Stroke patients and their attitudes toward mHealth monitoring to support blood pressure control and medication adherence
Introduction
Stroke is the leading cause of adult disability and the fifth leading cause of death in the United States, killing nearly 130,000 Americans each year—that is 1 of every 20 deaths (1). Someone in the United States has a stroke every 40 s. Every 4 min, someone dies of stroke (2). Every year, about 800,000 people in the United States have a stroke with about 610,000 first or new strokes and 185,000 recurrent strokes (2). At least 1 in 4 (25–35%) of those who have a stroke each year will have another stroke within their lifetime (3).
Stroke reduces mobility and increases disabilities with more than half of stroke survivors aged 65 years and over experiencing limitations in mobility (2). Additionally, stroke costs in the US are $34 billion annually, including the cost of health care services, medications, and lost productivity (2).
Recurrent strokes account for 25–30% of all strokes and are more disabling, fatal, and costly than primary stroke (4,5). The risk of recurrent stroke in survivors of acute stroke is about 11.1% (95% CI, 9.0–13.3%) at 1 year, 26·4% (95% CI, 20.1–32.8%) at 5 years, and 39.2% (95% CI, 27.2–51.2%) at 10 years (6). In young adults (18–50 years of age) who have had a stroke, the 20-year risk of recurrent ischemic stroke is about 19% (95% CI, 15–24%) (7).
Increased blood pressure (BP) is a leading risk factor for first stroke, recurrent stroke and premature death in the US and worldwide (2). In the year 2000, the world was estimated to have close to 1 billion people with hypertension and an increase to 1.56 billion was predicted by 2025 (2). The global economic burden of increased BP was estimated to consume US$370 billion worldwide and 10% of healthcare expenditures (8). Gaziano and colleagues estimated that control of BP could lead to a 32% reduction in stroke (8). On the basis of clinical and population research, increased BP, hypertension and hypertension-related complications are largely preventable. Antihypertensive drug therapy can effectively reduce the cardiovascular events attributed to hypertension (1-6). Nevertheless, most people with hypertension worldwide are not effectively treated and controlled to the recommended BP targets (2). Although there are many discussions about goal BP (150 or 140 or lower systolic and 90 or 80 diastolic), most all agree that for patients with stroke, BP control is a key consideration for effective prevention (9,10).
Use of remote monitoring via mobile health (mHealth) technology to improve medication adherence and BP control has increasingly been signaled as a means to improve outcomes for patients (11-21), especially those with chronic health conditions such as stroke. Given the prevalence and familiarity of mobile technology, mHealth promises to provide an especially useful and non-invasive tool to intervene in stroke populations with largely modifiable risk factors, such as high BP and medication management. Importantly, elevated BP (very treatable with medication) has the largest association with stroke recurrence out of all other risk factors. Medication adherence, vital to pharmaceutical efficacy and positive outcomes in this population, is possibly a target with great yield.
A key component to the success of any mHealth system is a positive, receptive attitude toward learning and implementing the technology. The stroke population presents a challenge to mHealth simply because the data are lacking regarding the receptiveness towards this technology. Thus, understanding stroke patients’ use of cellular and health technology devices and attitudes toward mHealth for medical regimen adherence will aid in identifying key indicators related to feasibility and optimal implementation of such technology to prevent and/or decrease the rate of secondary stroke and associated co-morbidities.
This study has several aims focusing on mHealth use. First, it seeks to evaluate a racially diverse sample of stroke patients on the use of cellular devices and attitudes toward use of a mHealth remote monitoring system, particularly to enhance medication adherence and BP control. The South Carolina stroke population, often described as the “buckle on the stroke belt”, offers a great chance to assess attitudes of patients in rural, underserved areas with limited access to providers. Second, it endeavors to explore whether demographics, clinical characteristics, prior technology utilization, and self-reported medication adherence impact receptivity toward mHealth. The study was approved by the Medical University of South Carolina Institutional Review Board.
