mHealth to promote pregnancy and interconception health among African-American women at risk for adverse birth outcomes: a pilot study
Introduction
The use of mobile phone applications (mHealth) to provide health education and behavioral prompts is one of the twelve common mHealth functions identified by the World Health Organization as innovations to strengthen health systems (1). Among low-income pregnant and parenting women, health education is widely recognized as a way to improve maternal and infant health outcomes, but the efficacy of written health education materials to change knowledge and behavior for this population is questionable (2,3). MHealth prompting, in contrast, is a promising alternative.
The literature about mHealth regarding receipt of recommended pregnancy and interconception care can be sorted by acceptability for use and effectiveness in achieving behavioral outcomes. Pregnant women’s interest in using mobile phone applications to expand their access to interconception and prenatal health information and services in one Argentinian study was very high (4). In Tanzania, L’Engle and colleagues found that Mobile Phone Interventions for Reproductive Health (m4RH), an opt-in interactive and menu-based short message service (SMS or text message) system that provides automated information about eight different long-acting, short-acting, and coitally-dependent family planning methods, was also highly used by the target group (5).
Text-4-Baby, the first free mobile health information service in the US, launched in 2010, is intended to reach and engage the widest national cross-section of pregnant women and new mothers with three free short messages (SMS) per week about key prenatal and postpartum health behaviors (Text-4-Baby, 2014) (6) Although Text-4-Baby was written for all literacy levels, a 2012 study indicates that health literacy influences women’s success in enrolling in Text-4-Baby to receive the messages (7). Health literacy, according to The U.S. Patient Protection and Affordable Care Act of 2010, Title V, is defined as, the degree to which an individual has the capacity to obtain, communicate, process, and understand basic health information and services to make appropriate health decisions (8). Gazmararian and colleagues found that only half of the women with low health literacy scores successfully self- enrolled in Text-4-Baby, suggesting that some women with low health literacy scores may need face-to-face support to engage effectively with mHealth education applications (7).
The literature reporting the effectiveness of mHealth in engaging women and promoting positive reproductive health behaviors and ultimately, maternal-infant health outcomes, is critical to the informed assessment of the value of mHealth in maternal-newborn health. A global review of mHealth in maternal and newborn health programs and their outcomes concluded that there is very little literature to date that corroborates the impact of mHealth with indicators of maternal and newborn health (9).
A recent systematic review of text messaging for maternal and infant health has shown mixed results on a wide variety of outcomes related to adherence to medications, contraceptives, clinic attendance, smoking cessation, diabetes and substance abuse management. Among the authors’ conclusions was motivational messages have been found more effective for behavioral change than informational messages, and variation in content and timing for medication adherence is preferred (10).
There is evidence of positive impact of mHealth in promoting safer sex among youth. A randomized control trial that used mobile advertising to promote safer sex to youth showed improved knowledge and behavioral differences among users of the technology compared to non-users (11). Katz and colleagues conducted a randomized trial of mobile phone-based counseling to prevent subsequent pregnancy in teen mothers in Washington, DC. They found significantly fewer subsequent pregnancies among adolescents between 15 and 17 years who received the intervention compared to controls who did not, but no differences among adolescents 18 years or age and older (12,13). Two studies in Thailand demonstrated improved adherence to prenatal and well-woman appointments among users of text messaging (14,15).
To our knowledge, no mHealth tools containing interactive features have been developed for women that span the pregnancy, postpartum, and interconception stages of women’s reproductive lives. The issuance of adherence reminders for contraception, folic acid supplements, and prescribed chronic medications is one strategy to reduce unintended pregnancies and promote women’s health in these periods. As a prerequisite to designing a study to measure the health and behavioral impacts of implementation of mHealth, our team adopted a community-based participatory research approach to test the acceptability and feasibility of an interactive mHealth application among reproductive age African American women during various reproductive stages (pregnancy, postpartum, and interconception). The goal of employing the mHealth application was to encourage low resource African American women in the U.S., who live in neighborhoods with the highest rates of adverse pregnancy outcomes and infant mortality in Atlanta, Georgia, to adhere to medically recommended prenatal vitamins, prenatal clinic visits, and interconception family planning use after their delivery. In this article, we report the creation, implementation, and results of the mobile phone application designed for this population.
