and hydrocoele; (III) recording patient information on paper forms; (IV) transferring selected information onto the SMS reporting forms; (V) reporting information by SMS (including practical exercises); and (VI) advising patients on managing their condition, including health centre referrals. All written training material was provided in the local language.
Data collection and analysis
In the days following the training, the HEWs returned to their respective catchment areas to identify all people affected by lymphoedema and hydrocoele. The two health office staff per district were responsible for overseeing the data collection, and acting as a point of contact if any problems were encountered. The paper-based standard patient information forms were collected at the end of the activity, and collated at central level. The SMS reports received were monitored via the MeasureSMS-morbidity server web browser in real-time by a central level supervising team, allowing any data reporting inaccuracies to be identified and rectified immediately.
The data recorded on the paper-based forms were entered into Microsoft Excel Version 12.3.6 (Microsoft Corp., Redmond, VA, USA), and the data from the SMS reporting were downloaded from the web browser. To compare the reported cases by each method, both datasets were disaggregated by gender, condition, severity of condition, and analysed for trends using IBM SPSS Statistics 32 (IBM Corp., Armonk, NY, USA). The Chi-squared test (P value >0.005 significant) was calculated to determine whether there was a significant difference between the reporting methods for the total cases reported and each condition (lymphoedema, hydrocoele and both). Prevalence estimates (per 10,000 total population) for each condition were also calculated from population estimates (22,23).
In addition, the kebeles in each district were ranked based on the highest to lowest number of lymphoedema, hydrocoele and total cases reported to identify if a similar ranking was observed for both reporting methods, which has important implications in the prioritisation of resources. Further, to examine the association between the paper-based and SMS ranking order of each kebele, the Pearson’s product-moment correlation was used with a range from −1 (negative association) to +1 (positive association) and correlations being significant at the 0.01 level (two-tailed).
In addition, the overall costs of the two methods were compared. Costs were compared for all elements from training, data collection and data entry and included the following cost areas: printing; training; fieldwork; supervision; data collection; collecting the completed paper based forms; data entry; phone purchase and credit. Additionally, human resource implications were also considered.
Results
Summary of reported data
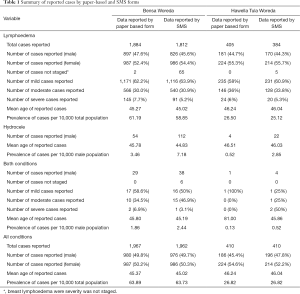
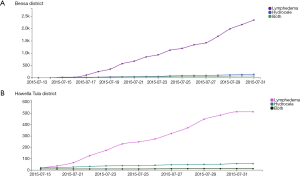
In total, 59 HEWs (40 from Bensa, 19 from Hawella Tula) and four district health office staff were trained on patient identification and reporting. The data collection period was completed within ten days in July 2015, with one HEW reporting per kebele. Table 1 presents the number of cases of each condition reported for both districts, aggregated by gender and severity (for lymphoedema only). In total, 2,377 clinical cases were reported by the paper-based form and 2,372 clinical cases by SMS in both districts. Of these, 96% (2,289/2,377) of paper-based reported cases and 93% (2,196/2,372) of SMS reported cases were lymphoedema. A summary of the daily cumulative responses reported by SMS and received by the online server for Bensa and Hawella Tula are shown in Figure 3.
Full table
Data reported from Bensa district
For all conditions reported in Bensa, five additional cases were reported by the paper-based forms (n=1,967) in 38 kebeles, compared to by SMS (n=1,962) in 39 kebeles, however the difference in the total number of cases reported was not significant (P=0.936). For both reporting methods, the mean age of reported cases was 45 years with a prevalence of 64 per 10,000 of total population. Additionally, for both reporting methods, the gender of reported cases was equally 50% male and 50% female.
When comparing the number of cases of each condition reported by the two methods of reporting (lymphoedema, hydrocoele or both) there were no significant differences in the number of lymphoedema cases (P=0.235), and patients with both conditions (P=0.271). Significant differences were observed in reported cases of hydrocoele, with over twice as many cases of hydrocoele reported by SMS (n=112) than by the paper-based forms (n=54) (P<0.001) (Table 1).
