Healthcare and healthcare systems: inspiring progress and future prospects
Introduction
Health care and health systems all over the world are undergoing intensive reforms. Internationally, the existing institutions for multilateral cooperation are facing unprecedented challenges. Many institutions are finding it increasingly difficult to fulfill their mandates. There are inefficient overlapping efforts among various multilateral organizations, but paradoxically, there are responsibility voids in executing some key functions. At the same time, other players, such as non-governmental organizations and transnational corporations, are gaining prominence.
In today’s more complex world, it is difficult to define health systems, what it consists of, where it starts and where it ends. The World Health Organization in its report on Health systems in 2000 defined health systems as “all activities whose main responsibility is to promote, restore and maintain health” (1).
Multiple forces are transforming the pattern of disease and health as well as creating a need for new institutional arrangements. Just as governments are reinventing their respective national health systems, international health must be rethought so that it can respond effectively to the emerging challenges.
The current paper discuses opportunities and challenges around global health care systems in next 25–30 years. The paper will analyze the future needs of healthcare in next 30 years and review key achievements and challenges faced globally both in developing and developed countries. Geo-political and environmental forces will drive the transformation of health care delivery and finance over the next decade, leading to changes in hospital and health system.
Methods
A structured review of both peer-reviewed and gray literature on the subject was conducted. The search was conducted using the keywords “health systems progress”, “achievements”, “challenges, health indicators, future of healthcare” and “technology use in health”. The relevant information was collected.
Results
The result section was divided into two parts, including health systems progress over the last 30 years and health systems of future. These results were further grouped into categories and themes for better understanding.
Health system progress [1985-2015]
To move towards the future, it is extremely important that one must build on its past success and adapt to changing economic, demographic and epidemiological realities. On the whole, people are healthier, wealthier and live longer today than 30 years ago. If children mortality was still the same as that in 1978, there would have been 16.2 million deaths globally in 2006. Based on the latest UNICEF estimates, published in September 2014, the number of under-5 mortality worldwide has declined from 12.7 million in 1990 to 6.3 million in 2013, an overall decline of 50.3%. About half of these under-5 deaths occurred in only five countries: India, Nigeria, Pakistan, the Democratic Republic of Congo (DRC) and China (2). The 50% reductions of under-5 deaths can be attributed to the decrease in pneumonia, diarrhea, and measles. According to the statistics, these three illnesses were responsible for most of the deaths. However, if the trend continues even with this reducing rate, about 4.4 million children younger than 5 years will still die in 2030 (3). A number of initiatives gearing towards the improvement in the overall health status were commenced during these years, including Millennium Development Goals in 2000, Global Strategy for Women’s and Children’s Health in 2010 by the United Nations Secretary-General.
Population
The world’s population doubled between 1965 and 2010, reaching to 7 billion a millstone in 2011. Another historical milestone was achieved in 2007 when 50% of the global population lives in cities and towns, making urban centers the dominant habitat for humankind (4). Fertility decline and increased longevity contributed to increasing numbers and proportion of people aged 60 and over. Currently, there are 810 million people aged 60 and over worldwide, with a projection of 2 billion by 2050 and more people will be over the age of 60 than those aged 14 and under (5). In the future, population growth will occur mainly in developing countries. With relatively high birth rates and a high proportion of young people, populations of the least developed countries are projected to double from 803 million in 2010 to 1.7 billion by 2050. Table 1 gives comparison of global population between more developed regions and less developed regions in 1985 and 2015.
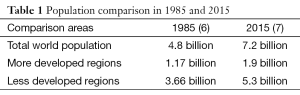
Full table
Life expectancy has also been improved worldwide, from 64 years in 1985 to more than 70 years in 2015, especially in Asia and Africa. Table 2 gives comparison of life expectancy between different continents in 1985 and 2015.
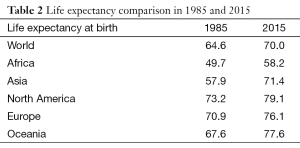
Full table
Health indicators
Although maternal mortality ratios (MMR) are still extremely high in most developing countries, it should be noted that these rates decreased substantially in many countries between 1990 and 2013. Tables 3,4 (8) explain and compare MMR in developed and developing countries.