Methods
Setting and participants
We implemented the mHealth application with clients of the Center for Black Women’s Wellness (CBWW), which is the only organization in Atlanta, Georgia, with a federally funded Healthy Start (HS) Initiative. HS programs have been shown to contribute to improved maternal infant outcomes (16); and CBWW staff had an already established community-based participatory research team who had worked on prior projects, with one of the Center Family Support Workers having been trained as a community researcher. HS programs serve women at high risk for adverse pregnancy outcomes.
For the community-based participatory component of the research, we identified three constituent stakeholders who would have an interest in the mHealth application features and results: women enrollees using the phones, health care providers who care for women from these neighborhoods during pregnancy, postpartum, and interconception periods, and the HS Consortium members. The Atlanta Healthy Start Initiative (AHSI) Consortium is a group of approximately 50 neighborhood, civic, clergy, and agency representatives who meet monthly to discuss issues of relevance to the improved health and quality of life of the population being served by HS. The Consortium also includes graduates of the HS program as well as health providers and hospital administrators. Additionally, the program was presented to the advisory board of the Urban Health Initiative at Emory University, a multidisciplinary group whose mission is to improve the health of and decrease disparities among the diverse and underserved populations in Atlanta.
Recruitment and sample
The targeted enrollment for the client-level implementation component of our study was 15 women over a three month period. Inclusion criteria included being a resident of Neighborhood Planning Units (NPUs) L and V in metro Atlanta, age 18–44, past or present participant in the AHSI, English-speaking, and having the capacity to provide informed consent for oneself. The city of Atlanta has 25 NPUs, each representing a specific geographic area. A previous study that used a community-based participatory research strategy to address priority health problems in Atlanta, such as infant mortality, identified NPUs L and V as the highest priority areas, which include over 5 contiguous neighborhoods (17). In Atlanta specifically, HS participants come from NPUs L and V, which consist of approximately 23,000 residents, 92% of whom are African-American, 62% are at or below 100% of the US federal poverty level, and 88% of households are headed by women. These neighborhoods have high crime rates and the highest rates of poor birth outcomes in the city (17).
A convenience sample of women within the HS program was recruited by a university and a community researcher first by telephone, and then face-to-face within the CBWW, until the target sample was achieved. Women were informed that each participant would have at least 3 months to use the phone and the application to test it. Final enrollment during the designated three month recruitment period was 14 women.
Incentives
Institutional Review Board approval was obtained from the academic authors’ universities. After obtaining informed consent, each participant was issued a flip mobile phone with a unique telephone number. As an incentive, the phone was equipped with unlimited text and 250 min for talk monthly for the duration of the study (6 months for those who were enrolled early and 3 months for the last enrollee). At the end of the study period, participants were given their phones to keep, but the mobile phone service was terminated.
The mHealth application
The mHealth application was the creation of a highly interdisciplinary team from one community-based and two academic institutions with collective expertise in Midwifery and Women’s Health, Preventive Medicine, Anthropology, Computer Science/Sensors and Systems, and Community-Based Case Management. After receiving approval from both universities’ Institutional Review Boards, the team created the script for outgoing messages, questions, and possible responses for the application. Each of the messages was aligned with the evidence-based recommendations developed by the Select Panel on Preconception Health and Health Care (Centers for Disease Control, 2006) (18).
