Information and communication technology use by female residents of public housing
Introduction
Using new and emerging technologies to provide intervention and support for behavior change is a novel and still under-utilized opportunity, particularly among populations that face health disparities [e.g., low socio-economic status (SES) populations] (1,2). Called Information and Communication Technologies (ICT), which encompasses cell phones, computer kiosks, and other electronic devices with access to services such as text messaging, Internet, and social media (3), these technologies carry information in bidirectional formats between experts and participants to provide specific cues, strategies, and multiple types of support to improve health-related actions and choices. As described by Viswanath and colleagues, ICTs “…offer an unprecedented opportunity to provide information on cancer prevention, monitor lifestyles and health behaviors, promote participatory decision making during cancer detection, diagnosis, and treatment, and foster quality of life during survivorship or end of life” (4). As such, ICTs are being applied to and evaluated in multiple areas along the cancer prevention and control continuum (5-8). For example, in the area of weight management, a systematic review of technology-based interventions, using modalities such as web, personal digital assistants, text messaging, email, and connected devices, found that approximately half of the included interventions had beneficial effects on weight (9).
However, the use of ICT is not evenly and equally distributed in the population. The term digital divide has been used to describe differential access to web-based technologies among difference groups, such as SES levels (10). American adults who are older, non-English speaking, less educated, and with lower incomes are less likely to access the Internet (11). However, Pew studies suggest these kinds of communication systems are increasingly common among all demographics of users, especially when including the rise of mobile devices (3,12). Mobile devices can be used for phone, text, and Internet use. African Americans and English-speaking Latinos are just as likely as whites to own any mobile phone and to use it for a wider range of activities (11,13-15). As ICT use evolves, there may be opportunities to better use these technologies for cancer control and prevention among populations with health disparities.
Public housing residents in Boston are at increased risk of having health risk conditions and behaviors including higher levels of obesity, physical inactivity, and smoking compared to other city residents (16). This is important due to the well-established links between nutrition, obesity, physical activity, and smoking and cancer prevention and control. Focusing on nutrition, obesity, and physical activity, a comprehensive report reviewing the scientific literature was published in 2007 documenting the strength of evidence of these links and multiple cancer sites (for example, endometrium, colorectum, postmenopausal breast cancers) (17) and since that time has been updating their findings with new research (http://www.aicr.org/continuous-update-project/). Despite close proximity to community health centers and academic medical centers, previous work has shown that public housing residents face barriers to engaging in care (18). Our extensive pilot data also indicates that public housing residents are open and interested in improving their health and in participating in evaluation activities for behavior change opportunities (18-22). The use of ICT to support public housing residents may be a feasible and effective way to reach a large number of public housing residents with appropriate messaging and support about modifiable cancer preventive behaviors.
We have no data, however, on the best ICT methods to select for reaching public housing residents with health supporting information about modifiable behaviors related to cancer prevention and control. Most surveys of ICT use do not identify public housing residents separately. Nor do surveys specifically focus on public housing residents as a low-SES vulnerable population. In this study, we examine the frequency of ICT use among a subgroup of low-SES individuals, adult female public housing residents, and also examine if ICT use varies across demographic, health, or obesity-specific variables.
Methods
Study design
We conducted a cross-sectional study of baseline data from an obesity prevention study in Boston Public Housing for female residents, called Healthy Families (n=211). The methods of the parent study have been previously described (21). In brief, participants were eligible if they were women aged 18–72 who lived in public housing and were responsible for a girl between the ages of 8 and 15, English or Spanish speaking, and able to change diet and activity behaviors if desired. A woman was excluded if she was not interested in participating or not able to complete survey tools. After collection of baseline data had begun, we decided to add additional questions regarding ICT use to the baseline survey which were included as part of the survey from that point forward. Thus, a subset of the total sample (n=158) responded to the questions about ICT use. This study was approved by the Boston University Medical Campus Institutional Review Board.
Measures
We collected information on socio-demographics, general health, and obesity. Socio-demographic variables including age, race/ethnicity, primary language spoken at home, country of birth, and educational attainment, as well as health and obesity-related characteristics were measured. For health variables, we examined self-rated general health, dichotomized as excellent, very good, or good versus fair or poor (23), and report of at least one health problem. Regarding obesity-related measures, height and weight were measured for each participant to calculate body mass index (BMI). Obesity was defined as BMI greater than or equal to 30. Participants were surveyed about physical activity with the question, “During the last 7 days, on how many days did you walk at least 10 min at a time in your neighborhood?”. Participants responded with number of days per week and minutes per day, from which standard levels of physical activity (“inactive”, “minimally or sufficiently active”, and “more or highly active”) were extrapolated (24).
