The Baby Bites Text Messaging Project with randomized controlled trial: texting to improve infant feeding practices
Highlight box
Key findings
• Current parents of infants view breastfeeding positively and want practical information from their infant’s healthcare provider about how to feed their infants;
• A 12-month text messaging feeding intervention based on the Health Belief Model did not result in less obesity or improved feeding practices among parents of infants.
What is known and what is new?
• Providing extra support for parents of infants to feed their infants in healthy ways can help them adopt healthier feeding practices. Inexpensive and accessible ways of providing this support are needed;
• This education-only approach was not effective in this small sample of mostly low-income parents.
What is the implication, and what should change now?
• mHealth-based means of providing parent support for healthy feeding practices are needed but may need to involve parent support;
• Delivery of m-Health strategies needs to be flexible because parents may lose/change cell phone service.
Introduction
Background
Children with obesity are more likely to become adults with obesity and associated health problems (1,2). In addition, pediatric obesity is associated with increased comorbidities, including hypertension, dyslipidemia, type 2 diabetes mellitus, nonalcoholic fatty liver disease, and psychosocial problems (1,3,4). Despite attempts to reduce pediatric obesity, rates continue to rise (5), and disparities have widened, with lower income groups showing worsening trends (6). Rapid weight gain in infancy is associated with childhood obesity (7-9). In one US study, more than half of overweight or obese children were overweight by age two, with average onset of overweight between 15–22 months (10). However, while modifiable risk factors for childhood obesity are present before birth and during infancy (11), the majority of pediatric obesity prevention interventions involve older children (11-14).
Approaches to prevent obesity in infancy have varied, ranging from enhanced pediatric well visits (15-18) and group visits (19), to home visits (20,21), dietitian visits (22), and even handouts (23) and posters (24). Some studies have demonstrated improved feeding practices (15,16,23,24). Slightly lower weight-for-length z scores, body mass index (BMI) percentiles, or prevalence of overweight have been found in others (19-21,24). However, limitations of these studies include little consistency regarding method, length, and intensity of intervention (15,19-25) and lack of grounding in health behavior theories (15,19,20,25). Thus, there remains a pressing need for data on best practices in preventing early pediatric obesity as well as obesity prevention interventions that are low cost, theory-based, and parent-informed.
Pediatric primary care is an ideal setting for obesity prevention efforts because infants have frequent appointments with their pediatric healthcare provider during the first year. In addition, primary care providers may influence parent feeding practices because of their position of authority (26). However, promoting healthy feeding practices is challenging due to barriers to effective communication (26) and the impact of conflicting advice from family and friends (27). While qualitative research can help uncover parental attitudes towards feeding (28-33) and risk for early obesity (34) to help address influences of feeding practices, few recent qualitative studies have involved diverse US populations. In addition, parent attitudes towards feeding and communication change with each new generation of parents (35).
Rationale and knowledge gap
Mobile health (mHealth), including text messaging, may be one cost-effective approach to influence early feeding decisions and prevent early obesity. However, there have been few mHealth initiatives to address infant feeding (36-40). Existing interventions have been limited by lack of rigorous data analysis (36) and limited publications on feeding outcomes (37-39). However, because mHealth breastfeeding promotion efforts have been shown to improve breastfeeding rates (40), there is potential to use this method to promote healthy feeding practices to reduce risk of early weight gain and obesity.
Objective
The purpose of this mixed methods project was two-fold:
- Explore attitudes of current generations of parents of newborns towards feeding, early obesity, and communication with their infant’s healthcare provider;
- Use these qualitative results to develop and conduct a pilot randomized controlled trial (RCT) to compare the efficacy of theory-informed text messages to usual primary care to prevent early pediatric obesity (the Baby Bites Text Messaging Project).
The primary aim of the RCT was to compare the impact of text messages versus usual pediatric nutrition care on weight-for-length percentiles and z scores at 2–4, 6–9, and 12 months. The secondary aim was to compare the effect of theory-based text messages versus usual pediatric nutrition care on feeding practices of infants at 2–4, 6–9, and 12 months. This manuscript was written following the COREQ and CONSORT reporting checklists (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-31/rc).
Methods
Mixed methods design
This mixed methods study involved a sequential, exploratory design. Parents of infants were recruited to participate in interviews in order to determine their attitudes towards early pediatric obesity, feeding practices, and receiving information from their providers. This information was used to choose the Health Belief Model (HBM) as a theory to inform an intervention. Then, a survey was used to test gain versus loss framed text messages on feeding topics targeting constructs of the HBM (41). Finally, the qualitative and survey data were used to develop the intervention.
Qualitative study of parent attitudes
We used a general qualitative approach to conduct a phenomenological analysis to explore the thoughts and perceptions of parents of infants in a diverse, urban community in Ft. Worth, Texas, USA regarding infant feeding, causes of early pediatric obesity, and receiving feeding information from their infant’s healthcare provider using focus groups and interviews.
The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of Texas Woman’s University (No. 00000829), and informed consent was taken from all individual participants.
Study setting and participants
During spring 2018, we recruited participants from the UNTHSC Pediatric Clinic, an urban, teaching clinic. This clinic serves a population that is primarily low income, with the majority of patients being covered by Medicaid. Eligibility criteria included: being a parent of a healthy, term infant; establishing care for the infant with a clinic healthcare provider in the first 30 days of life; at least 18 years of age; and able to understand and speak English. Researchers used purposive recruiting methods to seek participants of varying ages, race, and ethnicity. Recruitment methods included flyers and verbal invitations to parents of infants in the clinic waiting room. Due to longer than usual clinic wait times, focus groups of at least 3 were not always possible. Thus, parents were interviewed singly or in groups of 2–3 in a clinic conference room. More than 30 participants were invited to participate, but half or more did not agree to be screened due to time constraints, lack of interest, or hesitance to be recorded. This is an estimate; exact numbers for those declining to participate were not recorded.
