
Telemedicine utilization by providers in accountable care organizations
Accountable care organizations (ACOs) aim to improve healthcare quality and reduce spending. Telemedicine, or the remote delivery of healthcare services using a variety of telecommunications devices, offers the potential to advance these goals by expanding patients’ timely access to care, reducing costs, and enabling better coordination of care among providers and care settings (1). Recognizing the potential value telemedicine offers to ACOs, the Centers for Medicare & Medicaid Services (CMS) provided fraud and abuse waivers protecting ACO participants who share in the costs of telemedicine services. CMS is now proposing additional changes to the Medicare Shared Savings Program to further accelerate telemedicine use (2). While Medicare policy to promote telemedicine has largely focused on ACOs, the current use of telemedicine by ACO providers is unknown.
Therefore, we aimed to examine the impact of Medicare Shared Savings Program ACO policy initiation on the use of telemedicine for evaluation and management services provided to Medicare beneficiaries.
Using claims from a 20% national sample of fee-for-service Medicare beneficiaries and the Medicare Shared Savings Program ACO research identifiable file, we identified all evaluation and management visits from 2009 through 2015 performed by ACO and non-ACO providers. We defined telemedicine visits as those with a telemedicine-specific Current Procedural Terminology code (G0425-7, G0406-8, G0459) or modifier (GT, GQ).
We calculated the proportion of total evaluation and management visits that utilized telemedicine for ACO and non-ACO providers, by year of service. We used a Pearson’s chi-squared test to assess the relationship between ACO-participation and telemedicine use. To evaluate the impact of ACO policy initiation, we performed an interrupted time-series analysis. The dependent variable was use of telemedicine during an evaluation and management visit. We estimated a logistic model with quarterly linear splines after ACO initiation, adjusted for clustering at the provider level.
A P value of less than 0.05 was considered significant. Statistical analyses were conducted using Stata 15.1 (College Station, TX, USA). This study was deemed exempt from review by the institutional review board. This work was supported by NIA R01 R01-AG-048071 (BK Hollenbeck) and the MPrOVE Research Innovation Challenge Grant by the Institute of Healthcare Policy and Innovation (C Ellimoottil). The funding agencies had no role in the design of the study, analysis, collection, or interpretation of the data, nor in the decision to submit the manuscript.
We identified 629,810,363 evaluation and management visits provided by Medicare providers from 2009 through 2015. Of these, 180,559 (2.9 per 10,000) were identified as telemedicine visits. Medicare providers increased their use of telemedicine from 1.0 visit per 10,000 in 2009 to 5.4 visits per 10,000 in 2015. Both ACO-participating providers and non-ACO providers increased their use of telemedicine (Figure 1). Overall, non-ACO providers used telemedicine for a greater proportion of evaluation and management visits than ACO-participating providers (3.3 per 10,000 vs. 0.3 per 10,000, P<0.001). Among ACO providers, the proportion of telemedicine visits increased yearly, but the initiation of ACO policy was not independently associated with any change in the use of telemedicine visits {odds ratio 0.98 per quarter; [95% confidence interval (CI), 0.92–1.03], P=0.41}.
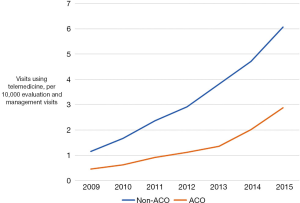
Telemedicine is increasingly used in the Medicare program (3). Despite this growth, we found that ACO-participating providers conducted disproportionately fewer telemedicine visits than non-ACO providers and did not significantly increase telemedicine use after ACO policy initiation. There are several factors that may explain the relatively low adoption of telemedicine services by ACO providers. First, while Medicare has removed limitations to reimbursement for telemedicine services for some ACOs, these are primarily risk-bearing ACOs. Most ACO providers during our study period, however, participated in one-sided risk models, under which they do not bear downside risk if spending exceeds benchmarks. As a result, most ACOs in the Medicare Shared Savings Program are not exempt from the telemedicine payment requirements. These Medicare regulations specify that telemedicine services can only be reimbursed under the physician fee schedule if provided to beneficiaries who reside in rural areas or outside of a metropolitan statistical area (4). Additionally, beneficiaries accessing telemedicine services must do so from a medical facility, and cannot be at home. Second, the low utilization of telemedicine by ACO providers may be further explained by the fact that ACOs have formed primarily in urban areas may not serve enough rural patients to spur investment in telemedicine technology (5,6). Geographic requirements for payment have been eliminated for Next Generation ACOs and in proposed changes to Medicare Shared Savings Program ACOs (7,8), which may foster telemedicine adoption in the future.