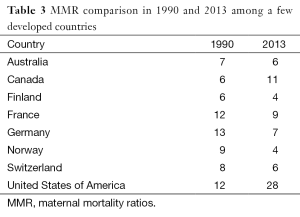
Full table
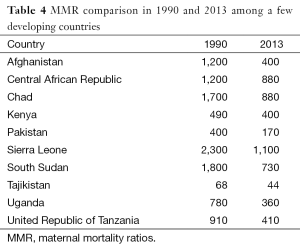
Full table
Infant mortality rates (IMR)
IMR correlates strongly with, and is the best predictors of the success or failure of a country. IMR is also a useful indicator of a country’s level of health or development, and is a component of the physical quality of life index. Though in the past 30 years, there was a trend showing a decline in IMR, the rate is still considered high in Africa and some Asian countries. Table 5 gives comparison of IMR between different continents in 1985 and 2015.
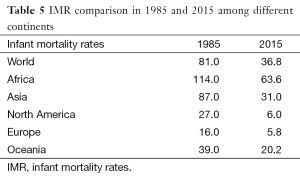
Full table
Health infrastructure—hospitals/facilities, number of beds
There has been a general upward trend in the number of both private and government hospitals over the last 30 years, with the biggest growth noted in the 1990s and a flattening decline in the last 10 years. Most hospitals are privately-owned, though there are roughly equal numbers of public and private beds. The expansion of private hospitals has been principally centered on urban or near-urban areas, leading to an inequitable distribution of health facilities and beds in those areas. Table 6 shows a decreasing trend in hospital beds from 1985 to 2015.
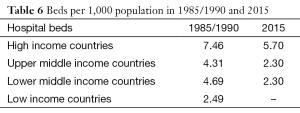
Full table
Health work force
Health workers are “all people engaged in actions whose primary intent is to enhance health” (9). These people not only include physicians, nurses and midwives, but also laboratory technicians, public health professionals, community health workers, pharmacists, and all other support workers whose main responsibility relates to delivering preventive, promotive or curative health services.
Low- and middle-income countries face the most severe challenges to ensure sufficient, fit-for-purpose and fit-to-practice health workforce. The situation was declared on World Health Day 2006 as a “health workforce crisis”—the result of decades of underinvestment in health worker education, training, wages, working environment and management.
A recent analysis conducted by the Global Health Workforce Alliance and WHO estimated there were 7.2 million professional health workers in 2012, with 83 countries facing a health worker crisis. Although the number of health workers is set to rise to 12.9 million by 2035, 100 countries currently are expected to fall below the threshold of 34.5 skilled health professionals per 10,000 populations (10).
Developing countries are committed in increasing health workforce to meet the WHO threshold of 2.3 heath workers per 1,000 people (11).
Health expenditure
Across the globe, there is an enormous disparity in the money countries spend on health. In high income countries, per capita health expenditure is over 3,000 USD, while in resource poor countries, it is only 30 USD per capita. In 2008, there were 64 countries with their health expenditure less than 100 USD per capita. There is also wide variation in health expenditure with respect to economic development. Some countries spend more than 12% of GDP on health, while others spend less than 3% on it (12). The US has the highest health spending in the world, equivalent to 17.9% of its gross domestic product (GDP), or $8,362 per person. And the government spending is at $4,437 per person, only behind Luxembourg, Monaco and Norway. Cuba has the highest government health spending in the world, accounting for 91.5% of all health spending. The result is 67.23 doctors per 10,000 populations, the highest of any major country. But it's beaten by the UK on the number of nurses. The UK has 101 nurses per 10,000 people, only behind countries like Norway and Germany. The UK also spends $3,480 per year on health—accounting for 9.6% of health spending, with government spending making up 83.9% of all health spending. Qatar has the lowest health spending in the world, 1.8% of GDP, followed by Burma (Myanmar) and Pakistan at 2.2% (13).
