
Management of arterial hypertension: home blood pressure measurement is a cornerstone for telemonitoring and self-management
Introduction
Home blood pressure monitoring (HBPM) is becoming the cornerstone of the management of arterial hypertension using telemedicine or mobile health because it combines the advantages of its intrinsic qualities to that of the new information and communications technologies (NICTs). HBPM has been shown to detect white coat hypertension and masked hypertension, is the preferred method for patients, and there are many reliable, inexpensive, and easy-to-use measuring devices available. An example of a disadvantage is that some patients make mistakes during their home measurements (primarily due to lack of patient training by healthcare providers), in practice, HBPM is widely recommended by all the scientific societies (1-4).
The first self-measurement of blood pressure (SBPM) devices with remote transmission capability date back to the 1990s. They connected directly to the wired telephone sockets in the patients’ homes and the results were transmitted to the physician’s personal computer. A quarter of a century ago, the pioneers of teletransmission understood that this process “provides evidence that the casual blood pressure (BP) measurements at the office should not remain the gold standard for making decisions on hypertension management” (5). Since then, the development of mobile telephones has made it possible to design BP monitors with data transmission via cellular lines, contributing to the emergence of the concepts of: “e-health” or “digital health” (the use of electronic processes, information and communication technologies to provide healthcare services); “telehealth” (the teletransmission of health-related data from one site to another via electronic communications); “m-health” or “mobile health” (teletransmission of health-related data by means of mobile communication devices (i.e., smartphones). Today, the direct-to-consumer marketing of many devices but also management programs of hypertension create a new context allowing an algorithmic processing of information for remote decision-making either by the patient or by a healthcare professional; this is “digital intervention” (6).
The use of NICTs has different organizational implications depending on the context. A distinction must be made between transmissions of BP values initiated by healthcare professionals, patients, or healthcare consumers. One should not confuse one-off analyses in a medical emergency (in this context BP is a “vital sign”) and long-term monitoring of BP as a chronic cardiovascular risk factor. In the first case, the clinician’s analysis is based on a single measurement, (for example a BP measurement to assess the severity of a hemorrhage); in the second, the medical reasoning must take into account the evolution of many BP readings, either over 24 hours [ambulatory BP monitoring (ABPM)] or over several days (HBPM). For the long-term follow-up, new technologies have the advantage of keeping a precise history of data with the possibility of algorithmic processing to show its evolution over time. The present review is focused on the long-term monitoring of hypertensive patients. It describes the care pathway in distinguishing the medical situations of self-management and telemonitoring, the differences of which imply a different use of NICTs.
Material and technique
Devices for measuring BP
The SBPM devices currently recommended are the automated upper-arm BP monitors. According to guidelines, the patient must be sitting with their back supported, at rest for at least 5 minutes before performing BP measurements using an appropriate cuff size, and stay quiet during measurement. Several measurements must be performed within a given period of time to accurately represent the patient’s average BP (1-4).
In most cases the patient carries out the act of HBPM device purchase (buy in pharmacies, department stores or on the internet) by himself. Consequently, the healthcare professional must guide the patient’s choice towards validated BP monitors, software included if connected devices. Conversely, he must call attention to the availability of many non-validated and/or non-reliable devices. There are many types of BP measuring devices, some with a cuff (wrist or arm), others called wearables, or even smartphone applications (Table 1) (7,8).
Table 1
| Automated oscillometric upper arm cuff or wrist cuff devices, unconnected or connected (wireless, or wired) |
| Wireless smartphone applications (paired with an external oscillometric wireless BP monitor or turning the smartphone into a cuffless BPM device (fingerprint, wrist, face) |
| Wearable monitors for long-term surveillance (e.g., wrist tonometers or finger plethysmography) or continual monitors (wrist, chest, ear) |
BP, blood pressure; BPM, blood pressure monitoring.
Provide such information is difficult because of the explosion of new devices attracting consumers by their design or ease of use. More than 500 wearable wristband devices are available on the online Australian Market (9).