The mHealth application was designed to be interactive; participants received and were prompted to respond to text messages according to their assigned profile. Specifically, the application was organized so that women were placed into any one of four pre-defined profiles based upon their reproductive stage: early pregnancy (pregnant women up to 28-week gestation), late pregnancy (pregnant women from 28 weeks to delivery), postpartum (women who had just delivered through 6 weeks postpartum) and interconception (women beyond 6 weeks postpartum). As their reproductive stage changed, so did their assigned profile, and therefore, the content of the messages and prompts they received. Women in each profile received questions on a daily, weekly, or monthly schedule via text message. All women received specific, timed, informational messages which are presented in Figure 1.

In addition to informational text messages, the mHealth application sent prompts with pre-defined responses for users to reply to with a “yes,” “no,” or “not yet” response. Responses were captured and recorded on a password protected website, available only to the research team. The responses were recorded in real time on the encrypted website. Messages were classified into two types according to their content: primary and secondary. Primary messages were prompts sent to the participants with content specific to their profile. Secondary messages were sent as a response to a participant’s reply to the primary message. For example:
- Primary message: Have you taken your prenatal vitamin today? Press 1 for Yes, 2 for No, 3 for Not Yet.
- Participant response: 1.
- Secondary message: Great! Thanks for your response.
Data collection
For evaluation of the client-level implementation of the mHealth application, data was collected from two sources from the women enrolled in this study.
- HS records. Sociodemographic information including maternal age, race/ethnicity, education level, and marital status were collected from registration information of the HS clinic.
- mHealth tool feedback. Data from the encrypted website associated with the mHealth tool contained the time-stamped receipts of messages of particular content that was sent to and from the participants.
Community participatory feedback
For the community-based participatory portion of this study, face-to-face, qualitative group interviews were conducted with the participants with phones three times throughout the study to discuss what they liked and did not like about the mHealth application and its messages. These meetings were audiotaped and transcribed verbatim. Also, the research team presented the study and requested feedback during one of the AHSI Consortium meetings.
Finally, two groups of health providers were presented with the study and specific feedback was elicited about the informational text messaging content at two different sites, a hospital site (primarily OB-GYN physicians and nurses), and one community site (Family Medicine Residents). Since the work schedules of health providers rarely allows time to participate in the AHSI Consortium’s monthly lunchtime meetings, our team scheduled meetings at grand rounds and before a scheduled lecture for residents to maximize the number of participants. Sixty-two physicians and nurses were present at the Medical Grand Rounds and 19 Family Medicine residents were present at the lecture at the community site. Participants were given a copy of the messages and requested to write on the paper or verbally discuss what else they would include in the messages.
Analysis
A summary of the text message content, along with the frequency of delivery, and the profile of the participant to whom the message was analyzed is presented in Figure 1. The average response rates for the participant women to outgoing messages were calculated for each participant according to: (I) week of participation in the study, (II) profile throughout their participation in the study, and (III) response to specific message content. The profiles, as described above, were defined as: pregnancy less than 28 weeks (pregnancy <28 weeks), pregnancy greater than 28 weeks (pregnancy >28 weeks), postpartum, and interconception. For the community-based participatory component of this study, the transcripts of the qualitative interviews were reviewed and summarized for the key messages. The health provider feedback was summarized.
Results
Demographics and participation
The final enrollment in this study was fourteen participants. All participants were single, African American women, with the average age of 21.8 years (range, 16–31 years). Thirteen participants were unemployed (93%), while one participant was employed part-time. Two had completed eighth grade (14%), 8 had some high school or in process of obtaining their GED (57%), 3 had graduated from high school (21%), and 1 was unknown. Six participants in the study were first-time mothers (43%), while the remaining eight participants (57%) had previous children.
The enrollment time and duration of participation in the study varied for each participant. The average duration of participation in the study was 7.21 weeks, with a range of 2 to 11 weeks. Figure 2 presents the average response rates for each participant through the various reproductive phases.