Achievements
In the past 30 years [1985-2015], world has witnessed many transitions in healthcare. The major achievements of the last three decades include:
- Health indicators (IMR, MMR) have been generally improved along with life expectancy;
- The prevalence of vaccine-preventable diseases was declining due to high and sustained immunization coverage;
- Strict control of infectious diseases led to increased life spans and a greater number of older populations;
- Upgrade of health infrastructure;
- More in-depth and reliable knowledge of health systems, health indicators and their challenges;
- Improvement of patient safety and quality in hospital care;
- Decreasing hospital admissions due to 40% drop in deaths caused by heart disease;
- Use of information technology to promote health care delivery, harnessed by both patients and providers (telemedicine, electronic health records, digital/distance learning, mHealth);
- New discoveries in health and hospital care such as breakthroughs in human genome and stem cell researches;
- New and advanced drug therapies extended survival in HIV and cancer patients;
- Minimally invasive and robotic techniques revolutionized surgery.
Challenges
Over the last 30 years, health systems around the world have faced multiple challenges. Some of them are listed below:
- Urbanization and changes in behaviors and diet contributed to an increased prevalence of chronic diseases such as hypertension, coronary artery disease, diabetes and cancer;
- UMany less economically developed countries were faced with double burden, which was persistently high rates of infectious diseases combined with rapidly rising rates of chronic diseases;
- UTraumatic injuries, violence and road traffic accidents further strained health systems, resulting in a triple burden, high rates of trauma, infectious and chronic diseases;
- UPeople have experienced epidemiologic transitions at different rates, which triggered needs for new health services and delivery systems;
- UMore focus on primary health care and less on secondary tertiary care levels;
- UDue to a large number of conflicts in different parts of the world over the last 30 years, implementing and sustaining health programs were serious challenges for the health community.
Future of healthcare [2015-2045]
Healthcare systems today have to address a host of different challenges resulting from medical and scientific advancement. Developments in the field of genetics, information technologies, and nanotechnology are enforcing a more individualized healthcare—often outside the hospital setting. And we have already seen the rise of user-centric healthcare and patient empowerment.
Concepts such as ‘the average patient’ are now viewed as outdated. And standards within modern medical systems are measured by different parameters, including patients’ access to the best-available treatments and to non-institutionalized care, compliance with treatments and even patient choice (14). A diverse group of health system leaders was asked to describe their ideal health system in 2040. Their visions are remarkable in their consistency. The preferred health system of the future is strikingly different from the national healthcare systems of today, with empowered patients, more diverse delivery models, new roles and stakeholders, incentives and norms (15).
Environmental forces will drive the transformation of health care delivery and finance over the next decade, leading to changes in hospital and health system. Over the next 30 years, most of the world’s population growth will occur in the urban areas of poor countries. Rapid, unplanned and unsustainable style of urban development will make developing cities the key focal points for emerging environmental and health hazards (16). By 2050, the median age of the population is projected to reach a remarkable level of 46 years in more developed regions. In less developed regions, the median age will increase more than 10 years reaching to 35 years in 2050, a level approaching to that of more developed regions currently (17).
Future hospital sector
In the future, hospitals will play a critical role in face of the challenges which the future healthcare will meet. Currently, a hospital building boom can be seen and fueled by increasing demand for health care services and increasingly obsolete hospital plant. Though international economy is expected to slow its pace, the continuing investment in hospital construction offers an opportunity to remake the hospital in its design, culture and practices in order to better meet the needs of patients and families and the aspirations of providers. Medical technology will keep advancing. Tools will become smaller and more mobile, allowing people to use them in the home setting. But, unless there are principles to guide the future development of hospitals, progress may simply be frozen in the status quo.
During the past several years, hospitals in the US have witnessed a decline in inpatient volumes along with a corresponding rise in outpatient utilization. It is forecasted that this trend will continue. Outpatient volumes will grow 17% in the next 5 years, while inpatient discharges are expected to go down by 3% (18). This ongoing shift to the outpatient setting has been driven largely by advances in minimally invasive surgical techniques and anesthesia that allow patients to recover more quickly.
This prediction for inpatient beds may be specific to the US, but it will be same in developing countries due to a number of factors: growth in population as well as ageing population with increased requirements for comorbid hospital care. The Advisory Board Researchers from Washington DC predicts that health care will face five forces over the next 5 to 10 years and beyond, population getting older, changes in lifestyle, information revolution, improvement in clinical technology and a new era of self-enabled healthcare consumer (19). Some of the forces are more complex than they seem and the challenge is when and how to adapt to them.