Focus group interview guide
The primary investigator (PI) (first author) wrote the qualitative interview questions, and a research staff member with qualitative research expertise edited the questions to minimize leading questions and bias (Table 1). The script was not pilot tested. The PI was a female, registered dietitian nutritionist (RDN) with a PhD and pediatric nutrition expertise and no prior relationship with the participants. The PI conducted the interviews in English, and the student investigator (second author) acted as the co-moderator and note taker. Older children of the participants were sometimes present, and an additional student was available to help keep the children entertained. Each interview was recorded using two digital recorders. The PI asked the questions, listened to the answers, and verbally summarized comments for clarity. Interviews took approximately 30 minutes to complete. Participants knew the purpose of the research was to inform an intervention and knew the PI’s role and training. Afterwards, the research team held a debriefing session to discuss emerging themes, compare the interviews/groups to previous sessions, and determine any needed changes in approach. Because of the difficulty of arranging interviews for parents of newborns, no follow-up interviews were conducted.
Table 1
| What are your thoughts about breastfeeding your baby? |
| What are your thoughts about using formula to feed your baby? |
| Tell me your thoughts on when the best time is to begin feeding your baby something other than breastmilk or formula |
| What types of foods do you think are the best to begin feeding your baby? |
| What do you think about offering your baby sweetened foods or drinks? |
| What do you think might cause some babies or children to become overweight? |
| What information would you like to receive from your healthcare provider about feeding your baby? |
| What are your thoughts about receiving information about feeding by text messaging? |
Analytic approach
Interviews were transcribed verbatim by the second author using NVivo12 Pro for Windows (QSR International, Victoria, Australia). Transcripts were not returned to participants for comment or correction. After half the interviews were transcribed, the first coder (second author) analyzed the data using open coding. A second coder (first author) then reviewed the codes. After coders reached consensus, they revised the original codes. Then the first coder (second author) coded the remaining transcripts. The second coder independently coded approximately half of the transcripts using the same code sets and after discussion, added a few codes. The first coder then re-evaluated the transcripts for final coding changes. After coding, the first and second authors sorted data into categories in order to identify themes. Then a comparative pattern analysis was completed to confirm themes. No new themes were identified in the analysis of the final transcripts. Therefore, it was determined that recruitment of additional participants was unnecessary as data saturation was reached. While the researchers summarized the interviews to each parent or small group of parents, we did not share the themes and sub-themes for feedback.
Pilot, RCT study
Recruitment
We recruited participants for the RCT from the same UNTHSC Pediatric Clinic during fall 2018 to spring 2019 via flyers and pediatric caregiver invitation. Data collection was completed by August 2021. Eligibility criteria included: being a parent of an infant aged 3–30 days with no special medical conditions or prematurity, at least 18 years of age or older, and having access to a mobile phone with Internet access. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of the University of North Texas Health Science Center (No. 00000702), and informed consent was taken from all individual participants.
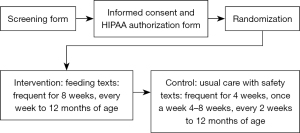
In the clinic waiting room, each parent provided informed consent, then completed a form providing demographic information, their mobile phone number, and their child’s date of birth. Participants were randomized to the feeding text messaging (intervention) group or usual nutrition care with infant safety text messaging (car safety, sun safety, etc.) (control). The PI, who is the first author used a computerized random number generator to create two sets of 20 study ID numbers between 50 and 150. Then the PI printed these numbers on slips of paper and wrote “intervention” or “control” on 20 of each. She drew 10 slips from each control or intervention set to place in opaque envelopes labeled “boy” and 10 in the envelopes labeled “girl”. She then sealed the envelopes, shuffled them, and sequentially numbered the “boy” and “girl” sets. As the PI or grant staff (graduate assistants or research coordinator) consented each eligible parent, they asked the sex of the infant, then chose the next sequentially numbered envelope, and opened it to reveal the group assignment. Following assignment, the research staff enrolled the parents into the correct text messaging study group (breastfeeding, formula feeding, or control) using the parents’ mobile phone numbers. To complete enrollment, participants accepted an initial text message. Due to the nature of the intervention, participants could not be blinded to their group. Also, due to the need to ensure participants were receiving the correct messages, the PI could not be blinded to group assignment. However, when data on weight and length were collected and dietary recalls were collected, data collectors were blind to group assignment. Care providers were unaware of research participation status or group assignment.
Intervention
Based on the findings from the qualitative analysis and a follow-up survey evaluating clinic parents’ text messaging preferences (41), intervention participants received short (typically fewer than 160 characters) gain-framed text messages (42). Gain-framed messages emphasize the benefits of adopting a health behavior or practice rather than the negative consequences of not adopting the behavior (42).
The messages targeted the HBM concepts of perceived benefits, perceived barriers, self-efficacy, and cues to action (43) regarding healthy feeding practices. This theory was chosen based on the analysis from the qualitative data (presented in the results). The intervention group received text messages with feeding advice four times per week for the first 4 weeks of study enrollment, decreasing to twice a week by 5 weeks, and once a week from 8 weeks to 12 months of age. The control group received safety messages twice a week for the first 4 weeks, once a week from 5 to 8 weeks, and every 2 weeks for the remainder of the study (up to 12 months of life). While preliminary research with parents suggested they preferred receiving messages once a week, the research team felt one message a week would be unlikely to provide adequate support to promote changes in breastfeeding adherence. Thus, parents received more frequent messages in the first few weeks, decreasing to one message per week at the 8-week mark. In addition to text messages, all participants received the clinic’s handouts including feeding and general infant safety advice (see Figure 1 for the flow of participants through the study; see Table S1 for sample texts).
Intervention parents who were breastfeeding received messages promoting and supporting breastfeeding. Formula-feeding parents received messages intended to provide cues to action regarding appropriate feeding practices and timing and to promote feeding self-efficacy. At about 6 months of age, parents received a text to enroll in the introduction to solid foods group. A service called Healthy-Txt (Columbus, OH, USA) delivered the texts.
The PI and a student with an Master of Science (MS) in Nutrition developed the gain-framed text messages. A subset of the messages was piloted with parents via a survey (41). After receiving parent feedback, the PI and MS Nutrition student developed additional messages in the same style as the piloted messages. Then another nutrition professor and dietitian with special expertise in nutrition education, a pediatric dietitian, a pediatrician, and a communications professor specializing in feeding reviewed and revised the messages. Some messages contained links to a web page where parents could read content with more information on feeding advice. The web pages also contained links to external web pages with additional information or videos related to feeding and infant nutrition care.
