A mixed methods systematic review of success factors of mhealth and telehealth for maternal health in Sub-Saharan Africa
Introduction
Background
Maternity for several women in Africa and other areas of the world is synonymous with suffering, illness, even death. Thousands of women continue to die every year because of child bearing in spite of a significant reduction in mortality rate worldwide (a 43% reduction from 532,000 in 1990 to 303,000 in 2015) (1). Between 1990 and 2015, 7–10 million women worldwide died of maternal causes (1). It is estimated that two-thirds of those maternal deaths occur in Sub-Saharan Africa (1). Maternal mortality is therefore the one health indicator pointing to disparities between rich and poor countries. By 2015, regional maternal mortality rates ranged from 12 deaths per 100,000 live births in developed countries to 546 in Sub-Saharan Africa (1). Maternity also greatly contributes to the heavy burden of women’s illness (2). Eight millions women suffer every year of acute or chronic complications such as infections of the reproductive organs or urogenital tract fistula (3). In Asia and SSA, the World Health Organization (WHO) estimates that more than 2 million women have untreated obstetric fistula (3). These high rates of maternal mortality and morbidity have heavy social and health consequences on the survival of children and families’ financial health. A mother’s death increases the possibility of death of her children and the risks of developing problems in growing up. Neonatal mortality is therefore strictly linked to maternal mortality. In Africa, women are the pillars of the family and actively participate in the local economy and contribute to household revenues. They raise children and provide child healthcare. The illness or death of a mother can directly impact on the family by plunging it in precarious situations and delay education of children who are forced to work in order to help their family.
This explains why several countries, and developing countries in particular, have given priority to improving maternal health. In 2000, the international community decided to make it one of the eight Millennium Development Goals (MDGs). In 2010, during the MDG summit, the United Nations launched a world strategy for women and child health, and in 2015, the World Summit for Sustainable Development adopted the same objectives. Among the envisaged strategies, telehealth, and particularly mobile health, is expanding fully and is increasingly being acknowledged for its potential to reduce maternal morbidity and mortality (4). Nevertheless, its potential is little known in SSA although some promising experiences have been reported (5). In reducing geographical distance and facilitating rapid exchange of information, telehealth and mhealth could provide a precious improvement to healthcare services. Moreover, it could offer a platform to facilitate coherence and equity of access to healthcare treatment and services, as well as to fight “medical deserts” through the recruitment and retention of skilled health professionals in rural and remote areas (6). Telehealth and mhealth seem therefore relevant options for healthcare, particularly in developing countries where access to healthcare and treatments continue to be a serious problem for local populations. Nevertheless, a number of conditions must be met in order to guarantee the success of introducing and using telehealth in this context. Improving knowledge of these conditions for success would allow more efficient and sustainable implementation of telehealth and mhealth services by minimizing obstacles to their use and diffusion. It is thus important to summarize these conditions as they are essential for decision makers to guide interventions and plan adequate time and resources for project implementation.
Objective of the systematic review
This systematic review aims at providing a knowledge synthesis regarding success factors of introduction and use of telehealth and mhealth for maternal health in Sub-Saharan Africa.
Why is it important to conduct this systematic review
Several telehealth and mhealth interventions fail or do not go past the stage of pilot projects due to the ignorance of the factors underpinning success of introduction and use. This systematic review aims to identify these factors with the aim of making them available to decision-makers and managers working towards improvement of access to, and quality of, maternal healthcare services in SSA, but possibly also in other contexts.
Methods
We conducted a mixed methods systematic review in order to consider quantitative, qualitative and mixed method studies of mhealth and telehealth success factors for maternal health in SSA.
Protocol registration
The protocol for this systematic review is registered under the number CRD42016038692 in the PROSPERO database.
Criteria considered for inclusion
Types of studies
We included all original studies about mhealth or telehealth for maternal healthcare in SSA, published in English or French, using quantitative or qualitative or mixed methods. We put no limit on the date of publication.
Types of participants
The introduction and use mhealth and telehealth for maternal healthcare involve several actors. In this review, the participants were women of childbearing age (15–50 years), health professionals or other actors such as funding agencies, healthcare managers and technicians responsible for telehealth projects in maternal healthcare in SSA.
Types of interventions
We initially identified all telehealth or mhealth interventions for maternal health care in SSA. We then retained those that have identified success factors for the introduction or use of telehealth. We considered the WHO’s definition of telehealth: “the management and support to healthcare through interactive sound and visual communication of data” including “provision of basic healthcare services, consultation, access to database, management of health institutions, basic training, continuing education, research, monitoring of diseases and management of emergencies” (7). As for mhealth, the WHO defines it as an area of electronic health (ehealth) that provides health services and information via mobile technologies such as mobile phones and PDAs (personal digital assistant) (8). It is considered as a sub-category of telehealth. Interventions considered include applications related to tele-education, telemedicine and telematics (associating telecommunications and computer science) for healthcare. We have however excluded other categories of ehealth, such as information systems, that are not used directly to provide health care and services (9). Several media could be used (text, audio, video, etc.). Two types of communications were included:
- Simultaneous (in real time and/or synchrony) between two health professionals or between a patient and health professional;
- Differed (asynchronous) when data exchange does not require the simultaneous presence of a patient or healthcare providers (10).
This review specifically addressed mhealth and telehealth interventions for maternal health. Maternal heath includes all aspects of women’s health, from pregnancy to postpartum. It can also include postpartum interventions, regular birth, obstetric emergencies or post-partum follow-up. The context of the intervention includes health infrastructure, primary care and specialized treatment, and the community in the 48 SSA countries identified by the World Bank (11).
Types of comparisons
Telehealth or mhealth intervention versus non-telehealth intervention or usual care.