Data reported from Hawella Tula district
For Hawella Tula, the total number of all cases reported in the 19 kebeles was the same for both reporting methods (n=410), with 52% (214/410) of cases reported by SMS and 55% (224/410) of cases reported by the paper-based method being female. For both reporting methods, the mean age of reported cases was 46 years with a prevalence of 27 per 10,000 of the total population.
When comparing the number of cases of each condition reported by the two methods of reporting, the difference observed was not statistically significant for lymphoedema (P=0.3454) or both conditions (P=0.180). When comparing hydrocoele cases reported, over five times as many hydrocoele cases were reported by SMS (n=22) than by the paper-based forms (n=4) (P<0.001) (Table 1).
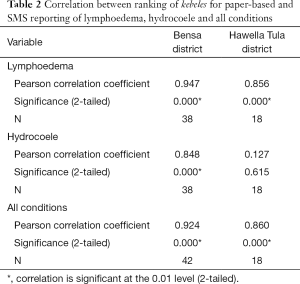
Ranking of sub-district (kebeles)
In Bensa, a significant positive correlation was found between paper-based and SMS reporting methods for the total reported cases (r=0.924, n=42, P<0.01), lymphoedema cases (r=0.947, n=38, P<0.01), and hydrocoele cases (r=0.848, n=38, P<0.01) (Table 2). In Hawella Tula, a significant positive correlation was found for the total reported cases (r=0.860, n=18, P<0.01) and lymphoedema cases (r=0.856, n=18, P<0.01) (Table 2). For hydrocoele cases, the rank correlation was weak and not significant (r=0.127, n=18, P=0.615) (Table 2).
Full table
The rankings of the total number of all cases reported per kebele in Bensa, found that seven of the 36 kebeles remain in the top rankings for both the paper-based and SMS report rankings. Similarly, the same seven kebeles were found in the top ranking when considering only lymphoedema cases, while for only hydrocoele cases, five kebeles were found in the top ranking.
The rankings of the total number of all reported cases per kebele in Hawella Tula, found that four of the 18 kebeles remain in the top rankings for both paper-based and SMS reporting, and six kebeles remain in the top rankings for lymphoedema only. Due to the low number of hydrocoele cases reported in Hawella Tula, the ranking for only hydrocoele cases shows no clear trend in this district.
Cost comparison
For both methods of data reporting, the costs such as the training of HEWs, fieldwork costs (per diem for patient searching), district-level supervision and central-level support remain the same regardless of the reporting method used. The additional costs associated with paper-based reporting are the printing of the data collection tools, the physical collection of the paper forms and manual data entry. These costs are not required for SMS-based reporting, however, additional costs related to the SMS reporting are the purchasing of SMS credit for HEWs and supervisors, and the purchasing of two phones to act as MeasureSMS server phones (one phone per district) and SMS credit for both server phones. A summary of the costs associated costs with both methods of reporting are shown in Figure 4.
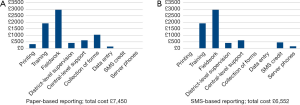
The total cost of paper-based reporting (£7,450) was 13.7% more expensive than the SMS-based reporting (£6,552). This is largely due to the costs associated with data collection and data entry. For SMS reporting, no physical collection or collation of data was required as this was done automatically via the MeasureSMS-morbidity server meaning that the results were available immediately after the five-day data reporting period. However, unanticipated challenges including network issues and power ‘black-outs’ lasting several days occuring during the reporting period. These issues left HEWs unable to charge their phones and send the SMS for periods of time during the survey. For the paper-based data entry, it took two staff six days to collect the forms from the two districts and further time to double-enter the data from the paper-based forms.
Discussion
This study highlights the value of the use of the MeasureSMS reporting tool to report clinical cases of LF and podoconiosis. When comparing the total cases reported, lymphoedema and both, the two reporting methods showed no significant difference. Similarly, the ranking and correlation shows that the kebeles with the highest burden of lymphoedema - the top seven highest burden kebeles in Bensa, and the top six highest burden kebeles in Hawella Tula - remain the same for both reporting methods. For hydrocoele, despite significant differences in the total number of cases reported in both districts, the top six highest burden kebeles remain the same for both reporting methods in Bensa, however due to the low prevalence in Hawella Tula, the ranking showed no clear trend.