The control group received usual care—handouts from the American Academy of Pediatrics about safety and feeding. They also received safety-related text messages, which were developed by Healthy-Txt (Columbus, OH, USA) for another project. These aimed to help control for any effect of receiving any health-related texts on the outcomes of interest (see Table S2 for the safety-related texts).
Data collection
The researchers gathered demographic data at baseline. All other data was collected between 3–30 days, 2–4 months, 6–9 months, and 12 months of the infant’s age, including weight and length, which were used to generate the primary outcome measures: weight for length percentiles and z scores. Data from 24 hour recalls and feeding surveys were used to evaluate the secondary outcomes measures: feeding practices such as breastfeeding and introduction of solids. The range was flexible so that parents who missed attending a scheduled visit or did not reply to a survey text could still participate within the interval. To track anthropometric measurements, the researchers had permission to access each infant’s electronic health record to gather weights and lengths. If the child had measurements occurring within the 2–4 or 6–9 months interval, we noted these with the infant’s age at the time of measurement. The weight-for-length percentile and z-score were determined by putting this information into the World Health Organization’s Anthropometric Calculator application (version 3.2.2; Geneva, Switzerland). Due to the coronavirus disease 2019 (COVID-19) pandemic, no 12-month measurements were available.
Feeding practices assessment
To assess infant feeding practices, parents received a text with a link to an online survey in PsychData (State College, PA), adapted from the National Health and Nutrition Examination Survey (NHANES) Diet Behavior Nutrition Questionnaire, including questions regarding breastfeeding, formula feeding, introduction of solids, and sugar sweetened beverages (44). The PI sent the survey link to participants at enrollment (0–30 days of the infant’s life) and between 2–4 months, 6–9 months, and 12 months of the infant’s age, with follow-up reminders up to twice. The NHANES questions address whether breastmilk was fed and when it was stopped, with similar questions about formula and other foods or beverages (44). Researchers also called participants at each time point to obtain 24-hour recalls as another method to assess breastfeeding and other feeding practices.
Statistical analysis and data monitoring
Descriptive statistics for all continuous variables split by group are displayed in Table 1. Independent samples t-tests were used to examine if there were differences between the treatment and control group on demographics, and χ2 were used for categorical variables.
All participants were included in statistical analyses. A linear mixed model utilizing a heterogeneous covariance structure was conducted to examine how weight for length changed over the three time points between the two groups. This approach was appropriate as there was an increased amount of missing data at the second and third time points. We used repeated measures analysis of variance (RM ANOVA) and repeated measures analysis of covariance (RM ANCOVA) to compare feeding practices (breastfeeding, introduction of solids). All data were analyzed using IBM SPSS (version 25, Armonk, NY). Statistical significance was set at α=0.05. An a priori power analysis was conducted to determine the minimum sample size required to find statistical significance for RM ANOVA. With a moderate effect size (f=0.25) and power set to 0.80, results indicated that a 2 (group) ×3 (time) RM ANOVA would require a total of 37 participants (including a 30% dropout rate). Based on the study of Gallegos et al. (40), who found a significant difference in breastfeeding rates using a text-messaging intervention, we expected to find similar improvement in the outcomes of interest. Effect sizes were not described in this study; thus, we estimated a moderate effect size.
Results
Qualitative study
Participants
Fifteen parents (10 mothers, 5 fathers) participated in the qualitative portion of the study (mean age: 26.1±7.3 years). Approximately 87% of parents spoke English as the primary language at home (Table 2). Qualitative analysis revealed six sub-themes: breastfeeding, attitudes about introducing solids, feeding opinions, problems related to feeding or parenting, information through text messaging, and receiving information. From these sub-themes, we identified two overarching themes: parental attitudes about feeding or parenting and parental preferences about feeding information (Table 3). No minority themes were identified.
Table 2
| Characteristics | Frequencies |
|---|---|
| Sex, n [%] | |
| Male | 5 [33] |
| Female | 10 [67] |
| Age (years), mean ± SD | 26.1±7.3 |
| Race/ethnicity, n [%] | |
| Non-Hispanic, White | 3 [20] |
| Non-Hispanic, Black | 6 [40] |
| Hispanic/Latina | 5 [33] |
| More than one | 1 [7] |
| Primary language, n [%] | |
| English | 13 [87] |
| Spanish | 2 [13] |
| Other languages spoken, n [%] | |
| English | 2 [13] |
| Spanish | 2 [13] |
| Hawaiian | 2 [13] |
| Number of children in household, n [%] | |
| 1 | 2 [13] |
| 2 | 7 [47] |
| 3 | 3 [20] |
| BMI (kg/m2), mean ±SD | |
| Male | 34.0±10.1 |
| Female | 29.4±4.9 |
BMI, body mass index; SD, standard deviation.
Table 3
| Themes | Sub-themes | Codes |
|---|---|---|
| Parental attitudes about feeding or parenting | Breastfeeding | Attitudes about breastfeeding |
| Breastfeeding barriers | ||
| Breastfeeding benefits | ||
| Attitudes about introducing solids | Best age to introduce solids | |
| Best foods to introduce solids | ||
| How solids should be introduced | ||
| Introduction of solids by family members | ||
| Reasons to start introducing solids | ||
| Feeding opinions | Attitudes about feeding with formula | |
| Feeding style & responsive feeding attitudes | ||
| Attitudes about introducing SSB or foods | ||
| Signs a baby is hungry | ||
| Problems Related to Feeding or Parenting | Causes of picky eating | |
| Causes of early overweight or obesity | ||
| Parental preferences about feeding information | Information through text messaging | Information interested in receiving via text |
| Attitudes about receiving feeding information by text message | ||
| Preferred time and frequency to receive text messages | ||
| Receiving information | Information wanted from healthcare provider | |
| Preferred learning style | ||
| Sources of information |
SSB, sugar-sweetened beverage.
Parental attitudes about feeding or parenting
Overall, parents viewed breastfeeding positively (Table 4). Several parents identified specific benefits, such as breast milk’s nutrient content and its immunological benefits. Parents also noted differences in responsive feeding with breastfeeding versus formula feeding. For example, they expressed that because breastfeeding is “natural”, it is easier to know when the infant has had enough than when feeding with formula. Therefore, they felt this was another benefit to breastfeeding.