Methods
Participants and recruitment
Study participants were patients who had been previously hospitalized at the Medical University of South Carolina Medical Center with a diagnosis of stroke (CVA) or transient ischemic attack (TIA), were ≥18 years of age and spoke English. A convenience sample of participants was recruited from the Medical University of South Carolina (MUSC) Ambulatory Stroke Clinics during their routine clinical follow-up visit post-stroke evaluation. Patients were approached regarding their willingness to receive information on a new prototype program and complete a survey by a clinical coordinator, clinic nurse, or physician.
Study setting and design
Clinical staff asked patients to visit with a research assistant in the stroke clinic. They received a description and demonstration of a mHealth enabled medical regimen system (i.e., smart phone with application, Bluetooth enabled BP monitor, electronic medication device) and completed a survey including questions on attitudes and receptivity toward mHealth system. Medication adherence was also evaluated through a survey. The above protocol was used in several previous studies to evaluate patient attitudes toward mHealth technology for chronic disease management among African American and non-Hispanic White kidney transplant recipients and Hispanic patients with uncontrolled hypertension (22,23).
Patients who agreed to participate in the research signed an informed consent following a discussion with the research staff where all questions were answered. Each participant was then given a verbal description and video demonstration of the procedural steps in using the prototype system that included use of:
- A wireless Bluetooth-enabled BP monitor (AND model UA-767 Plus BT; San Jose, Ca.) that would be used to take the participant’s BP and pulse every three days in the morning and evening;
- Use of a smart phone with an application that automatically acquired and presented audio and visual results of the BP readings and forwarded encrypted BP data from the phone to a secure server;
- A wireless (GSM-enabled) medication tray Maya MedMinder (Maya,Inc., Needham, MA) that would be used for all of their medications.
The explanation to the patient was that the smart phone would be used to automatically transfer the BP and pulse data to the computer for analysis and synthesis into weekly summary reports of BP ranges and levels and medication adherence to their health care provider. The medication tray plugs into a standard 110v outlet, has 28 compartments allowing up to 4 dose times per day for 7 days for all of their medications. It would be programmed to provide a series of automated escalating reminder signals every 30 min when it was time to take their medications (blinking light followed by a chime and finally if not taken after 1 h, a text or phone message was sent to the phone to remind the participant to take their medications. Adherence with medication would be tracked in real time and would trigger the delivery of motivational and social reinforcement messages via text, email, or phone the following day based upon degree of adherence. The healthcare provider team would receive notification if any session’s average BP reading was outside a preset range determined by the provider.
Following the demonstration of the prototype system, the participant was then asked to complete the survey that included questions related to patient demographics, personal medical history, and opinions on using mHealth strategies for medical regimen adherence. The survey included:
- Twelve items related to gender, yearly income, education, marital status, proximity to MUSC, and common co-morbidities such as hypertension, diabetes, arthritis and asthma;
- Nine questions to assess prescription compliance and frequency;
- Three questions to assess basic health literacy;
- Fourteen questions rating general medical knowledge of basic vascular disease;
- Two questions sets totaling 21 questions, 11 of which used a 5 point-Likert rating scale for evaluating attitudes and willingness to use mHealth for medical correspondence with providers. Queries targeted prior experience and ownership of technology, confidence with being able to learn use of mHealth software and hardware, and beliefs on mHealth confidentiality and efficacy.
The following scales were also included in the survey.
Medication adherence scale
A 7 item modified Morisky Medication Adherence Scale (mMMA) was used to assess medication adherence among the participants. The modified Morisky scale provides a score from range 0 to 7 with higher scores indicative of higher adherence to medication. The scale, initially developed and tested with hypertension patients, has an internal consistency of 0.82, sensitivity of 91%, sensitivity of 50% (24) and additional psychometrics have been evaluated in a variety of patients and disease states (22,23,25).
mHealth related survey
A 10-item survey evaluated participants’ attitudes toward mHealth and telemedicine based remote monitoring (22,23). Nine items are scored on a 5 point-Likert scale ranging from “Strongly disagree” to “Strongly agree” while one item has only two choice (Yes/No). The items were adapted from a questionnaire used to assess patients’ attitudes toward mobile phone based remote monitoring for chronic illness. Cronbach’s alpha for internal consistency in the current sample for the 9 items was 0.87. Examples from the survey included receptivity towards, comfort with mHealth technology, perceived security of their health information, and whether health care could still be judiciously provided from a distance.