Participant response rates
Participant response rates were calculated according to week of participation, profile, and response to specific message IDs. One hurdle in this data analysis is that participants only have the ability to respond to the most recent primary message they had received. Therefore, they could not reply directly to any previous primary messages from days prior to the most recent primary message. In the event that they had attempted to respond to several primary messages at one time, they would receive a secondary prompt (message ID # 41 in Figure 1). It was difficult to determine which primary messages some of the participants were intending to respond to, as many would continue to send responses back after receiving the secondary messages.
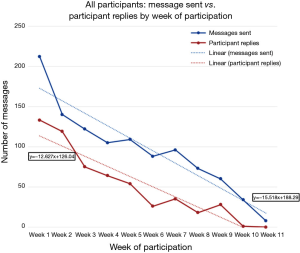
When calculating response rates by week of participation, participant responses to both primary and secondary messages were included. Average response rates did trend down by week of participation. However, participants were receiving fewer messages as their duration of participation increased and the profiles of participation were not taken into account. The number of messages received and replied to by week of participation for all participants is displayed in Figure 3.
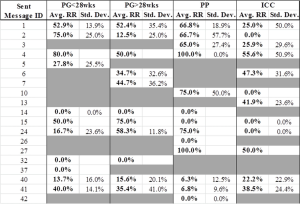
Participants were most likely to respond to message IDs #1 (“Have you taken your prenatal vitamin today?”), #2 (“What birth control method do you use?”), and #4 (in response to the question, “Are you protected from sexually transmitted infection?”) in the pregnancy less than 28 weeks profile, with response rates of 52.9%, 75%, and 80%, respectively. In the pregnancy greater than 28 weeks profile, the highest response rates were seen for message IDs #1 (“Have you taken your prenatal vitamin today?”) (52.4%), #15 (“People who are overweight have a higher risk for complications…”) (75%), and #24 (“Depression is common…”) (58.3%) (refer to Figure 1 for reference to message ID with complete content of message). The postpartum profile had the highest response rates for the majority of message IDs received during that period, yielding response rates equal to or greater than 65% for seven different messages. Finally, the interconception profile had the lowest response rates per message IDs, with messages #4 (“Don’t forget!.”), a secondary message (50.9%), #6 (“Have you taken your multi-vitamin and any prescribed medications?”) (47.3%), and #27 (“Reminder: Got appointment for next Depo shot?”) (50.0%) rank the highest.
Qualitative feedback
One of the most surprising and unanticipated results was that all the participants in the sample had smartphones, which meant that the flip phone was an extra device they needed to carry. However, participants did not necessarily have continuous service on their smartphones, so they would episodically use the flip phones they were issued to place personal phone calls and send/receive personal text messages. Participants commented that they did not like carrying two phones and would have preferred to receive the messages on their personal phone, with compensation for extra data and messaging on their personal cell phone plan. Despite carrying an extra phone, at each of the three participant meetings, 10 of the participants reported that they found the reminders for appointments and for prenatal vitamins helpful. Additionally, they suggested two additional messages. Four participants suggested reminders for their well-baby visits and two participants suggested that a message should be sent every 1 or 2 weeks to inquire about their mental health (“Asking about how you been ‘feeling’ this week”), followed by a hotline number if they responded that they were not doing well. There was general agreement by the others that both of these additional messages would enhance the application.
There were also 2 negative reports (14%) that the application became an annoyance over time. “It become boring,” said one participant. “Me, I hate automatic (messages),” said another.
Of the 14 participants, 3 lost their phones over a 6-month period (21%).
The feedback from the health providers was much more detailed and organized around tailoring questions for individuals to respond to their specific needs, with much more frequent messaging on a larger volume of topics, timed to the ideal of when tests should be done. Their suggestions were focused on inquiring if they had already received the information they needed for recommended lab tests, symptoms of labor, danger signs in labor, breastfeeding, contraception, and sexually transmitted infections.