Many devices are not suitable for medical decision-making, although some claim to be validated for example this is the case of cuffless monitors for which there is not yet an international standard to cover their validation (8).
Data communication technologies
The transmission of BP data can be done using various techniques. Some are adapted to the use of conventional BP monitors, which still remains predominant today: This is the case of websites with dedicated forms allowing manual data input of BP readings. Others use dedicated wireless devices based on Bluetooth and/or Wi-Fi, with mobile phone-based transmission systems. More than ten modalities exist, details have been described elsewhere (10).
A distinction must be made between the tools used by professionals who must comply with strict regulatory obligations (security and data confidentiality) and those of healthcare consumers who are free of these rules (for example, nothing prohibits a patient from publishing their medical data on unsecured social networks that do not comply with the regulations [for example the European General Data Protection Regulation (GDPR)].
Home BP telemonitoring (HBPT)
The HBPT is the remote transmission of BP values, measured at home and transmitted to the clinician’s office or hospital, by means of telehealth strategies. Once the data are received at the central telemedicine server, they are stored, analyzed and then reviewed by a healthcare professionals.
In this context, the main principles of the patient-clinician consultation relationship (usual care) are maintained: the clinician decides when to initiate and stop the procedure (start and end of telemonitoring, synchronous or asynchronous contact), its technical methods (choice of transmission tools and the type of data transmitted) and remains the author of medical decisions. In practice, the healthcare professional masters the technical environment (secured in accordance with the regulations) and can involve other professionals (nurses, telemedicine assistants, pharmacists). If the system manages alert rules, it can set the thresholds and the frequency of information feedback (immediate or periodic automatic forward). Throughout this process the healthcare professional can communicate with the patient to gather information on his/her health status and adjust treatment (if needed) according to the indications of the managing physician.
BP performance of BP telemonitoring
Randomized controlled trials (RCTs) studies have demonstrated HBPT ability in improving patients’ compliance and adherence to antihypertensive treatment and in accomplishing better hypertension control rates. The increase in BP control rates obtained, resulted in a significantly larger prescription of antihypertensive medications, but a similar rate of office consultations (10,11).
A meta-analysis of RCTs including a total of 23 studies (n=7,037 patients) showed regular implementation of HBPT during a 6-month follow-up period, was associated with significantly greater reductions in BP [average and 95% confidence interval (CI): 4.7 (6.2, 3.2) mmHg for systolic BP (SBP) and 2.5 (3.3, 1.6) mmHg for diastolic BP (DBP); P<0.001 for both] (11).
In the HOME BP study after 1 year, mean values of BP decreased from 151.7/86.4 to 138.4/80.2 mmHg in the intervention group and from 151.6/85.3 to 141.8/79.8 mmHg in the usual care group, giving a mean difference in SBP of −3.4 mmHg (95% CI: −6.1 to −0.8 mmHg) and of −0.5 mmHg (−1.9 to 0.9 mmHg) in DBP (12). The SBP reduction is clinically interesting.
The HBPM should not be overvalued: In reality, the level of evidence (strength of evidence) for the reduction in BP is “moderate”. It is “very low” for improving adherence to antihypertensive treatment, drug safety or reducing deaths or hospitalizations (13). Its financial impact is still debated and its cost evaluations are contradictory (8). Some studies show that healthcare costs were significantly (P<0.0001) larger in the telemonitoring group (11). Its ability to reduce the frequency of office consultations is poorly documented in real life because it is difficult to transpose the practices of clinical trials to current practice (routine primary care; poor integration with routine clinical process). Finally, the problems of interfacing with other care software are remaining.
Furthermore, HBPT cannot be performed by all hypertensive patients who constitute one third of the adult population. Telemonitoring implies that patients accept this mode of care, have access to the Internet and computer equipment, know how to fill out questionnaires, input the BP values into the system, are able to follow remote instructions (received by phone, email, SMS or given during a teleconsultation) and agree to adaption of treatment without facing a doctor in person. Let’s take an example: out of 11,400 patients contacted to take part in the HOME BP study, those who gave the reasons for their refusal were the lack of internet access (41%) and the wish not to change treatment (21%) (12).