Data management and analysis
All data were transmitted to a secure, password protected data management and storage system at the Medical University of South Carolina. Research Electronic Data Capture (REDCap) system serves as the data repository and is a secure, web application designed to support data capture and storage. The data were exported to SAS version 9.4 for analysis. Means (± standard deviation) and proportions for demographic and stroke related clinical characteristics are reported for the entire sample. Proportions and frequencies of participants’ attitudes towards mHealth and telemedicine based remote monitoring are provided. Demographic and stroke related clinical characteristics were compared by groups via pooled t-test or Chi-square/Fisher’s Exact test. Participants were grouped based on race (White vs. African-American/Black), and whether they answered “Agree” or “Strongly agree” to the question whether they would use the mHealth device if it was provided free of charge or replied “Disagree”, Strongly disagree” or were undecided (replied “Neutral”). Ordinal logistic regression was used to examine associations of demographic and clinical characteristics with attitudes toward use of mHealth technologies. Due to small cell sizes the neutral, disagree and strongly disagree categories were combined for this analysis.
Results
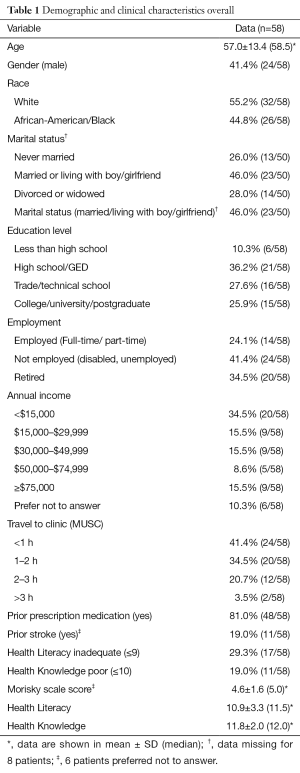
Between the months of June 2013 and July 2014, 60 persons completed the surveys during a stroke clinic visit. The mean age of participants was 57 years. The majority of participants were female (59%), White (55%), not married and/or living with a partner (54%), and had more than a high school education (54%). Over 80% reported using prescription medication prior to their stroke and almost 30% had inadequate health literacy (Table 1). White participants tended to be more educated compared to AA/B (P=0.43); more AA/B participants (65%) reported being disabled or unemployed while 47% in the White group were retired (P=0.004). Over 75% of AA/B participants reported a household income of less than $30,000 compared to 38% of White participants (P=0.004).
Full table
Medication management
Almost half of the 60 (41.67%) reported some difficulty with daily medication adherence; however, based on data below, only about 28.3% forgot to take their medications while 71.7% reported “never/rarely” forgetting to take their medications. Among the participants, an appreciable number (25%) reported missing one or more days of prescribed pills within the last two weeks and forgetting prescription while on vacation. About 16.7% endorsed stopping medications while asymptomatic or “feeling fine”. Around 65% used home monitoring devices, BP or glucose monitors, and 53.3% used some version of a medication dispensing device at home.
Mobile phone use
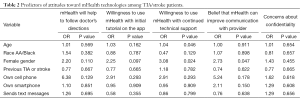
Mobile phone use was plentiful among the participants. An overwhelming majority (93.3%) owned a working mobile device and over a third (35%) owned a smartphone. Over half (53.3%) belong to households with at least one person owning a smartphone. Over 90% reported being comfortable with a cell phone. Almost all participants (97%) reported having a working cellular phone, over half (54%) had a working smart phone in their household and more than 75% send or receive text messages on their phone (Table 2). Participants demonstrated substantial access to computers with greater than 70% with a working computer, along with assistance if needed, in the home. 78.3% reported using mobile devices for text, 35% email, 43.3% for internet use, and 45% used the devices with other software applications.