Table 4
| Themes | Illustrative quotes* |
|---|---|
| Parental attitudes about feeding or parenting | “I heard it (breastfeeding) helps with the hormones, or it helps keep the hormones in check for mom. And then shrinks your uterus faster and helps you burn calories and stuff so all those are good things.” P9 |
| “It (breastfeeding) helps with the baby’s immune system.” P7 | |
| “When we’re out I do give it to her because I’m not really comfortable yet with breastfeeding in public like with other people around.” P3 | |
| “I think you should breastfeed, I’m not because it takes a lot of time and energy and my milk didn’t come in and I would have to pump like every two hours and I’m trying to finish the school semester right now so I kinda need the extra time and energy.” P9 | |
| “I personally like it (formula) because…it’s just really quick and easy to pour and shake and put it in her mouth and to me that’s easier.” P8 | |
| “I’ve heard that your body naturally knows how much to feed the baby. Sometimes I’m worried I’m overfeeding him or sometimes he’s not hungry, he just needs to burp.” P9 | |
| “From what I’ve read is when you start early with table foods then that leads to obesity.” P2 | |
| Parental preferences about feeding information | “I would like to know when to feed more.” P8 |
| “We really want to know more on breastfeeding and the effects that it has.” P7 | |
| “The patience, the feeding, sleeping habits like get your rest when the baby is sleeping. Like diapers because some parents don’t know how often they should use the bathroom.” P5 | |
| “I like the more visual approach. I like to read and see the breakdown and the research and the study and the facts.” P2 |
*, P + number denotes participant number.
Whereas the overall view of breastfeeding was positive, parents also noted several barriers, such as discomfort about breastfeeding in public; confusing messages from healthcare providers; pain while breastfeeding; latching issues; and scheduling, time, and energy constraints (Table 4). Parents preferred breastfeeding to formula feeding but did not imply that feeding with formula was unhealthy. Parents of infants mostly agreed that formula is useful if there is limited time or there are latching problems. The main reason parents chose to feed formula instead of breastfeeding was due to the convenience of formula feeding and barriers to breastfeeding: “I personally like it because…it’s just really quick and easy to pour and shake and put it in her mouth and to me that’s easier.”
When asked their opinions concerning the best age to introduce solids, most parents identified 6 months. Most felt fruits and vegetables were ideal first foods. Parents also expressed the desire to introduce solids to keep the infant full longer or because their infant did not seem to be getting full. In referring to prior experiences with their other children, many participants shared frustration regarding the introduction of solids by their extended family members. They expressed that family members were more likely to feed their infant something they did not want them to have: “They’re old-fashion and say, ‘Well we did it back then and you are alive and you didn’t die. (sic)’ And I’m like, yeah we’re here, but we’re overweight.”
Parents attributed causes of early pediatric obesity and picky eating to problems with feeding or parenting. A majority of participants thought parents were mostly responsible for picky eating behaviors among their children. Lack of exposure to new or healthy foods was discussed as a reason why children grow up to be picky or unhealthy eaters. Parents also linked early obesity to early introduction of solids: “From what I’ve read is when you start early with table foods, then that leads to obesity.” They also mentioned unhealthy foods provided by parents or grandparents: “Their moms and grandparents giving them everything they want.” Parents also mentioned lack of healthy foods and exercise due to time, energy, and/or budget constraints. They also noted other factors that can lead to early overweight or obesity, such as genetics, children having to finish their plate, or overfeeding children.
Parental preferences about feeding information
Most participants expressed a desire for more information from their infant’s healthcare provider concerning feeding. They wanted more information on topics such as what to feed when, how to start solids, and how much to feed: “I would like to know when to feed more.” Parents also expressed diverse opinions on how they wanted to receive information: “I like the more visual approach” versus “I want to read it, and I want to believe it for myself. I’m not saying I don’t trust the doctors, but I want to be able to read for myself.” In addition, parents expressed positive attitudes toward receiving feeding information via text. Parents preferred to receive information about topics such as introducing solids, increasing feeding, and breastfeeding versus formula feeding (e.g., “How often am I supposed to increase her feeding?”).
Pilot, randomized, controlled trial: the Baby Bites Text Messaging Project
Formation of the pilot study
The formative, qualitative data informed the intervention. Parents participating in the interviews desired practical information from their pediatricians and also wanted convenient information. Consequently, the RCT provided practical information for parents via text. In addition, because parents in the qualitative study seemed well aware of breastfeeding benefits but mentioned communication barriers, only a few messages focused on benefits of breastfeeding. Instead, more messages focused on issues such as what to do if breastfeeding is painful, how to recognize and respond to hunger and satiety cues, how to manage breastfeeding in public, or what to do if you need to take medications. In addition, parents had misconceptions about reasons for starting solids, such as identifying solids as a way to keep the baby full instead of noting the importance of helping a child accept new flavors or introduce iron-rich foods at an important stage. Thus, text-messages emphasized repeated offering of new flavors and careful introduction of textures. Most parents recommended starting first foods with fruits and vegetables, whereas practice guidelines suggest iron-rich foods (e.g., fortified infant cereals or pureed meats) should be first. Consequently, text messages made suggestions for iron-fortified cereals or pureed meats as first foods. These were designed to focus on addressing perceived barriers, building self-efficacy, and providing cues to action, which are constructs of the HBM.
Participants
Participants (n=44) were recruited and consented to participate in the RCT; however, six never accepted the text message invitation to enroll. Thus, the initial sample size for the study was 38 participants (control =17; intervention =21). Furthermore, two participants in each group unsubscribed, and six (three in each group) were lost during following-up over the course of the study due to changes in phone number or loss of cell service. This resulted in the final sample size of 28 (control =12; intervention =16); however, all randomized participants were used in the intent to treat analysis (see Figure S1 for the flow of participants).
Participants were balanced in terms of numbers of parents of male vs female infants, parent age and BMI (based on self-reported height and weight), number of children in household, and participation in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) (Table 5). The intervention infants had lower mean birth weight at baseline, t[35] =2.25, P=0.031, d=0.74. Birth weight for length percentiles and z-scores were not significantly different, t[24] =1.70, P=0.10, d=0.67. There were only two fathers in the control group and no fathers in the intervention group. There was a higher percentage of white participants in the control group compared to intervention (35.3% versus 14.3%) and a higher percentage of Hispanic parents in the intervention group compared to control (61.9% versus 41.2%).