In addition to uncertainty regarding Medicare reimbursement for telemedicine services, hospitals and physician groups must consider commercial payers’ payment policy as well. Recent analyses have suggested that commercial payers are uncertain about the value of telemedicine and may have variable coverage of these services, further limiting enthusiasm for provider groups to invest in this technology (7). While cost and reimbursement issues appear to be the most important barriers to widespread telemedicine adoption, qualitative studies have also cited technical issues (lack of adequate equipment and incompatible electronic medical record systems), personnel limitations (insufficient staffing, no clear workflow process), and the perception that some patients were not well suited to participation in telemedicine visits (9).
Ultimately, payment policy designed to foster the adoption of telemedicine is likely to increase its use. However, CMS is understandably concerned about the potential for expansion of potentially low-value telemedicine services if they are fully reimbursed for all beneficiaries in fee-for-service Medicare. Given the overlap between the goals of ACOs and the potential benefits of telemedicine, and the need for ACOs to investigate and control the value of telemedicine services delivered, risk-bearing ACOs seem to be an ideal laboratory for CMS to understand the utilization of telemedicine services.
Acknowledgements
Funding: This work was supported by NIA R01 R01-AG-048071 (BK Hollenbeck), NCI F32 CA232332 (PK Modi) and the MPrOVE Research Innovation Challenge Grant by the Institute of Healthcare Policy and Innovation (C Ellimoottil). The views expressed in this manuscript do not necessarily reflect the official policies of the NIH nor imply endorsement by the U.S. Government.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Report to Congress: E-health and telemedicine. Office of Health Policy, Office of the Assistant Secretary for Planning and Evaluation, Washington, DC: Department of Health and Human Services. Available online: https://aspe.hhs.gov/sites/default/files/pdf/206751/TelemedicineE-HealthReport.pdf
- Medicare Program; Medicare Shared Savings Program; Accountable Care Organizations-Pathways to Success. Available online: https://www.federalregister.gov/documents/2018/08/17/2018-17101/medicare-program-medicare-shared-savings-program-accountable-care-organizations-pathways-to-success
- Mehrotra A, Jena AB, Busch AB, et al. Utilization of Telemedicine Among Rural Medicare Beneficiaries. JAMA 2016;315:2015-6. [Crossref] [PubMed]
- CMS. Medicare learning network: Telehealth services. 2018. Available online: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/TelehealthSrvcsfctsht.pdf
- Lewis VA, Colla CH, Carluzzo KL, et al. Accountable Care Organizations in the United States: market and demographic factors associated with formation. Health Serv Res 2013;48:1840-58. [Crossref] [PubMed]
- Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med 2017;377:1585-92. [Crossref] [PubMed]
- Commission MPA. Chapter 16. Mandated report: Telehealth services and the Medicare program. 2018. Available online: http://www.medpac.gov/docs/default-source/reports/mar18_medpac_ch16_sec.pdf?sfvrsn=0
- Next Generation ACO Model Telehealth Expansion Waiver Frequently Asked Questions. Available online: https://innovation.cms.gov/Files/x/nextgenaco-telehealthwaiver.pdf
- Lin CC, Dievler A, Robbins C, et al. Telehealth In Health Centers: Key Adoption Factors, Barriers, And Opportunities. Health Aff (Millwood) 2018;37:1967-74. [Crossref] [PubMed]
Cite this article as: Modi PK, Kaufman SR, Portney DS, Ryan AM, Hollenbeck BK, Ellimoottil C. Telemedicine utilization by providers in accountable care organizations. mHealth 2019;5:10.