Full table
Attitudes and willingness toward mHealth technology
Only a small group (16%) of the participants had previously heard of mHealth/telehealth. However, over 75% of participants would use a mHealth system if the device(s) were provided free of charge. A majority of patients checked “agree or strongly agree” to all questions evaluating their willingness and confidence in mHealth as alternative means of delivery for health communication. About 71.7% were willing to use a free “smart” device as directed if given assistance, 85% were comfortable with a nurse or doctor monitoring health information using mHealth, 78.3% believed mHealth would help them with medication adherence, specifically following doctor’s directions, 71.7% believed private health information would be protected via mHealth technology, and finally, 83.3% were confident this technology would be a means of effective communication between themselves and respective health providers.
No statistically significant differences in attitudes towards mHealth were observed in this sample based upon race, income, medication adherence, and use of smart phones or BP devices/medication boxes. When comparing participants based on whether they would or would not use a mHealth system, the majority (52%) of those who reported they would use the mHealth system had a household income of less than $30,000, compared to 44% in the group that would not use the device (P=0.01).
In ordinal logistic regression, gender was statistically significantly associated with a willingness to use mHealth if continued technical support was provided as well as with beliefs that mHealth could improve the communication with the health care provider (see Table 2). Females had 3.1 and 2.7 times the odds to strongly agree versus the combined remaining categories compared to males (P=0.24 and P=0.047, respectively). Age was also associated with the willingness to use mHealth with continued technical support. For a 1-year increase in age the odds to strongly agree increased by 4% (OR =1.04; P=0.046) compared to the remaining categories combined.
Discussion
This study indicates generally positive attitudes toward telecommunication and mHealth strategies in this small stroke subset. Given the demonstrated familiarity and prevalence of mobile phone use, participants appear equipped to quickly learn and adapt to the ongoing transformation of healthcare delivery systems, particularly telehealth.
Healthcare is changing and providers are eager to balance the increased need for personalized medicine, optimal medical management with limited time. The mobility, convenience, and popularity of cell phones provide an accessible and affordable target for the medical industry to exploit and use to improve patient care. Supporting patients in taking control of their medication management and the control of their BP may boost morale, adherence, and consistency with lifestyle changes. The greater perception of care due to increased, expedited responsiveness via mHealth may benefit the therapeutic relationship and enhance trust ties.
Mobile device use is high in this sample of stroke patients and they are amenable to mHealth for communication and assistance in adhering to their medical regimens. Since elevated BP is a major cause of stroke and secondary stroke, and lack of medication adherence is a major contributor to elevated BP, mHealth monitoring of BP and medications may help to reduce secondary stroke in this population. However, more research is needed to explore perceptions and assess potential usefulness of this technology in larger stroke populations.
Acknowledgements
Funding: This publication was supported with funding from the Medical University of South Carolina’s Telehealth Initiative and National Institutes of Health (NIH) grants U01 NS079179, U54 HG007479, R21 NS094033, and the South Carolina Clinical and Translational Research Institute, with an academic home at MUSC, through NIH Grant Number UL1 TR000062. The content does not represent the official views of NIH.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Medical University of South Carolina Institutional Review Board.