Table 5
| Characteristics | Control (n=17) | Intervention (n=21) | Significance |
|---|---|---|---|
| Infant characteristics | |||
| Infant gender, n (%) | 0.74 | ||
| Girls | 8 (47.1) | 11 (52.4) | |
| Boys | 9 (52.9) | 10 (47.6) | |
| Birth weight (kg), mean ± SD | 3.43±0.57 | 3.11±0.30 | 0.03 |
| Birth weight/length percentile, mean ± SD | 57.5±33.7 (n=13) | 35.8±26.3 (n=13) | 0.08 |
| Parent/household characteristics | |||
| Parent age (years), mean ± SD | 27.1±7.5 | 26.7±4.5 | 0.84 |
| Parent gender, n (%) | 0.11 | ||
| Fathers | 2 (11.8) | 0 (0) | |
| Mothers | 15 (88.2) | 21 (100.0) | |
| Parent race/ethnicity*, n (%) | 0.31 | ||
| White | 6 (35.3) | 3 (14.3) | |
| Black | 4 (23.5) | 3 (14.3) | |
| Hispanic/Latinx | 7 (41.2) | 13 (61.9) | |
| Asian | 0 (0) | 2 (9.5) | |
| Other | 1 (5.9) | 0 (0) | |
| Parent BMI (kg/m2), mean ± SD | 29.1±5.3 | 30.3±5.6 | 0.50 |
| Number of children in household, n (%) | n=20 | 0.84 | |
| 1 | 4 (23.5) | 6 (28.6) | |
| 2 | 7 (41.2) | 8 (38.1) | |
| 3+ | 6 (35.3) | 6 (28.6) | |
| Enrolled in WIC, n (%) | n=15 | n=17 | 0.27 |
| Yes | 5 (29.4) | 9 (42.9) | |
| No | 10 (58.8) | 8 (38.1) | |
*, parents were allowed to select all race/ethnicity categories with which they identified. Only one chose more than one. BMI, body mass index; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children; SD, standard deviation.
Weight-for-length z-scores and percentiles
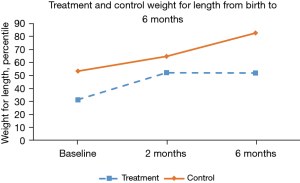
Results indicated that there was a significant main effect of time, F(2, 43.03) =3.26, P=0.04, as well as a significant main effect for group, F(1, 34.47) =6.90, P=0.01. The test for interaction effects between time and group was not statistically significant, P=0.18. By examining marginal means, it was clear that the full sample increased in birth weight for length percentile at each time point (Figure 2). Likewise, the control group had higher weight for length percentile across all time points (Figure S2 for weight for length percentiles over time).
Feeding practices
An analysis of breastfeeding practices over time using Pearson’s χ2 was not possible due to expected counts being less than expected (that is, there were not enough responses to the surveys at each time point). Pearson’s χ2 for the 6–9-month time point also did not indicate an impact of the intervention on breastfeeding, χ2[1] =1.45, P=0.23. Table 6 presents the trends in breastfeeding for both groups, indicating that the intervention group had slightly higher raw numbers breastfeeding at 6–9 and 12 months. However, the difference at 12 months was also not statistically significant, χ2[1] =0.24, P=0.63.
Table 6
| Group | Baseline, n (%) | 2–4 months, n (%) | 6–9 months, n (%) | 12 months, n (%) | Mean time breastfeeding (months), mean ± SD |
|---|---|---|---|---|---|
| Control (n=17) | 16 (94.1) | 11 (64.7) (n=16) | 6 (35.3) (n=17) | 2 (11.8) (n=16) | 4.53±4.4 (n=16) |
| Intervention (n=21) | 19 (90.5) | 14 (66.7) (n=20) | 10 (47.6) (n=18) | 3 (14.3) (n=19) | 4.99±4.1 (n=19) |
*, the “n” in parentheses indicates the number of participants responding to the survey and/or recall from which breastfeeding status was determined. SD, standard deviation.
Regarding initiating foods besides breastmilk or formula, 14 participants (control =6; intervention =8) reported age of first feeding solids in the 6–9 or 12-month survey. The age of first feeding of solids ranged from 5 to 9 months with a mean of 6.3 months for the control group and 6.5 months for the intervention group. In the control group, one participant reported having offered sugar-sweetened beverages (SSBs), while in the intervention group four participants denied having done this. Statistical significance was not calculated as there were only five participants that answered this question (one in control; four in treatment). For the person answering “yes” to offering SSBs, they admitted to offering more than sips or a few ounces on occasion. In summary, surveys and 24-hour recalls for breastfeeding and other feeding practices were not available for all participants at all time points, making the number of responses variable at each time point (see Table 6).
Discussion
Key findings
This mixed methods study involved a qualitative assessment of a diverse sample of parents’ thoughts and attitudes towards early obesity and feeding practices and an assessment of how and what information parents would like to receive from their infant’s healthcare provider. Based on key themes from the interviews, we developed a pilot-RCT to test the efficacy of text messages to promote healthier feeding practices and prevent early obesity. This is the first US study reporting a theory-based and parent-informed text-messaging initiative to influence parent feeding practices to reduce risk of early obesity in a diverse, lower socioeconomic status (SES) population of parents seeking well child pediatric healthcare.
Strengths and limitations
Limitations of the qualitative research include the small sample of parents participating in the interviews. In addition, because few parents agreed to participate in the interviews/focus groups due to issues such as time constraints, there was a high probability of selection bias. Finally, few first-time parents were in this group. This more experienced group of parents may have had more knowledge about infant feeding and obesity risks. However, a strength of this study was the diversity of the participants. A high percentage were Black and Hispanic/Latina/o parents (40% and 33%, respectively), which is similarly diverse to the clinic population later participating in the text-messaging intervention.