We collected information on ICT use with questions from the Pew Internet and American Life Project and previous studies of Boston public housing residents (25,26). Questions are listed in Table 1. We adapted the Pew typology of ICT users to define an ICT “user” in our study based on two of the three dimensions of ICT use: assets (access to hardware and connectivity) and activity (frequency of use) (25). We did not collect data on the third dimension, attitudes towards use. We defined an email, Internet, or social media “user” as a participant who engaged in daily use or use within the last day. A health information Internet user was an Internet user who answered affirmatively to the question on online health, dieting, or fitness-seeking. A multimodal user was a participant who used all three media—Internet, email, and social media—in the last day.
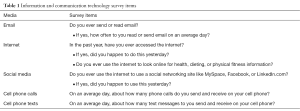
Full table
Analysis
SAS 9.3 was used to perform all analyses. We report descriptive statistics and performed bivariate comparisons of socio-demographic, health, and obesity-related characteristics by user status for email, Internet, and social media, as well as health information Internet user and multimodal user. Student t-tests were performed for continuous measures, Chi square tests for categorical variables, and Fisher’s exact tests when cell size was <5.
Results
The socio-demographic and health characteristics of our subset sample (n=158) include: the majority were Hispanic or Latino (64%), Spanish-speaking (49%), non-United States born (71%), and had a high school education or less (64%). Nearly 50% were obese, a third overweight, and over 80% sedentary. Mean age was 38 (SD=7). Two-thirds of participants rated their health as excellent, very good, or good, while 53% reported at least one health problem. However, compared to the entire baseline cohort, our sample had a greater percentage of Hispanic (69% vs. 64%), non-English speaking (72% vs. 60%), and non-US born participants (72% vs. 66%).
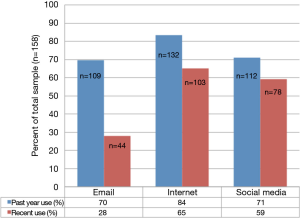
Past year use of email, Internet, and social media was reported by 70%, 84%, and 71% of participants, respectively (Figure 1). Recent use (within the last day) was less frequent ranging from 28% of the study sample for email use, to 65% for Internet use, to 59% for social media use. The difference in percentage reporting using email in the past year and percentage using email recently was 42%; differences in percentages between past year and recent use of Internet and social media were lower (less than 20%). Seventy percent of survey participants had a Facebook account, while 12% reported a Twitter account (Data not shown).
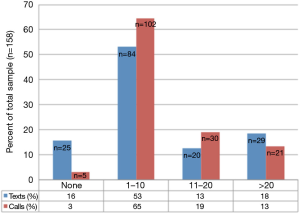
The use of cell phones for calls was nearly ubiquitous, with 97% of participants reporting at least one phone call daily (Figure 2). Text messaging via cell phone was also common: 84% of the sample indicated at least one text message sent or received daily, while about one-third reported over 10 daily text messages.
Table 2 shows demographic, obesity, and health measures by user status for email, Internet, social media, multimodal, and health information Internet use. Across most user types, users were younger than non-users; this was statistically significant for Internet and social media use. For health information Internet use, users were older than non-users (P=0.001). Similarly, users were more likely to be US born and have higher levels of education (P<0.05 for all but social media users). Users of email were more likely to be white and English speaking compared to non-users (P<0.05). In contrast, social media users and health information Internet users were more likely to be Hispanic (P=0.75 and 0.47, respectively) and Spanish speaking (P=0.60 and 0.10, respectively) compared to non-users.
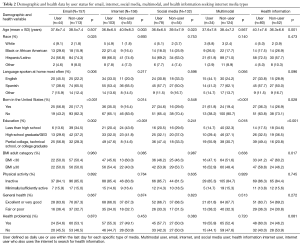
Full table
Table 2 also contains the health markers by user category. Internet, social media, multimodal, and heath information Internet users tended to be slightly more obese and inactive compared to nonusers, though this was not statistically significant. Likewise, all types of users tended to report poorer health and at least one health problem more often than nonusers, though this was also not statistically significant.