To adapt and be flexible is the key
The burgeoning cost of health care remains a major challenge for all countries. Given that the cost of hospitals is by far the largest component in most health systems, to rein in the cost of health care, we must improve hospital productivity. Today’s new hospital facilities are required to balance contradictory and competing demands of specialization and efficiency, high-end amenities and low operating costs, optimum clinical quality and minimized capital costs.
Setting priorities and developing strategies for a new facility project is highly sensitive to the future market, and there is no “one-size-fits-all” solution for every institution. The research from Advisory Board shows that increasing investments in infrastructure aiming to improve clinical quality and best-in-class cost performance will provide a competitive advantage regardless of the nature of the future market. Accordingly, their research showed 16 experience on building high quality, low-cost inpatient facilities and making critical implementation decisions associated with facility strategy, such as capacity needs, space planning, design choices, and the construction process. Some lessons are summarized as follow:
- Provide flexibility and allow for changes at the same time. For example, we should pay attention to the impact of technology and demographic changes when building the facilities and building in phases is also important.
- Create as much as general purpose ORs, ICUs, and so on to allow for efficiency and flexibility rather than specific specialty needs. Private rooms are standard, though not mandated. Support facilities should be equipped in non-hospital grade space.
- With staffing shortages still looming in the hospital of the future, hospitals may need to accomplish more jobs with fewer health professionals. Well-functioning teams can do more than any individual.
- At the same time, outpatient and ambulatory work are on the increase. Prosperous economy is driving this move along with advances in medicine. More surgical cases and more non-invasive procedures will continue to occur in outpatient settings and facilities have to be more attractive and appealing to meet the needs of both patients and providers.
Must-do strategies to succeed in the future
The inaugural report of the American Hospital Association Committee on Performance Improvement detailed “Hospitals and Care Systems of the Future”, identified must-do, and developed priority strategies. They recommended that core organizational competencies organizations should be established and remain successful in this time with sweeping change (20).
- Aligning hospitals, physicians and other providers across the care continuum;
- Utilizing evidence-based practices to improve quality and patient safety;
- Improving efficiency through productivity and financial management;
- Developing integrated information systems;
- Joining and growing integrated provider networks and care systems;
- Educating and engaging employees and physicians to create leaders;
- Strengthening finances to facilitate reinvestment and innovation;
- Partnering with payers;
- Advancing through scenario-based strategic, financial and operational planning;
- Seeking population health improvement through pursuit of the “triple aim”.
Organizational core competencies
Organizations on path to implement the above must-do strategies should achieve competency in several areas of care delivery and organizational management. Similar to the strategies, these competencies are intrinsically connected and aligned. These are:
- Design and implementation of patient-centered, integrated care;
- Creation of accountable governance and leadership;
- Strategic planning in an unstable environment;
- Internal and external collaboration;
- Financial stewardship and enterprise risk management;
- Engagement of full employee potential;
- Collection and utilization of electronic data for performance improvement.
Focus for the next 30 years
Some of the top driving factors for the global healthcare system in the next 30 years are discussed below.
- Top causes of death must remain our core focus. The leading causes of death are similar across the globe, and the new evidence further supports the need for persistent and unwavering attention to the leading causes of under-5 mortality. Focus should be given to (21):
- Newborns. The number of newborn deaths is declining, but at a slower rate than under-5 deaths in the post-neonatal period. Thus, newborn deaths comprise an ever-increasing portion of total under-5 deaths. The World Bank Group’s Global Monitoring Report calls attention to this, noting that resources devoted to reducing child mortality rates should focus on the neonatal period.
- Pneumonia. Pneumonia accounted for approximately 15% of all under-5 deaths in 2013, and pneumonia mortality has decreased at a slower pace than other leading causes of child mortality, including malaria, measles and diarrhea. The funding to fight pneumonia is also uneven relative to its share of the burden: an estimated 2% of the $30.6 billion in development assistance spent in 2011 targeted pneumonia.
- Malaria. Reducing child mortality from 453,000 children estimated to have died of malaria in 2013 according to the latest World Malaria Report to fewer than 100,000 child deaths is within our reach.