The RCT portion of the current study was also limited by small sample size. The number of participants needed for adequate power was recruited; however, due to low response rates for surveys sent via text link, the amount of data available at each time point was significantly lower than expected. Although the actual dropout rate (approximately 19%) was lower than expected, the poor response rate to on-line surveys and phone calls greatly reduced the power of the study to detect differences in groups. Moreover, the lack of 12-month data points due to the COVID-19 pandemic contributed to these limitations. Phone number changes and discontinuation of cell phone service also limited the study. Even for participants who did not drop out of the study, the research staff sometimes could not contact the participant for several weeks due to interruptions in their service. These issues may be anticipated in many low-income populations, limiting the usefulness of mHealth on its own as a health behavior change strategy unless there are alternate means of communication. In addition, we were unable to blind participants to their group assignment because of the nature of the study involving education, in which participants knew the type of education they were receiving via text, which could influence outcomes. Generalizability of this study’s findings may be limited because of the lack of power and the specific diversity characteristics of this population in a single pediatric clinic in Texas, USA. Strengths included measuring feeding practices over the course of the year, the inclusion of a diverse population with high WIC use, and the careful development of the study intervention.
Comparison with similar research
The formative, qualitative study indicated some parental thoughts about feeding were similar to prior qualitative studies, while other opinions were different. Most parents attributed causes of pediatric overweight to improper nutrition, including starting solids too early, a tendency to feed infants sweet foods, or not introducing fruits and vegetables. These findings are similar to a study examining parental perceptions of childhood obesity in a group of Canadian parents in which parents believed a healthy diet and physical activity were important factors in preventing obesity (45). However, unlike an early study on maternal feeding practices and childhood obesity in which mothers expressed frequent concern that their babies were not getting enough food and the belief that bigger babies were healthier (28), participants in this study did not express concern over whether their infants were getting enough, nor did they mention the desirability of having larger babies. In the present study, most parents seemed aware that feeding strategies promoting finishing meals could promote pediatric obesity.
Explanation of findings
Despite careful development of the text messaging intervention, there were no positive findings in terms of changes in weight-for-length percentile or z-score, the primary targets of the intervention. In addition, there were no positive changes in breastfeeding duration, frequency of offering SSBs, timing of introduction of solids, or first foods. Because this study targeted these outcomes, these findings were unanticipated. A couple of key issues may have contributed to the lack of improvements. First, higher rates of parents in this study were breastfeeding at baseline (over 90% for each group), with approximately two-thirds still breastfeeding at 2–4 months (Table 6), compared to US averages of approximately 84% of women ever breastfeeding and 46.9% exclusively breastfeeding at 3 months (46). Thus, this sample’s breastfeeding rates were higher than the national and state averages at baseline and 2–4 months, making improvement challenging. However, breastfeeding persistence in this study’s groups was lower compared to national averages at 6 months (30% for the study versus 58% US) and 12 months (14% for the intervention group and 11% for the control versus 36% US). This leads to a second potential contributor to lack of positive outcomes. Although income data was not gathered, 29% of the control participants and 43% of the intervention group were enrolled in WIC, an income-based program. In addition, nearly 65% of the control group and 86% of the intervention group identified as being non-white. Breastfeeding persistence has been shown to be lower in infants from lower-income households and in Mexican-American and Black infants (47), which likely relates to the need for mothers to return to work soon after giving birth in lower income populations, with lower income mothers being more likely to be Mexican-American or Black (47). The intervention group in this study had a lower raw percentage of white participants, who often have higher breastfeeding persistence.
Similar to the present study’s results, Taveras et al., conducted a small study (n=80) comparing interventions involving pediatricians alone to a health educator intervention and group parenting workshops and found no differences in breastfeeding practices or responses to satiety cues (15). Other studies in pediatric well care have found significant changes in breastfeeding. For example, Gross and colleagues were able to demonstrate increases in exclusive breastfeeding and reduced use of complementary foods and liquids in a group of over 500 3-month-old infants (48). Schroeder et al. were also able to demonstrate improvements in SSB offering and delayed offering of cow’s milk in parents receiving additional advice during pediatric well visits (18). In the present study, surveys were sent via text link to parents, who often did not complete them. Thus, whereas other larger studies of feeding interventions have shown benefits for breastfeeding or other feeding practices (18,49), this smaller study, with limited data at the time points measured, found none.
Other trials have assessed impact of various interventions on BMI percentile, obesity frequency, or BMI z-score, with varying results. In PROBIT, a trial to prevent obesity in around 500 Italian toddlers, there were no differences in obesity among children receiving additional educational materials during well child visits (16). In contrast, in a small study of 47 parent-child parents in the Bronx receiving well child group visits, Machuca et al. showed infants in the intervention group were less likely to be overweight or obese at two years compared to control participants (19). Paul and colleagues found lower weight-for-length percentiles at age one year in infants who had been randomized to receive an education intervention during which parents learned about hunger and satiety and how to deal with introducing solids plus an intervention to learn about soothing infants with strategies other than feeding (20). In contrast, another study seeking to teach pregnant women about breastfeeding, healthy feeding, and good sleep strategies found no differences in BMI percentile at 24 months in the offspring (17). These variable results may reflect that including social support (19) and intensive interventions that train parents about responsive feeding (20) are more effective than studies such as ours, which primarily involved education without social support.
Implications and actions needed
Based on our findings, we believe future interventions aimed at influencing infant feeding practices using mHealth should involve elements of social support. Survey-based data should be gathered in person. In addition, the intervention needs to be flexible so that parent contact can be maintained if they lose or change cell service.
Conclusions
In summary, this intervention, while carefully developed and informed by both parent input and selection of an appropriate HBM on which to base the intervention, found no improvements in early pediatric obesity or feeding practices. While the results were unanticipated, text messaging may still hold promise as a mechanism that can extend communication with the provider beyond office visits. The current study was underpowered to detect a difference in the groups due to participant inconsistency in answering surveys and attending healthcare appointments, and the lack of 12-month data due to COVID. In addition, the number of parents breastfeeding was slightly higher in the intervention group, suggesting that a study with better adherence to data collection may have found an improvement in breastfeeding rates.
Studies indicate text messaging may be a quick and cost-effective method to communicate important nutrition or health information, particularly with populations with higher health risks or more in need of support (50,51). Because risk for early obesity is present even prior to infancy due to differences in parental obesity and other factors, health professionals should consider implementing future interventions during pregnancy or in populations who may become pregnant and extend through age two or pre-school age, as many children become obese by this time. In addition, while text messaging is a promising avenue, other mHealth interventions, including online support groups through social media platforms, may also need to be considered, along with easily accessible content through platforms used by younger adults, including TikTok, Instagram, and others. In addition, if survey or dietary intake data is needed, gathering it in person at medical appointments would likely be a better approach, given the difficulty of contacting parents of infants, especially lower income parents.