Discussion
In our study of ICT use in female residents of public housing, we found email, Internet, and social media use to be common, with cell phone use being particularly high. The majority of participants in this low-income population had a Facebook account (70%). Overall, users varied by demographic variables more than by health status.
Our results mirrored patterns of ICT use among the few studies done in similar populations as well as national data. In an assessment of ICT use in the Supplemental Nutrition Assistance Program population, 68% of participants who earned up to 185% of the federal poverty line had a mobile phone (27). In a clinical sample of single mothers, cell phone access was nearly ubiquitous (97%) as in our study (28). While over 85% of the study sample in Mitchell et al. reported texting and unlimited data, 26% reported service interruptions in the previous year, highlighting a challenge of using these technologies in a low SES population. Similar to our study, 87% of the sample reported social media use and 79% reported having a Facebook account. The broad use of these widely available media suggests these are feasible tools that could be used in the context of cancer prevention and control interventions.
Of note, we observed the contrast between past year use and recent use was greatest for email users, while the gap between infrequent and frequent use was smallest for social media users (i.e., use of social networking sites such as MySpace, Facebook, or LinkedIn.com). Especially given the younger age of study participants, our findings may reflect a national trend in technology use, where teens in particular are using more interactive technologies like social media rather than older technologies like email (29,30). The shift from email to interactive technologies and demographics such as age should be considered when developing interventions targeting modifiable health behaviors related to cancer. For example, in the CHOICES study, which focused on weight gain prevention among 18–35-year-old students attending U.S. community colleges, intervention group participants received access to an interactive study website that encourages social networking between participants as well as provision of information and support for weight management (31,32). Other research of current interventions in weight management are also capitalizing on recent advances in technology to deliver tailored approaches to individuals’ contexts (33). The approach of using new interactive technology-based intervention tools, particularly among younger age public housing residents is an avenue for future research.
We observed similar patterns of use compared to national samples, which include people of higher SES. The digital divide has diminished for Latinos and African Americans with respect to Internet use, and has closed for cell phone use and ownership (14,15). The prevalence of social media use nationally among Blacks is 73% and Latinos 84%, similar to the low-income population in our study. Of note, about 40% of Latinos use social media in Spanish or in combination with English, indicating the need to consider language when developing ICT cancer-related interventions.
Previous research suggests the preferred content of health messages differs by race and ethnicity (34). Hispanics in particular tend to use interpersonal networks more frequently as health resources (34,35). In our study, we found high use of social media sites by Hispanics, which may represent a virtual and electronic extension of interpersonal networks. Targeting interventions using social media may be a way to tap into these interpersonal networks to disseminate information about modifiable cancer prevention behaviors, cancer screening activities, or supportive resources for individuals undergoing cancer treatment or in survivorship phases. A systematic review of research about social media platforms among Hispanic populations reported a few intervention-based studies focused on diet and physical activity topics but also emphasized the need for further intervention-focused research (36). Furthermore, identifying influential community members who are interpersonal resources may be another way to disseminate health information, potentially through social networking sites. In a study to enhance health literacy through computer literacy, “health information mavens”, or interpersonal sources of general information, tended to have larger social networks and more civic engagement (37). Mavens also tended to have lower English language acculturation once again highlighting the need to consider the language used to deliver ICT interventions. Tailoring ICT intervention content may also improve attrition, which tends to be poor (38).
The generalizability of our results is limited by the setting of our study; our results may not be applicable to other low SES populations. This is particularly true given we look at a fairly young female sample. In addition, our questions about technology use were limited to a subset of participants; there may be a selection bias as the technology sample of the baseline sample was more Hispanic, non-US born, and Spanish speaking. However, public housing residents are a vulnerable population that is often not distinguished in national surveys and our study highlights the ICT capabilities of this low SES subset. Furthermore, there is a nationwide infrastructure for public housing, so there is a potential network to use effective interventions in other public housing sites.
One innovation of our study includes examining multimodal users. Most studies only consider one type of technology, while we measured multiple types of ICT users accessing several types of media. Multiple media may be required to successfully recruit and retain low SES study subjects (39). Hudnut and colleagues also emphasize the need for intervention-focused research to use multiple ICT platforms (e.g., texting and email) that can be complementary to social media platforms, which may work together to facilitate behavior change (36). Therefore, future intervention research among public housing populations could consider using telephone-based platforms to deliver a cancer-related behavior change intervention (e.g., encourage walking by delivering a motivational program increase self-efficacy and motivation to change using interactive voice response technology) and then complement this intervention with text message reminders to walk and/or a social media-based support group to encourage peer support for intervention participants.