Today the place of HBPT is not clearly established in current practice. We will see below some specific situations where it is reasonable to offer telemonitoring at first to high-risk patients who need rapid adaptation of treatments, such as malignant hypertension, resistant hypertension, pregnancy-induced hypertension, drugs-induced hypertension, etc.
Self-management and mHealth
Patients using NICTs of their own initiatives have greater leeway than professionals because they own their health data and are not subject to professional confidentiality). After having measured their BP (compliant or not) the patients are free to make their own decisions (for the better or for the worse). For example, buying products or medicines (good or bad), subscribing to an e-health platform, turning to a third party (friend, family, carer, charlatan or qualified health professional) remotely or face-to-face. To make a self-diagnosis of hypertension they can use an application (reliable or not).
To avoid bad practices, the clinician must supervise the self-management approach. In practice, he must: (I) ensure the quality of the applications used; (II) inform and educate the patient; (III) choose the appropriate time between two medical consultations considering the level of cardiovascular risk and the wishes and autonomy of the patient.
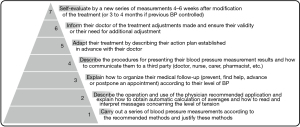
Digital interventions (apps, programs, or software used in healthcare) have the potential to support people in self-management (2). We define here by self-management, a strategy to support patients to self-diagnose hypertension or to self-control their BP after performing a SBPM at home. This patient activation needs to assess a patient’s acceptance and ability to engage with self-management. This approach presupposes the prior acquisition of skills, the level of which must be adapted to the level of health literacy of each patient. It is not one size fits all. For patient education by health care providers, we propose a skill pyramid which includes 7 levels (Figure 1) (14). Level 1 at the base of the pyramid corresponds to the simplest task, level 7 to that reserved only for autonomous patients who have acquired the previous stages. It is only with them that self-medication adjustment can be offered. To reach the next level, the patient must fully understand the precedent step.
App quality
App quality is an important concern. Too many are designed by engineers without any collaboration with the healthcare professionals (15,16).
Some algorithms confuse the thresholds of office BP and home BP, others base their analysis on specific measurements (not on an average of several measurements) and most do not take into account the medical profile of the user, finally few are subject to published reviews and keep their algorithm secret (17). Few of m-apps for hypertension can be regarded as accurate and safe for clinical use and to date, we do not have high quality evidence to determine the overall effect of smartphone apps on BP control (7).
A compilation of RCTs related to the influence of an app-based intervention in hypertensives shows that smartphone interventions lead to a reduction in BP and an increase in medication adherence (18).
According to this analysis of 6 studies assessing SBP, a significant overall effect showed in favor of the smartphone intervention (weighted mean difference: −2.28, 95% CI: −3.90 to −0.66). Conversely, the “smart hypertension control study” found no significant difference with a stand-alone app (19). Other studies have not clearly shown that the apps made it possible to obtain better control of the BP of hypertensive subjects (20-23).
Specific clinical situations
The relevance and methods of use of NICTs differ according to the patients. The target BP to be achieved under treatment depends on the medical profile (age, comorbidities) and the speed of therapeutic adaptations are not the same for all patients: the monitoring frequencies of a person with grade 1 hypertension without comorbidity, of a woman at the end of pregnancy with a history of preeclampsia, a patient with a malignant hypertension attack or heart failure, a patient on dialysis, or people treated with molecules with a hypertensive effect [corticosteroids, estrogen, tyrosine kinase inhibitor (TKI), etc.] are different (24).
The use of telemonitoring and app coaching for pregnant women is booming for clinical reasons (relevance of BP monitoring during pregnancy with the search for an alternative to hospitalization) and social reasons (patients motivated to self-monitor and many know how to use a smartphone because of their young age) (25-29).