As the areas with the highest burden of disease would be prioritised for MMDP services, these results show that both reporting methods allow the identification of the highest burden kebeles, meaning that limited resources would be targeted in the same way. This is particularly important for lymphoedema services in which the basic package of managing lymphoedema is traditionally delivered at the community level with support from HEWs, where sub-district prioritisation is essential for delivery of accessible services; unlike hydrocoele surgery which is performed at district-level hospitals (2).
Following on from experiences of using the MeasureSMS-morbidity mHealth tool in Malawi, Ghana and Tanzania (21,26), new challenges were observed in Ethiopia such as network issues and power ‘black-outs’ lasting several days which left HEWs unable to charge their phones and send the SMS. Also, unlike previous studies in Malawi where 96% of data reporters stated that they did not have any difficulty in submitting data by SMS (21), a higher proportion of HEWs in Ethiopia had problems sending the data via SMS. To overcome these issues in future deployments of mHealth tools for NTD activities in Ethiopia, it would be recommended to employ a ‘two-tier’ reporting system in which HEWs collect the patient data, but the data itself is collated and reported by SMS at the health-facility level by a more senior health worker (27). This approach has been successfully used in a large urban area of Tanzania (26), and would help reduce the risk of community health workers losing confidence in the SMS reporting system when faced with challenges, the negative implications of which could be under-reporting.
Although challenges were encountered sending the data via SMS, the mHealth tool allowed the rapid collation of data throughout the activity, allowing easier monitoring and supervision of data reporting from anywhere in the world. On the other hand, the paper-based forms, although allowing more information to be collected, required manual collection and collation which required greater human and financial resources.
Conclusions
In summary, this study highlights the first pilot of mHealth tools for integrated NTD MMDP case reporting in Ethiopia. Notwithstanding some the phone network challenges, the SMS reporting tool was shown to be an equitable, time- and cost-effective reporting tool to enable resources to be allocated to those most in need quickly, and at low cost.
Acknowledgements
The authors acknowledge the fieldwork team in Ethiopia, including the health extension workers (HEWs) involved in the study for their assistance in locating the cases. The authors also gratefully acknowledge the cases who agreed to participate in the study. This work was supported by a grant from the UK Department for International Development to the Centre for Neglected Tropical Diseases, Liverpool School of Tropical Medicine for the Lymphatic Filariasis Elimination Programme.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval for this study was obtained from the Research Ethics Committee at the Liverpool School of Tropical Medicine, UK, and the Amhara and SNNP Regional Health Bureaus in Ethiopia. Informed consent was obtained from all household heads and patients involved in the study.
References
- Price EW, Plant DA. The significance of particle size of soils as a risk factor in the etiology of podoconiosis. Trans R Soc Trop Med Hyg 1990;84:885-6. [Crossref] [PubMed]
- WHO. Lymphatic Filariasis: managing morbidity and preventing disability. An aide-mémoire for national programmes managers. 2013.
- Tekola F, Mariam DH, Davey G. Economic costs of endemic non-filarial elephantiasis in Wolaita Zone, Ethiopia. Trop Med Int Health 2006;11:1136-44. [Crossref] [PubMed]
- Tora A, Franklin H, Deribe K, et al. Extent of podoconiosis-related stigma in Wolaita Zone, Southern Ethiopia: a cross-sectional study. Springerplus 2014;3:647. [Crossref] [PubMed]
- Stanton MC, Yamauchi M, Mkwanda SZ, et al. Measuring the physical and economic impact of filarial lymphoedema in Chikwawa district, Malawi: a case-control study. Infect Dis Poverty 2017;6:28. [Crossref] [PubMed]
- Coreil J, Mayard G, Louis-Charles J, et al. Filarial elephantiasis among Haitian women: social context and behavioural factors in treatment. Trop Med Int Health 1998;3:467-73. [Crossref] [PubMed]
- Gyapong M, Gyapong JO, Adjei S, et al. Filariasis in northern Ghana: some cultural beliefs and practices and their implications for disease control. Soc Sci Med 1996;43:235-42. [Crossref] [PubMed]
- Ramaiah KD, Ottesen EA. Progress and impact of 13 years of the global programme to eliminate lymphatic filariasis on reducing the burden of filarial disease. PLoS Negl Trop Dis 2014;8. [Crossref] [PubMed]
- Davey G, Tekola F, Newport MJ. Podoconiosis: non-infectious geochemical elephantiasis. Trans R Soc Trop Med Hyg 2007;101:1175-80. [Crossref] [PubMed]
- Tekola Ayele F, Adeyemo A, Finan C, et al. HLA class II locus and susceptibility to podoconiosis. N Engl J Med 2012;366:1200-8. [Crossref] [PubMed]
- Deribe K, Wanji S, Shafi O, et al. Measuring elimination of podoconiosis, endemicity classifications, case definition and targets: an international Delphi exercise. Int Health 2015;7:306-16. [Crossref] [PubMed]
- Mengistu B, Deribe K, Kebede F, et al. The National Programme to Eliminate Lymphatic Filariasis from Ethiopia. Ethiop Med J 2017;55:45-54. [PubMed]
- WHO. 489 Global programme to eliminate lymphatic filariasis: progress report, 2014. Wkly Epidemiol Rec 2015;90:489-504. [PubMed]
- WHO. Validation of elimination of lymphatic filariasis as a public health problem. 2017.