Study limitations and lessons learned
The mHealth technology required brief training, which the community workers provided. However, it also required monthly renewal of the participants’ text message and voice plans. The monthly renewal posed challenges with gaps in communication. Participants were enrolled at varying times during the recruitment period; therefore not all participants needed renewal at the same time. Participants had a limited number of voice minutes, so the overuse caused plan access issues and overage charges. The high occurrence of overuse indicates that the participants may have needed reminders of the phone plan restrictions. If a phone did not have minutes, then it would not be taken with participants or charged when the plan was renewed. Even when service was restored, the participants would not know and therefore would not be able to respond to the messages.
The computer science members of the research team did not interact directly with the participants. Participant feedback to the technical team was routed primarily via the in-person meetings with the qualitative research team or a noted request from the AHSI community workers. Therefore, issues could not be resolved in real-time.
It is highly important for technology to meet the needs of the participant group. At the start of the pilot, it was determined that the study team should procure phones for the participants in order to mitigate the HS community member populations’ behavior of changing phone providers and phone numbers during the study. However, since the participants already owned smartphones, the study phone was used as a back-up at times and was not able to gain the attention of a primary communication device. Also, 3 participants (21%) lost their provided phones during the duration of their participation in the study.
Overall, the technical issues with the service boiled down to a matter of logistics needed to maintain close communication with the participants. Some suggestions to mitigate this in future and scaled-up studies include phone plans that were automatically renewed, a technology assessment to determine equipment needs and preferences of participants, pre-installation of issue “hot-line” phone number installed on the phones, an alternative contact number for the participants, the addition of a question to ask for feedback on the service via text message, and the addition of a statement to remind participants of their phone plan restrictions.
Discussion
In summary, all stakeholders contributed to a better understanding of a mHealth application that would potentially be user-friendly and effective with the population under study. The majority of the participants in the pilot found the messages helpful. They wanted more focus on their mental health and also requested reminders for their babies’ well-child appointments. Providers wanted more interaction on the specific laboratory and diagnostic tests conducted during pregnancy. Specifically, the OB-GYN provider group wanted the application to include medical record information accessible on the phone. The Family Medicine physicians, on the other hand, were more focused on learning if their patients had received the information that they wanted or needed. They felt it would be helpful to know the summaries of these responses, so that they could individualize their care with assistance of a case manager.
The particular strengths of the project included the piloting of an interactive application across a changing spectrum of women’s reproductive needs. Most applications apply only during pregnancy or only during contraception. A more holistic application can provide reminders during the tumultuous transitions in women’s lives from pregnancy to postpartum to interconception care. Women told us they wanted it to remind them of their babies’ care as well.
Another valuable component to the study was the inclusion of multidisciplinary perspectives; from users, to clinicians, to community, in order to inform future iterations of the mHealth application. The clinical perspective, however, must incorporate the logistic and technical requirements to make a more sophisticated application feasible financially, which only the computer scientists could evaluate. If the population using the application already had smartphones, however, the cost of providing phones incurred in this study could be reallocated to more detailed programming in future projects.
Another strength of the study was that the mHealth application was not simply “an app”. It included the encrypted website that captured responses in real-time. The persons who could view these responses were researchers in this case, but in the future, with prior patient permission, clinicians or case managers could use the real-time web information to help identify those for whom special outreach contact would be beneficial to their health. This could help distinguish those who needed more frequent visits or more concentrated case management. This aspect of the application is especially important with low health literacy populations, as Gazmararian et al., pointed out, regarding the need for face-to-face support with cellular education messages (7). The research team hopes to incorporate not only the lessons learned for future scale up, but also to enhance the application by means of the input of the participants, providers, and invested community members to amplify the benefits of mHealth to promote pregnancy and interconception health.
Acknowledgements
The authors gratefully acknowledge all the staff at the Center for Black Women’s Wellness, as well as Research Assistants, Ms. Jennifer Hudson, BSN, MPH, from Emory University and Mr. Trevor J. Goodyear, Georgia Technology Research Institute, Atlanta, Georgia.