- Non-health driving factors. There are some emerging issues in the global health community that also need attention if a healthier outcome is required. For example, compelling new evidence was released over past year that underscores the impact of nutrition, sanitation, women’s empowerment, and other underlying factors in driving unhealthy outcomes and mortality. The Global Nutrition report estimated a new, remarkable return on investment in nutrition: Across these 40 countries, for every dollar investment in nutrition, a greater than 16 dollar return is seen, competitive with investments in roads, irrigation, and health more generally (22). The latest malnutrition figures for specific countries are staggering, despite some progress in Afghanistan. The latest data suggest that reported rates of stunting in Afghanistan are still some of the highest in the world, ranging by province from 24–71%. Alarmingly, almost half of both stunting and wasting figures for children younger than 5 years in Afghanistan are severe. New research on malnutrition in India, suggests that a root cause may be poor sanitation, rather than a scarcity of food, and those underlying driving factors of poor nutrition (23).
- Investment in health workforce will be one of the best buys in healthcare for future. For instance, investing in midwifery education, with deployment to community-based services, can yield a 16-fold return on investment in terms of life saving and avoid unnecessary costs of caesarean sections. Health services should be organized, comprehensive, integrated and people-centered to increase access to health care in rural and remote areas. A greater focus is required on putting incentives in place and ensuring good working conditions that can enhance health workforce productivity, quality and responsiveness (24).
- Medical Tourism-growth in future healthcare scenario. Globalization and advances in technology have transformed health care in the past decade, making procedures such as remote diagnoses a more common practice. As part of that trend, cheaper travel has led to increasing numbers of people crossing the globe for medical care. Healthcare is the largest sector in the world and people spend huge amount to get the benefits of medical procedures to stay healthy and fit. It has become a major contributor in the GDP of destination countries, which offer quality medical procedures to people across the globe. It has one of the largest service sectors in countries like India, Singapore, Thailand, Malaysia, and South Korea (25). The worldwide medical tourism market is estimated to be worth $55 billion, and it is projected to continue growing by 20% a year (26). A cardiac treatment in India or Thailand could save an American patient roughly 80% of what it would cost out of pocket in the United States, said Cohen. Increasingly, insurers (especially self-insured firms) are providing medical tourism options in their plans as a way to cut their own costs, at least where permitted to do so by existing law (27).
Conclusions
The next 30 years will witness intense changes. There is no rocket science that patterns of previous 30 years will be repeated in exponential numbers. Providing and maintaining adequate clean water, good sanitation and nutritional food will take the center stage of humanities struggle. One the one hand, medical science is hopeful to solve the mystery of common chronic diseases and improve life expectancies. On the other hand, new diseases will emerge. Medical science will continue to be reactive to social forces and social forces will continue to be major determinants of health and disease in return. The emergence of new infectious agents will be closely related to human activities such as travel, trade, antibiotic usage and ecological degradation. The human-related factors of emergence will increase over the next 30 years. Human population growth on the planet will exacerbate epidemic activity. The breadth of transmission will continue to increase. The major threats to health will come from geopolitical, economic forces and individual behaviors.
Care will not be similar as minimally invasive techniques that may overtake traditional approaches. The lines between secondary and tertiary care will be blurred. Smaller and more manageable institutes and health centers will emerge, which will decrease health expenditures as providers will focus more on becoming self-sustainable. Medical care will be more self-directed as information is more accessible and user friendly with higher quality.