In summary, ICT use is common among a sample of female public housing residents. Cell phones in particular were ubiquitous and may serve as intervention tools for interventions focused on cancer prevention and control in public housing settings. Finally, differences among profiles of users suggest mobile- and electronic-health-based public health interventions should consider targeting health messages to socio-demographic characteristics, such as age, ethnicity, and language.
Acknowledgements
The authors thank the Resident Health Advocates, Healthy Living Advocates, and public housing administration and residents who supported and participated in this research project.
Funding: This work supported by the Centers for Disease Control and Prevention Partners in Health and Housing Prevention Research Center (U48DP001922 to DJ Bowen).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Boston University Medical Campus Institutional Review Board.
References
- Bock BC, Rosen RK, Barnett NP, et al. Translating Behavioral Interventions Onto mHealth Platforms: Developing Text Message Interventions for Smoking and Alcohol. JMIR Mhealth Uhealth 2015;3:e22. [Crossref] [PubMed]
- Sarkar U, Gourley GI, Lyles CR, et al. Usability of Commercially Available Mobile Applications for Diverse Patients. J Gen Intern Med 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Horrigan JB. The mobile difference. Pew Internet Am Life Proj. March 25, 2009.
- Viswanath K, Nagler RH, Bigman-Galimore CA, et al. The communications revolution and health inequalities in the 21st century: implications for cancer control. Cancer Epidemiol Biomarkers Prev 2012;21:1701-8. [Crossref] [PubMed]
- Wildevuur SE, Simonse LW. Information and communication technology-enabled person-centered care for the "big five" chronic conditions: scoping review. J Med Internet Res 2015;17:e77. [Crossref] [PubMed]
- Bender JL, Yue RY, To MJ, et al. A lot of action, but not in the right direction: systematic review and content analysis of smartphone applications for the prevention, detection, and management of cancer. J Med Internet Res 2013;15:e287. [Crossref] [PubMed]
- Goode AD, Lawler SP, Brakenridge CL, et al. Telephone, print, and Web-based interventions for physical activity, diet, and weight control among cancer survivors: a systematic review. J Cancer Surviv 2015;9:660-82. [Crossref] [PubMed]
- Sanchez MA, Rabin BA, Gaglio B, et al. A systematic review of eHealth cancer prevention and control interventions: new technology, same methods and designs? Transl Behav Med 2013;3:392-401. [Crossref] [PubMed]
- Raaijmakers LC, Pouwels S, Berghuis KA, et al. Technology-based interventions in the treatment of overweight and obesity: A systematic review. Appetite 2015;95:138-51. [Crossref] [PubMed]
- Bush NE, Bowen DJ, Wooldridge J, et al. What do we mean by Internet access? A framework for health researchers. Prev Chronic Dis 2004;1:A15. [PubMed]
- Zickuhr K, Smith A. Digital differences. Pew Internet Am Life Proj [Internet]. 2012 [cited 2012 Nov 5]. Available online: http://alexa.pewinternet.com/~/media/Files/Reports/2012/PIP_Digital_differences_041312.pdf
- Smith A. Americans and their cell phones. Pew Internet Am Life Proj. August 15, 2011.
- Livingston G. The Latino Digital Divide: the native bordn versus the foriegn born. Pew Res Center’s Internet Am Life Proj. July 28, 2010.
- Lopez MH, Gonzales-Barrera A, Patten E. Closing the digital divide: Latinos and technology adoption. Pew Hispanic Center. March 7, 2013.
- Smith A. African Americans and technology use: A demographic portrait. Pew Res Center’s Internet Am Life Proj. January 6, 2014.
- Digenis-Bury EC, Brooks DR, Chen L, et al. Use of a population-based survey to describe the health of Boston public housing residents. Am J Public Health 2008;98:85-91. [Crossref] [PubMed]
- American Institute for Cancer Research and World Cancer Research Fund. Food, nNutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. Washington DC: American Institute for Cancer Research, 2007.