A survey of women using a smartphone pregnancy calendar found that almost a third of the majority of women monitored their BP at home on their own initiative, but did not seek any medical advice (30). It is therefore necessary to direct them towards validated apps, such as the free Hy-Result application in current practice (31,32).
Among specific situations, we can mention the case of patients for whom the traditional follow-up consultation is not necessarily the most suitable choice for medico-social reasons (physical disability making travel complex, remoteness from place of care, immunosuppression or fragility justifying limiting contacts at risk of infection).
Outlook
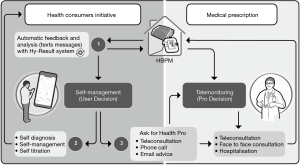
Currently, a hypertensive patient may be referred to a consultation (specialized center and/or primary care), as an outpatient or in hospitalization. Similarly, the use of NICT presupposes a choice of monitoring mode (HBPT or self-management, for example). In the example of the Hy-Result app, a self-management program can be a gatekeeper for multiple means of contacting a professional after an algorithmic sorting (Figure 2) (33).
The design of digital interventions is currently evolving and it is too early to propose a standardization of practices. Knowledge and assessments are lacking and several categories of professionals can contribute:
- Manufacturers should design affordable, simple, and user-friendly devices (providing reliable and meaningful data), possibly integrated in mobile phones, tablets or home appliances. Cuffless devices for 24/7 longitudinal BP measurement are among the new possibilities but not recommended up today;
- Researchers must assess the role of artificial intelligence. Exploiting such data may disrupt understanding of cardiovascular disease classification, and contributing actionable analytics to improve health and healthcare, but major challenges need to be addressed to realize more fully their potential (34);
- Health authorities must assure adequate infrastructures (mobile network, Internet, connected homes); take into consideration people who are digitally excluded; find new financial models of care and focus on legal and ethical frameworks for data sharing, confidentiality and promote cost-effective systems;
- Scientific societies must publish new standardized validation procedures, specifically in the reliable tracking of BP changes in the short and long-term. As for the connected devices, it would be preferable to validate both the BP monitor and the software linked to it;
- Proper implementation of BP monitoring guidelines by doctors;
- Clinicians show robust evidence with blinded, prospective randomized clinical trials addressing the role of m-health strategies for BP, focusing on hard outcomes over longer follow up times. Carry out real-life studies with healthcare consumers to assess the impact of the “self-management tool”; evaluate the ability of patients to correctly report data (patient-reported outcomes) even in the context of poor health and/or poor informatics illiteracy; demonstrate the indications and benefits of monitoring other parameters than BP alone [single channel electrocardiogram (ECG), pulse oximetry, body temperature, blood glucose, medication intake, etc.];
- Patient associations can oversee the ethics of new digital interventions.
Conclusions
NICTs are a real opportunity to improve the management of hypertension (Table 2). It is probable, but it is difficult to estimate the time needed for this hope to become an accessible reality for most patients. Beyond the scientific evidence that remains to be provided, it is up to society to resolve the resistance to change on the part of professionals as well as that of patients. It can be evolution taking the time of one or more generations. For example, will doctors who have a traditional activity of face-to-face consultation agree to process data from hundreds of patients simultaneously? How much confidence will patients have in the algorithms?
Table 2
| HBPM is widely recommended by all the scientific societies |
| The use of NICTs has different organizational implications depending on the medical context |
| Too many app are designed by engineers without any collaboration with the healthcare professionals |
| Many direct-to-consumer BP connected device are not suitable for medical decision-making |
| With the HBPT the physicians decides when to initiate and stop the procedure and remains the author of medical decisions |
| Digital interventions (apps, programs, or software used in healthcare) have the potential to support people in self-management |
| Self-management presupposes the prior acquisition of skills, the level of which must be adapted to the level of health literacy of each patient |
HBPM, home blood pressure monitoring; NICTs, new information and communications technologies; BP, blood pressure; HBPT, home blood pressure telemonitoring.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-51/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-22-51/coif). NPV serves as an unpaid editorial board member of mHealth from December 2022 to November 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021-104. [Crossref] [PubMed]
- Parati G, Stergiou GS, Bilo G, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the Working Group on Blood Pressure Monitoring and Cardiovascular Variability of the European Society of Hypertension. J Hypertens 2021;39:1742-67. [Crossref] [PubMed]
- Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension 2020;75:1334-57. [Crossref] [PubMed]
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension 2018;71:1269-324. [Crossref] [PubMed]
- Menard J, Linhart A, Weber JL, et al. Teletransmission and computer analysis of self-blood pressure measurements at home. Blood Pressure Monitoring 1996;1:S63-8.