On the positive side, new technology will allow people to understand and characterize infectious agents’ emergence causes and what they spread more rapidly, and to produce effective vaccines more quickly. These two capacities will become central to control disease spread. Ebola virus in recent times is a very good example, which gives humanity a scare and hope at the same time. In addition, ability to accurately map the planet and its ecosystem may allow people to predict the occurrence of diseases, like weather predictions. Healthcare workforce will use multidisciplinary approaches to fill the gap of health human resource. At global level, countries will try to curtail their expenses and be open to more involvement of private sectors in healthcare.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- World Health Organization. World Health Report 2000. Available online: http://www.who.int/whr/2000/en/whr00_en.pdf
- World Health Organization. World Health Statistics 2008. Available online: http://www.who.int/gho/publications/world_health_statistics/EN_WHS08_Full.pdf
- Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000-13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet 2015;385:430-40. [PubMed]
- Population dynamics in the post-2015 development agenda: report of the global thematic consultation on population dynamics. Available online: http://www.unfpa.org/sites/default/files/pub-pdf/Population%20Dynamics%20in%20Post-2015%20FINAL.pdf
- Population dynamics in the context of the post-2015 development agenda beyond 2015. Available online: http://www.beyond2015.org/sites/default/files/Population%20Dynamics.pdf
- Our common future, chapter 4: population and human resources, from A/42/427. Our common future: report of the world commission on environment and development. Available online: http://www.un-documents.net/ocf-04.htm
- Current population trends. Available online: https://populationmatters.org/wp-content/uploads/D12Currentpopulationtrends.pdf
- Trends in maternal mortality: 1990 to 2013, estimates by WHO, UNICEF, UNFPA, the World Bank, and the United Nations Population Division. Available online: http://apps.who.int/iris/bitstream/10665/112682/2/9789241507226_eng.pdf
- World Health Organization. World Health Report 2006: working together for health. Available online: http://apps.who.int/iris/bitstream/10665/43432/1/9241563176_eng.pdf
- Health Workforce 2030: a global strategy on human resources for health. Available online: http://www.who.int/workforcealliance/knowledge/resources/strategy_brochure9-20-14.pdf?ua=1
- The Global Health Workforce Alliance 2013 Annual Report: rising to the grand challenge of Human Resources for Health. Available online: http://www.who.int/workforcealliance/knowledge/resources/ghwa_anual_report_2013.pdf?ua=1
- Ke X, Saksena P, Holly A. The determinants of health expenditure, a country level panel data analysis. Available online: http://www.who.int/health_financing/documents/report_en_11_deter-he.pdf
- Healthcare spending around the world, country by country. Available online: http://www.theguardian.com/news/datablog/2012/jun/30/healthcare-spending-world-country
- The future of healthcare: trends, opportunities & challenges. Available online: http://www.gilcommunity.com/docs/future-healthcare-trends-opportunities-challenges/
- Sustainable health systems visions, strategies, critical uncertainties and scenarios. Available online: http://www3.weforum.org/docs/WEF_SustainableHealthSystems_Report_2013.pdf
- World Health Organization. Environment and health in developing countries: future trends and emerging issues. Available online: http://www.who.int/heli/risks/ehindevcoun/en/index1.html
- World Population Ageing 1950-2050: changing balance between age groups. Available online: http://www.un.org/esa/population/publications/worldageing19502050/pdf/81chapteriii.pdf
- Adamopoulos H. The future of hospitals: visions of the healthcare landscape in 2035. Available online: http://www.beckershospitalreview.com/hospital-management-administration/the-future-of-hospitals-visions-of-the-healthcare-landscape-in-2035.html
- Hospital of the future: lessons for inpatient facility planning and strategy. The Advisory Board Company, 2007. Available online: https://www.advisory.com/research/health-care-advisory-board/studies/2007/hospital-of-the-future
- Hospitals and care systems of the future, American hospital association committee on performance improvement report. September 2011. Available online: http://www.aha.org/content/11/hospitals-care-systems-of-future.pdf
- Grabowsky M, Rockwell K. With one year to go, what the data say about MDG4 progress and gaps. Available online: http://www.mdghealthenvoy.org/with-one-year-to-go-what-the-data-say-about-mdg4-progress-and-gaps/
- International Food Policy Research Institute. 2014. Global Nutrition Report 2014: actions and accountability to accelerate the world’s progress on nutrition. Washington, DC. Available online: http://www.ifpri.org/sites/default/files/publications/gnr14.pdf
- A universal pathway. A woman’s right to health. Available online: http://www.unfpa.org/sites/default/files/pub-pdf/EN_SoWMy2014_complete.pdf
- Afghanistan in Transition: Call for Investment in Nutrition. Available online: http://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(14)70362-6.pdf
- Jagyasi P. Increasing healthcare costs in developed countries a boon for medical tourism market. Available online: http://www.medicaltourism.com/blog/increasing-healthcare-costs-in-developed-countries-a-boon-for-medical-tourism-market/
- Yamasaki D, Fujiwara T. Available online: Asia leads industry worth $55B. Available online: http://asia.nikkei.com/Business/Trends/Asia-leads-industry-worth-55B
- Walsh C. The rise of medical tourism. Available online: http://news.harvard.edu/gazette/story/2012/10/the-rise-of-medical-tourism/
Cite this article as: Durrani H. Healthcare and healthcare systems: inspiring progress and future prospects. mHealth 2016;2:3.