Rising rates of pediatric obesity and consequences of pediatric obesity in later life (2,4) indicate the need for new, innovative pediatric obesity interventions. Infancy is a significant point of intervention and warrants more research with a focus on finding cost-effective interventions that may be widely implemented among diverse populations.
Acknowledgments
We want to thank Madhavi Kaluva, MS, for assisting in developing the text messages and recruiting participants, and collecting 24-hour recalls. We also wish to acknowledge Leah Zimmerman for recruiting participants and collecting patient weights and lengths. Finally, we thank Lona Sandon, PhD, RDN, LD, Kimberly Mory, PhD, CCC-SLP, and Kathleen Eustace, MPH, RDN, LD for their assistance in evaluating the text messages and web landing page content.
Funding: This work was supported by the Texas Woman’s University Research Enhancement Program.
Footnote
Reporting Checklist: The authors have completed the COREQ and CONSORT reporting checklists. Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-31/rc
Trial Protocol: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-31/tp
Data Sharing Statement: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-31/dss
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-31/prf
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-31/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The qualitative study was approved by the Institutional Review Board of Texas Woman’s University (No. 00000829), the RCT was approved by the Institutional Review Board of the University of North Texas Health Science Center (No. 00000702), and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kelly AS, Barlow SE, Rao G, et al. Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 2013;128:1689-712. [Crossref] [PubMed]
- Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1876-85. [Crossref] [PubMed]
- Park MH, Falconer C, Viner RM, et al. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev 2012;13:985-1000. [Crossref] [PubMed]
- Ma J, Flanders WD, Ward EM, et al. Body mass index in young adulthood and premature death: analyses of the US National Health Interview Survey linked mortality files. Am J Epidemiol 2011;174:934-44. [Crossref] [PubMed]
- Skinner AC, Ravanbakht SN, Skelton JA, et al. Prevalence of Obesity and Severe Obesity in US Children, 1999-2016. Pediatrics 2018;141:e20173459. Erratum in: Pediatrics 2018 Sep;142(3):e20181916. [Crossref] [PubMed]
- Ogden CL, Carroll MD, Fakhouri TH, et al. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household - United States 2011-2014. MMWR Morb Mortal Wkly Rep 2018;67:186-9. [Crossref] [PubMed]
- Stettler N, Kumanyika SK, Katz SH, et al. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr. 2003;77:1374-8. [Crossref] [PubMed]
- Druet C, Stettler N, Sharp S, et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr Perinat Epidemiol 2012;26:19-26. [Crossref] [PubMed]
- Taveras EM, Rifas-Shiman SL, Sherry B, et al. Crossing growth percentiles in infancy and risk of obesity in childhood. Arch Pediatr Adolesc Med 2011;165:993-8. [Crossref] [PubMed]
- Harrington JW, Nguyen VQ, Paulson JF, et al. Identifying the "tipping point" age for overweight pediatric patients. Clin Pediatr (Phila) 2010;49:638-43. [Crossref] [PubMed]
- Blake-Lamb TL, Locks LM, Perkins ME, et al. Interventions for Childhood Obesity in the First 1,000 Days A Systematic Review. Am J Prev Med 2016;50:780-9. [Crossref] [PubMed]
- Redsell SA, Edmonds B, Swift JA, et al. Systematic review of randomised controlled trials of interventions that aim to reduce the risk, either directly or indirectly, of overweight and obesity in infancy and early childhood. Matern Child Nutr 2016;12:24-38. [Crossref] [PubMed]
- Ciampa PJ, Kumar D, Barkin SL, et al. Interventions aimed at decreasing obesity in children younger than 2 years: a systematic review. Arch Pediatr Adolesc Med 2010;164:1098-104. Erratum in: Arch Pediatr Adolesc Med 2011 Feb;165(2):111. [Crossref] [PubMed]
- Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011;CD001871. [PubMed]
- Taveras EM, Blackburn K, Gillman MW, et al. First steps for mommy and me: a pilot intervention to improve nutrition and physical activity behaviors of postpartum mothers and their infants. Matern Child Health J 2011;15:1217-27. [Crossref] [PubMed]
- Morandi A, Tommasi M, Soffiati F, et al. Prevention of obesity in toddlers (PROBIT): a randomised clinical trial of responsive feeding promotion from birth to 24 months. Int J Obes (Lond) 2019;43:1961-6. [Crossref] [PubMed]
- Taylor BJ, Gray AR, Galland BC, et al. Targeting Sleep, Food, and Activity in Infants for Obesity Prevention: An RCT. Pediatrics 2017;139:e20162037. [Crossref] [PubMed]
- Schroeder N, Rushovich B, Bartlett E, et al. Early Obesity Prevention: A Randomized Trial of a Practice-Based Intervention in 0-24-Month Infants. J Obes 2015;2015:795859. [Crossref] [PubMed]
- Machuca H, Arevalo S, Hackley B, et al. Well Baby Group Care: Evaluation of a Promising Intervention for Primary Obesity Prevention in Toddlers. Child Obes 2016;12:171-8. [Crossref] [PubMed]
- Paul IM, Savage JS, Anzman SL, et al. Preventing obesity during infancy: a pilot study. Obesity (Silver Spring) 2011;19:353-61. [Crossref] [PubMed]
- Savage JS, Birch LL, Marini M, et al. Effect of the INSIGHT Responsive Parenting Intervention on Rapid Infant Weight Gain and Overweight Status at Age 1 Year: A Randomized Clinical Trial. JAMA Pediatr 2016;170:742-9. [Crossref] [PubMed]
- Campbell KJ, Lioret S, McNaughton SA, et al. A parent-focused intervention to reduce infant obesity risk behaviors: a randomized trial. Pediatrics 2013;131:652-60. [Crossref] [PubMed]