References
- Centers for Disease Control and Prevention, National Center for Health Statistics. Underlying Cause of Death 1999-2013 on CDC WONDER Online Database, released 2015. Data are from the Multiple Cause of Death Files, 1999-2013, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Available online: http://wonder.cdc.gov/ucd-icd10.html
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation 2015;131:e29-322. [Crossref] [PubMed]
- National Stroke Association. Take control of your health: preventing another stroke. Available online: http://www.stroke.org/we-can-help/survivors/stroke-recovery/first-steps-recovery/preventing-another-stroke
- Rothwell PM, Coull AJ, Giles MF, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 2004;363:1925-33. [Crossref] [PubMed]
- Luengo-Fernandez R, Gray AM, Rothwell PM, et al. A population-based study of hospital care costs during 5 years after transient ischemic attack and stroke. Stroke 2012;43:3343-51. [Crossref] [PubMed]
- Mohan KM, Wolfe CD, Rudd AG, et al. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke 2011;42:1489-94. [Crossref] [PubMed]
- Rutten-Jacobs LC, Maaijwee NA, Arntz RM, et al. Long-term risk of recurrent vascular events after young stroke: The FUTURE study. Ann Neurol 2013;74:592-601. [Crossref] [PubMed]
- Gaziano TA, Bitton A, Anand S, et al. The global cost of nonoptimal blood pressure. J Hypertens 2009;27:1472-7. [Crossref] [PubMed]
- James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507-20. [Crossref] [PubMed]
- Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957-67. [Crossref] [PubMed]
- Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol 2008;2:509-17. [Crossref] [PubMed]
- Logan AG, McIsaac WJ, Tisler A, et al. Mobile phone-based remote patient monitoring system for management of hypertension in diabetic patients. Am J Hypertens 2007;20:942-8. [Crossref] [PubMed]
- Scherr D, Kastner P, Kollmann A, et al. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation: randomized controlled trial. J Med Internet Res 2009;11:e34. [Crossref] [PubMed]
- Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemed J E Health 2009;15:231-40. [Crossref] [PubMed]
- Paré G, Sicotte C, St-Jules D, et al. Cost-minimization analysis of a telehomecare program for patients with chronic obstructive pulmonary disease. Telemed J E Health 2006;12:114-21. [Crossref] [PubMed]
- Quinn CC, Clough SS, Minor JM, et al. WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther 2008;10:160-8. [Crossref] [PubMed]
- Kauer SD, Reid SC, Crooke AH, et al. Self-monitoring using mobile phones in the early stages of adolescent depression: randomized controlled trial. J Med Internet Res 2012;14:e67. [Crossref] [PubMed]
- Vuong AM, Huber JC Jr, Bolin JN, et al. Factors affecting acceptability and usability of technological approaches to diabetes self-management: a case study. Diabetes Technol Ther 2012;14:1178-82. [Crossref] [PubMed]
- Seto E, Leonard KJ, Cafazzo JA, et al. Mobile phone-based telemonitoring for heart failure management: a randomized controlled trial. J Med Internet Res 2012;14:e31. [Crossref] [PubMed]
- Piette JD, Datwani H, Gaudioso S, et al. Hypertension management using mobile technology and home blood pressure monitoring: results of a randomized trial in two low/middle-income countries. Telemed J E Health 2012;18:613-20. [Crossref] [PubMed]
- Earle KA, Istepanian RS, Zitouni K, et al. Mobile telemonitoring for achieving tighter targets of blood pressure control in patients with complicated diabetes: a pilot study. Diabetes Technol Ther 2010;12:575-9. [Crossref] [PubMed]
- McGillicuddy JW, Weiland AK, Frenzel RM, et al. Patient attitudes toward mobile phone-based health monitoring: questionnaire study among kidney transplant recipients. J Med Internet Res 2013;15:e6. [Crossref] [PubMed]
- Price M, Williamson D, McCandless R, et al. Hispanic migrant farm workers' attitudes toward mobile phone-based telehealth for management of chronic health conditions. J Med Internet Res 2013;15:e76. [Crossref] [PubMed]
- Bharmal M, Payne K, Atkinson MJ, et al. Validation of an abbreviated Treatment Satisfaction Questionnaire for Medication (TSQM-9) among patients on antihypertensive medications. Health Qual Life Outcomes 2009;7:36. [Crossref] [PubMed]
- Morisky DE, Ang A, Krousel-Wood M, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348-54. [Crossref] [PubMed]
Cite this article as: Jenkins C, Burkett NS, Ovbiagele B, Mueller M, Patel S, Brunner-Jackson B, Saulson R, Treiber F. Stroke patients and their attitudes toward mHealth monitoring to support blood pressure control and medication adherence. mHealth 2016;2:24.