- Postel-Vinay N, Bobrie G, Savard S, et al. Home blood pressure measurement and digital health: communication technologies create a new context. J Hypertens 2018;36:2125-31. [Crossref] [PubMed]
- Stergiou GS, Parati G, Mancia G. Home blood pressure monitoring. Updates in hypertension and cardiovascular protection. Cham: Springer International Publishing, 2020.
- Stergiou GS, Mukkamala R, Avolio A, et al. Cuffless blood pressure measuring devices: review and statement by the European Society of Hypertension Working Group on Blood Pressure Monitoring and Cardiovascular Variability. J Hypertens 2022;40:1449-60. [Crossref] [PubMed]
- Burnier M, Kjeldsen SE, Narkiewicz K, et al. Cuff-less measurements of blood pressure: are we ready for a change? Blood Press 2021;30:205-7. [Crossref] [PubMed]
- Parati G, Dolan E, McManus RJ, et al. Home blood pressure telemonitoring in the 21st century. J Clin Hypertens (Greenwich) 2018;20:1128-32. [Crossref] [PubMed]
- Omboni S, Gazzola T, Carabelli G, et al. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens 2013;31:455-67; discussion 467-8. [Crossref] [PubMed]
- McManus RJ, Little P, Stuart B, et al. Home and Online Management and Evaluation of Blood Pressure (HOME BP) using a digital intervention in poorly controlled hypertension: randomised controlled trial. BMJ 2021;372:m4858. [Crossref] [PubMed]
- Omboni S, McManus RJ, Bosworth HB, et al. Evidence and Recommendations on the Use of Telemedicine for the Management of Arterial Hypertension: An International Expert Position Paper. Hypertension 2020;76:1368-83. [Crossref] [PubMed]
- Postel-Vinay N, Bobrie G, Baud D, et al. Autosurveillance de la pression artérielle: osons confier aux patients les clés de leur suivi. Rev Med Suisse 2021;17:1233-6. [Crossref] [PubMed]
- Kumar N, Khunger M, Gupta A, et al. A content analysis of smartphone-based applications for hypertension management. J Am Soc Hypertens 2015;9:130-6. [Crossref] [PubMed]
- Plante TB, Urrea B, MacFarlane ZT, et al. Validation of the Instant Blood Pressure Smartphone App. JAMA Intern Med 2016;176:700-2. [Crossref] [PubMed]
- Ranasinghe M, Cabrera A, Postel-Vinay N, et al. Transparency and Quality of Health Apps: The HON Approach. Stud Health Technol Inform 2018;247:656-60. [PubMed]
- Xu H, Long H. The Effect of Smartphone App-Based Interventions for Patients With Hypertension: Systematic Review and Meta-Analysis. JMIR Mhealth Uhealth 2020;8:e21759. [Crossref] [PubMed]
- Persell SD, Peprah YA, Lipiszko D, et al. Effect of Home Blood Pressure Monitoring via a Smartphone Hypertension Coaching Application or Tracking Application on Adults With Uncontrolled Hypertension: A Randomized Clinical Trial. JAMA Netw Open 2020;3:e200255. [Crossref] [PubMed]
- Kim JY, Wineinger NE, Steinhubl SR. The Influence of Wireless Self-Monitoring Program on the Relationship Between Patient Activation and Health Behaviors, Medication Adherence, and Blood Pressure Levels in Hypertensive Patients: A Substudy of a Randomized Controlled Trial. J Med Internet Res 2016;18:e116. [Crossref] [PubMed]