- French GM, Nicholson L, Skybo T, et al. An evaluation of mother-centered anticipatory guidance to reduce obesogenic infant feeding behaviors. Pediatrics 2012;130:e507-17. [Crossref] [PubMed]
- Verbestel V, De Coen V, Van Winckel M, et al. Prevention of overweight in children younger than 2 years old: a pilot cluster-randomized controlled trial. Public Health Nutr 2014;17:1384-92. [Crossref] [PubMed]
- Daniels LA, Mallan KM, Nicholson JM, et al. Outcomes of an early feeding practices intervention to prevent childhood obesity. Pediatrics 2013;132:e109-18. [Crossref] [PubMed]
- Heinig MJ, Ishii KD, Bañuelos JL, et al. Sources and acceptance of infant-feeding advice among low-income women. J Hum Lact 2009;25:163-72. [Crossref] [PubMed]
- Bentley ME, Dee DL, Jensen JL. Breastfeeding among Low-Income, African-American Women: Power, Beliefs, and Decision Making. J Nutr 2003;133:305S-309S. [Crossref] [PubMed]
- Baughcum AE, Burklow KA, Deeks CM, et al. Maternal feeding practices and childhood obesity: a focus group study of low-income mothers. Arch Pediatr Adolesc Med 1998;152:1010-4. [Crossref] [PubMed]
- Peacock-Chambers E, Dicks K, Sarathy L, et al. Perceived Maternal Behavioral Control, Infant Behavior, and Milk Supply: A Qualitative Study. J Dev Behav Pediatr 2017;38:401-8. [Crossref] [PubMed]
- Matvienko-Sikar K, Kelly C, Sinnott C, et al. Parental experiences and perceptions of infant complementary feeding: a qualitative evidence synthesis. Obes Rev 2018;19:501-17. [Crossref] [PubMed]
- Appleton J, Laws R, Russell CG, et al. Infant formula feeding practices and the role of advice and support: an exploratory qualitative study. BMC Pediatr 2018;18:12. [Crossref] [PubMed]
- Russell CG, Taki S, Azadi L, et al. A qualitative study of the infant feeding beliefs and behaviours of mothers with low educational attainment. BMC Pediatr 2016;16:69. [Crossref] [PubMed]
- Redsell SA, Atkinson P, Nathan D, et al. Parents' beliefs about appropriate infant size, growth and feeding behaviour: implications for the prevention of childhood obesity. BMC Public Health 2010;10:711. [Crossref] [PubMed]
- Bentley F, Swift JA, Cook R, et al. "I would rather be told than not know" - A qualitative study exploring parental views on identifying the future risk of childhood overweight and obesity during infancy. BMC Public Health 2017;17:684. [Crossref] [PubMed]
- Xiong R, Spaccarotella K, Quick V, et al. Generational Differences: A Comparison of Weight-Related Cognitions and Behaviors of Generation X and Millennial Mothers of Preschool Children. Int J Environ Res Public Health 2019;16:2431. [Crossref] [PubMed]
- Evans WD, Wallace JL, Snider J. Pilot evaluation of the text4baby mobile health program. BMC Public Health 2012;12:1031. [Crossref] [PubMed]
- Denney-Wilson E, Laws R, Russell CG, et al. Preventing obesity in infants: the Growing healthy feasibility trial protocol. BMJ Open 2015;5:e009258. [Crossref] [PubMed]
- Uesugi KH, Dattilo AM, Black MM, et al. Design of a Digital-Based, Multicomponent Nutrition Guidance System for Prevention of Early Childhood Obesity. J Obes 2016;2016:5067421. [Crossref] [PubMed]
- Gibby CLK, Palacios C, Campos M, et al. Acceptability of a text message-based intervention for obesity prevention in infants from Hawai'i and Puerto Rico WIC. BMC Pregnancy Childbirth 2019;19:291. [Crossref] [PubMed]
- Gallegos D, Russell-Bennett R, Previte J, et al. Can a text message a week improve breastfeeding? BMC Pregnancy Childbirth 2014;14:374. [Crossref] [PubMed]
- Brown C, Davis KE, Habiba N, et al. Parent preferences for text messages containing infant feeding advice. Mhealth 2020;6:9. [Crossref] [PubMed]
- Wansink B, Pope L. When do gain-framed health messages work better than fear appeals? Nutr Rev 2015;73:4-11. [Crossref] [PubMed]
- Skinner CS, Tiro J, Champion VL. The Health Belief Model. In: Glanz K, Rimer BK, Viswanath K. editors. Health Behavior and Health Education. San Francisco, CA: Jossey-Bass; 2015:75-94.
- National Center for Health Statistics. NHANES 2013-2014 Questionnaire Data Overview. Centers for Disease Control and Prevention. 2013. Available online: https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/questionnaires/dbq_h.pdf
- Akhtar-Danesh N, Dehghan M, Morrison KM, et al. Parents' perceptions and attitudes on childhood obesity: a Q-methodology study. J Am Acad Nurse Pract 2011;23:67-75. [Crossref] [PubMed]
- Division of Nutrition PA, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Breastfeeding Among US Children Born 2010-2017, CDC National Immunization Study 2020 [Available from: https://www.cdc.gov/breastfeeding/data/nis_data/results.html.
- Davis KE, Li X, Adams-Huet B, et al. Infant feeding practices and dietary consumption of US infants and toddlers: National Health and Nutrition Examination Survey (NHANES) 2003-2012. Public Health Nutr 2018;21:711-20. [Crossref] [PubMed]
- Gross RS, Mendelsohn AL, Fierman AH, et al. Maternal infant feeding behaviors and disparities in early child obesity. Child Obes 2014;10:145-52. [Crossref] [PubMed]
- Gross RS, Mendelsohn AL, Gross RS, Scheinmann R, Messito MJ. Randomized Controlled Trial of Primary Care-Based Child Obesity Prevention Intervention on Infant Feeding Practices. J Pediatr 2016;174:171-7.e2. [Crossref] [PubMed]
- Free C, Phillips G, Watson L, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med 2013;10:e1001363. [Crossref] [PubMed]
- Hall AK, Cole-Lewis H, Bernhardt JM. Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health 2015;36:393-415. [Crossref] [PubMed]
Cite this article as: Davis KE, Klingenberg A, Massey-Stokes M, Habiba N, Gautam R, Warren C, Yeatts P. The Baby Bites Text Messaging Project with randomized controlled trial: texting to improve infant feeding practices. mHealth 2023;9:11.