- Bowen DJ, Battaglia TA, Murrell SS, et al. What do public housing residents say about their health? Prog Community Health Partnersh 2013;7:39-47. [Crossref] [PubMed]
- Battaglia TA, Murrell SS, Bhosrekar SG, et al. Connecting Boston's public housing developments to community health centers: who's ready for change? Prog Community Health Partnersh 2012;6:239-48. [Crossref] [PubMed]
- Bowen D, Rus A, Beltrane C, et al. Walking groups: A simple, affordable intervention program for public housing developments. J Health Care Poor Underserved. In Press.
- Quintiliani LM, DeBiasse MA, Branco JM, et al. Enhancing physical and social environments to reduce obesity among public housing residents: rationale, trial design, and baseline data for the Healthy Families study. Contemp Clin Trials 2014;39:201-10. [Crossref] [PubMed]
- Rorie JA, Smith A, Evans T, et al. Using resident health advocates to improve public health screening and follow-up among public housing residents, Boston, 2007-2008. Prev Chronic Dis 2011;8:A15. [PubMed]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 1997;38:21-37. [Crossref] [PubMed]
- Booth M. Assessment of physical activity: an international perspective. Res Q Exerc Sport 2000;71 Suppl 2:114-20. [Crossref] [PubMed]
- Horrigan JB. A Typology of Information and Communication Technology Users. Pew Research Center. May 6, 2007.
- McNeill LH, Puleo E, Bennett GG, et al. Exploring social contextual correlates of computer ownership and frequency of use among urban, low-income, public housing adult residents. J Med Internet Res 2007;9:e35. [Crossref] [PubMed]
- Neuenschwander LM, Abbott A, Mobley AR. Assessment of low-income adults' access to technology: implications for nutrition education. J Nutr Educ Behav 2012;44:60-5. [Crossref] [PubMed]
- Mitchell SJ, Godoy L, Shabazz K, et al. Internet and mobile technology use among urban African American parents: survey study of a clinical population. J Med Internet Res 2014;16:e9. [Crossref] [PubMed]
- Lenhart A. A Majority of American Teens Report Access to a Computer, Game Console, Smartphone and a Tablet. Pew Research Center. April 9, 2015.
- Purcell K. Teens 2012: Truth, Trends, and Myths About Teen Online Behavior. Pew Res Cent Internet. July 11, 2012.
- Lytle LA, Moe SG, Nanney MS, et al. Designing a Weight Gain Prevention Trial for Young Adults: The CHOICES Study. Am J Health Educ 2014;45:67-75. [Crossref] [PubMed]
- Laska MN, Lytle LA, Nanney MS, et al. Results of a 2-year randomized, controlled obesity prevention trial: Effects on diet, activity and sleep behaviors in an at-risk young adult population. Prev Med 2016;89:230-6. [Crossref] [PubMed]
- Spruijt-Metz D, Wen CK, O'Reilly G, et al. Innovations in the Use of Interactive Technology to Support Weight Management. Curr Obes Rep 2015;4:510-9. [Crossref] [PubMed]
- Ahlers-Schmidt CR, Chesser A, Brannon J, et al. "Necesita una vacuna": what Spanish-speakers want in text-message immunization reminders. J Health Care Poor Underserved 2013;24:1031-41. [Crossref] [PubMed]
- Cheong PH. Health communication resources for uninsured and insured Hispanics. Health Commun 2007;21:153-63. [Crossref] [PubMed]
- Hudnut-Beumler J, Po'e E, Barkin S. The Use of Social Media for Health Promotion in Hispanic Populations: A Scoping Systematic Review. JMIR Public Health Surveill 2016;2:e32. [Crossref] [PubMed]
- Kontos EZ, Emmons KM, Puleo E, et al. Determinants and beliefs of health information mavens among a lower-socioeconomic position and minority population. Soc Sci Med 2011;73:22-32. [Crossref] [PubMed]
- Neve M, Morgan PJ, Jones PR, et al. Effectiveness of web-based interventions in achieving weight loss and weight loss maintenance in overweight and obese adults: a systematic review with meta-analysis. Obes Rev 2010;11:306-21. [Crossref] [PubMed]
- Nagler RH, Ramanadhan S, Minsky S, et al. Recruitment and Retention for Community-Based eHealth Interventions with Populations of Low Socioeconomic Position: Strategies and Challenges. J Commun 2013;63:201-20. [Crossref] [PubMed]
Cite this article as: Quintiliani LM, Reddy S, Goodman R, Bowen DJ. Information and communication technology use by female residents of public housing. mHealth 2016;2:39.