Funding: This study was supported by PHS Grant # UL1TR000454 by from the Clinical and Translational Science Award Program, National Institutes of Health, National Center for Research Resource.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Ethical Statement: The study was approved by the institutional review board of both Emory University and Georgia Institute of Technology in Atlanta, Georgia. Written informed consent was obtained from the participants.
References
- Labrique AB, Vasudevan L, Kochi E, et al. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract 2013;1:160-71. [PubMed]
- Poorman E, Gazmararian J, Elon L, et al. Is health literacy related to health behaviors and cell phone usage patterns among the text4baby target population? Arch Public Health 2014;72:13. [PubMed]
- Gazmararian JA, Elon L, Yang B, et al. Text4baby program: an opportunity to reach underserved pregnant and postpartum women? Matern Child Health J 2014;18:223-32. [PubMed]
- Cormick G, Kim NA, Rodgers A, et al. Interest of pregnant women in the use of SMS (short message service) text messages for the improvement of perinatal and postnatal care. Reprod Health 2012;9:9. [PubMed]
- L'Engle KL, Vahdat HL, Ndakidemi E, et al. Evaluating feasibility, reach and potential impact of a text message family planning information service in Tanzania. Contraception 2013;87:251-6. [PubMed]
- Text4baby. Healthcare provider Text4baby basics. 2014. Available online: https://partners.text4baby.org/index.php/get-involved-pg/partners/healthcare-providers/h-p-text4baby-basics
- Gazmararian JA, Yang B, Elon L, et al. Successful enrollment in Text4Baby more likely with higher health literacy. J Health Commun 2012;17 Suppl 3:303-11. [PubMed]
- Centers for Disease Control and Prevention. Health literacy. Available online: http://www.cdc.gov/healthliteracy/Learn/index.html
- Tamrat T, Kachnowski S. Special delivery: an analysis of mHealth in maternal and newborn health programs and their outcomes around the world. Matern Child Health J 2012;16:1092-101. [PubMed]
- Poorman E, Gazmararian J, Parker RM, et al. Use of text messaging for maternal and infant health: a systematic review of the literature. Matern Child Health J 2015;19:969-89. [PubMed]
- Gold J, Aitken CK, Dixon HG, et al. A randomised controlled trial using mobile advertising to promote safer sex and sun safety to young people. Health Educ Res 2011;26:782-94. [PubMed]
- Katz KS, Rodan M, Milligan R, et al. Efficacy of a randomized cell phone-based counseling intervention in postponing subsequent pregnancy among teen mothers. Matern Child Health J 2011;15 Suppl 1:S42-53. [PubMed]
- Katz R, Mesfin T, Barr K. Lessons from a community-based mHealth diabetes self-management program: "it's not just about the cell phone J Health Commun 2012;17 Suppl 1:67-72. [PubMed]
- Jareethum R, Titapant V, Chantra T, et al. Satisfaction of healthy pregnant women receiving short message service via mobile phone for prenatal support: A randomized controlled trial. J Med Assoc Thai 2008;91:458-63. [PubMed]
- Kaewkungwal J, Singhasivanon P, Khamsiriwatchara A, et al. Application of smart phone in "Better Border Healthcare Program": a module for mother and child care. BMC Med Inform Decis Mak 2010;10:69. [PubMed]
- Health and Human Services. Child Health USA 2013. Available online: https://mchdata.hrsa.gov/dgisreports/PerfMeasure/default.aspx
- Kreuter MW, Kegler MC, Joseph KT, et al. The impact of implementing selected CBPR strategies to address disparities in urban Atlanta: a retrospective case study. Health Educ Res 2012;27:729-41. [PubMed]
- Johnson K, Posner SF, Biermann J, et al. Recommendations to improve preconception health and health care--United States. A report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep 2006;55:1-23. [PubMed]
Cite this article as: Foster J, Miller L, Isbell S, Shields T, Worthy N, Dunlop AL. mHealth to promote pregnancy and interconception health among African-American women at risk for adverse birth outcomes: a pilot study. mHealth 2015;1:20.