- Buis L, Hirzel L, Dawood RM, et al. Text Messaging to Improve Hypertension Medication Adherence in African Americans From Primary Care and Emergency Department Settings: Results From Two Randomized Feasibility Studies. JMIR Mhealth Uhealth 2017;5:e9. [Crossref] [PubMed]
- Morawski K, Ghazinouri R, Krumme A, et al. Association of a Smartphone Application With Medication Adherence and Blood Pressure Control: The MedISAFE-BP Randomized Clinical Trial. JAMA Intern Med 2018;178:802-9. [Crossref] [PubMed]
- Searcy RP, Summapund J, Estrin D, et al. Mobile health technologies for older adults with cardiovascular disease: current evidence and future directions. Current Geriatrics Reports 2019;8:31-42. [Crossref]
- Azizi M, Chedid A, Oudard S. Home blood-pressure monitoring in patients receiving sunitinib. N Engl J Med 2008;358:95-7. [Crossref] [PubMed]
- Hughson JP, Daly JO, Woodward-Kron R, et al. The Rise of Pregnancy Apps and the Implications for Culturally and Linguistically Diverse Women: Narrative Review. JMIR Mhealth Uhealth 2018;6:e189. [Crossref] [PubMed]
- Perry H, Sheehan E, Thilaganathan B, et al. Home blood-pressure monitoring in a hypertensive pregnant population. Ultrasound Obstet Gynecol 2018;51:524-30. [Crossref] [PubMed]
- Pealing LM, Tucker KL, Mackillop LH, et al. A randomised controlled trial of blood pressure self-monitoring in the management of hypertensive pregnancy. OPTIMUM-BP: A feasibility trial. Pregnancy Hypertens 2019;18:141-9. [Crossref] [PubMed]
- van den Heuvel JFM, Lely AT, Huisman JJ, et al. SAFE@HOME: Digital health platform facilitating a new care path for women at increased risk of preeclampsia - A case-control study. Pregnancy Hypertens 2020;22:30-6. [Crossref] [PubMed]
- van den Heuvel JFM, Ayubi S, Franx A, et al. Home-Based Monitoring and Telemonitoring of Complicated Pregnancies: Nationwide Cross-Sectional Survey of Current Practice in the Netherlands. JMIR Mhealth Uhealth 2020;8:e18966. [Crossref] [PubMed]
- Postel-Vinay N, Jouhaud P, Bobrie G, et al. Home blood pressure measurement and mobile health app for pregnant and postpartum women. Journal of Hypertension 2019;37:e280. [Crossref]
- Postel-Vinay N, Bobrie G, Ruelland A, et al. Automated interpretation of home blood pressure assessment (Hy-Result software) versus physician's assessment: a validation study. Blood Press Monit 2016;21:111-7. [Crossref] [PubMed]
- Postel-Vinay N, Shao JD, Pinton A, et al. Home Blood Pressure Measurement and Self-Interpretation of Blood Pressure Readings During Pregnancy: Hy-Result e-Health Prospective Study. Vasc Health Risk Manag 2022;18:277-87. [Crossref] [PubMed]
- Postel-Vinay N, Steichen O, Pébelier E, et al. Home blood pressure monitoring and e-Health: investigation of patients' experience with the Hy-Result system. Blood Press Monit 2020;25:155-61. [Crossref] [PubMed]
- Hemingway H, Asselbergs FW, Danesh J, et al. Big data from electronic health records for early and late translational cardiovascular research: challenges and potential. Eur Heart J 2018;39:1481-95. [Crossref] [PubMed]
Cite this article as: Postel-Vinay N, Bobrie G, Asmar R, Stephan D, Amar L. Management of arterial hypertension: home blood pressure measurement is a cornerstone for telemonitoring and self-management. mHealth 2023;9:18.