- Medhanyie A, Spigt M, Kifle Y, et al. The role of health extension workers in improving the utilization of maternal health services in rural areas in Ethiopia: a cross sectional study. BMC Health Serv Res 2012;12:352. [Crossref] [PubMed]
- Mangham-Jefferies L, Mathewos B, Russell J, et al. How do health extension workers in Ethiopia allocate their time? Hum Resour Health 2014;12:61. [Crossref] [PubMed]
- Kebede B, Martindale S, Mengistu B, et al. Integrated morbidity mapping of lymphatic filariasis and podoconiosis cases in 20 co-endemic districts of Ethiopia. PLoS Negl Trop Dis 2018;12. [Crossref] [PubMed]
- Brinkel J, Kramer A, Krumkamp R, et al. Mobile phone-based mHealth approaches for public health surveillance in sub-Saharan Africa: a systematic review. Int J Environ Res Public Health 2014;11:11559-82. [Crossref] [PubMed]
- Piette JD, Lun KC, Moura LA Jr, et al. Impacts of e-health on the outcomes of care in low- and middle-income countries: where do we go from here? Bull World Health Organ 2012;90:365-72. [Crossref] [PubMed]
- Stanton M, Molineux A, Mackenzie C, et al. Mobile Technology for Empowering Health Workers in Underserved Communities: New Approaches to Facilitate the Elimination of Neglected Tropical Diseases. JMIR Public Health Surveill 2016;2. [Crossref] [PubMed]
- Stanton MC, Mkwanda SZ, Debrah AY, et al. Developing a community-led SMS reporting tool for the rapid assessment of lymphatic filariasis morbidity burden: case studies from Malawi and Ghana. BMC Infect Dis 2015;15:214. [Crossref] [PubMed]
- Ethiopia CSAo. Population and Housing Census Report-Country 2007.
- Bank W. Ethiopia population growth (annual %). 2016. Available online: http://data.worldbank.org/indicator/SP.POP.GROW?locations=ET
- McPherson T, Fay MP, Singh S, et al. Health workers' agreement in clinical description of filarial lymphedema. Am J Trop Med Hyg 2006;74:500-4. [Crossref] [PubMed]
- Tekola F, Ayele Z, Mariam DH, et al. Development and testing of a de novo clinical staging system for podoconiosis (endemic non-filarial elephantiasis). Trop Med Int Health 2008;13:1277-83. [Crossref] [PubMed]
- Mwingira U, Chikawe M, Mandara WL, et al. Lymphatic filariasis patient identification in a large urban area of Tanzania: An application of a community-led mHealth system. PLoS Negl Trop Dis 2017;11. [Crossref] [PubMed]
- Mableson HE, Martindale S, Stanton MC, et al. Community-based field implementation scenarios of a short message service reporting tool for lymphatic filariasis case estimates in Africa and Asia. Mhealth 2017;3:28. [Crossref] [PubMed]
Cite this article as: Martindale S, Mableson HE, Kebede B, Kiros FH, Tamiru A, Mengistu B, Krueger A, Mackenzie CD, Kelly-Hope LA. A comparison between paper-based and m-Health tools for collating and reporting clinical cases of lymphatic filariasis and podoconiosis in Ethiopia. mHealth 2018;4:49.