Types of results
The main results of interest were the success factors of mhealth and telehealth. The concept of success is complex in that it relates to a perception which varies in time, according to the context, and according to the perspective of the observer (12). Specialized literature offers two definitions of success of telehealth which are particularly relevant to this work. The first one is Wootton and Hebert’s (13) definition which states that a successful application produces high quality treatment at a low cost. The second definition considers the continuity and permanence of a telehealth program as an indicator of its success (14). In other words, the success of a telehealth application can be assessed on the basis of its sustainability. Although several telehealth projects are in fact medically and technically viable solutions, their permanence constitutes a major challenge (14), especially in developing countries (15).
Several factors can determine the success of telehealth introduction and implementation. In a systematic review, Van Dyk (9) identified and compared nine frameworks for telehealth implementation which could contribute to study their success. These frameworks were drawn from different theories and projects. They are grouped depending on whether they deal with the diffusion of telehealth (16), the concept of e-readiness (17), the use of the Unified Theory of Acceptance and Use of Technology (UTAUT) (18), the use of a global model for telehealth evaluation, project life cycles (19,20) or guidelines that are not based on a particular theory (21-23). These frameworks sometimes overlap on certain themes such as technology, organizational structures, change management process, economic feasibility, societal impacts, perceptions, user-friendliness, evaluation, legislation, politics and governance, but none of them covers all these themes simultaneously.
For this review, we used a framework inspired from that of Broens et al. (19), which we found to be the most appropriate given its focus on both success factors at the pilot phase and those that are key to sustainability. For these authors (19), the extent to which technology is accepted by users and society determines the success of the pilot phase. But once the pilot project has been scaled up, financial factors and organizational considerations become key determinants of the success of telehealth services. Based on this framework, we classified telehealth success factors into five main categories: (I) technology; (II) acceptance by healthcare professionals and patients; (III) funding; (IV) organization and (V) politics and legislation.
Studies identification strategy
The following databases were consulted: PubMed, Web of Science, Embase, Scopus, and CINHAL. Additional searches were done on Google Scholar. We used concepts grouped into three categories of interest: telehealth (e.g., telehealth, telemedicine, mHealth and telecare), maternal health, and the geographical area (Africa) on each database to identify keywords that generated the most relevant results.
For each database, we searched the combinations of keywords and their related terms, using controlled or free vocabulary. Once results were generated on the database, they were grouped in bibliographic management software and duplicate records were eliminated.
Pairs of authors made a first selection independently from reading the titles and abstracts. In case of disagreement, and if consensus was not found, a third author acted as arbitrator. In case of doubt, the full article was read to decide. To ensure completeness of the literature review, we consulted the reference lists and conducted a citation tracking of included studies to identify any other relevant publications. All publications finally selected were downloaded and fully read in order to extract data.
Extraction, analysis and synthesis of data
First, we performed a descriptive analysis of all included studies to document their main characteristics: (I) title, first author and year of publication; (II) main goal of the study; (III) methodological approach; (IV) sampling strategy and characteristics of participants; and (V) main results according to the prosed classification. Second, we used the framework adapted from Broens et al. (19) to classify success factors into the proposed five categories and an analysis was made within and between categories. A narrative synthesis of studies results was produced to present the main findings regarding determinants of telehealth success for maternal health in SSA.
Assessment of studies quality
Although there is limited consensus on how to assess methodological quality in mixed methods review (24), the Mixed Methods Appraisal Tool (MMAT) seems to be the best indicated to assess concomitantly the quality of qualitative, quantitative and mixed methods studies (25). Two reviewers (Mohamed Ali Ag Ahmed, Marie-Pierre Gagnon) independently evaluated the methodological quality for each article using the MMAT and completed the data extraction table.
Results
Characteristics of included studies
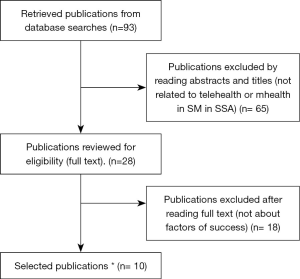
In total, we identified 93 references using the search terms from the databases. After reviewing titles and abstracts, 65 articles were excluded because they were not about telehealth/mhealth for maternal healthcare in SSA. Thus, 28 publications met initial inclusion criteria and were selected for a full-text review. Of these, 18 were excluded because they did not identify success factors for the implementation or use of telehealth. Thus, ten publications were selected in the final review. Among these, three articles (26-28) reported on a same study, and two other publications (29,30) were also related to a single study. Therefore, seven studies were finally included in the review. The study selection flow diagram is presented in Figure 1.
The characteristics of included studies are summarized in Table 1. All studies were published between 2009 and 2015. Interestingly, more than half were published during the last three years and all but one were specifically on mhealth. Two studies used theoretical frameworks. Only one study was conducted in west Africa (Ghana) (31). They were all pilot studies and most focused on the collection and transmission of health and management information (26,28-30,32).

Full table
Studies were diverse in terms of sample size and population, duration of intervention, delivery system, and type of control. The sample sizes ranged from 30 to 4,768 participants and the duration from 4 weeks to 26 months.
Overview of telehealth success factors
Factors related to technology
Technological factors were the most documented in relation to the success of telehealth projects. Six studies (26,30,32-34) have shown that availability of technical support to maintain and troubleshoot the system led to positive perceptions among users and increased their use of the technology. Having good network coverage was also highlighted in two studies (26,33). Similarly, user-friendliness of the applications (e.g., devices with a touch screen, a more readable keyboard, and more aesthetic) would facilitate the use of the technology (26,31). For instance, small telephone keypad was likely to lead to errors in the recording of data, whereas touch-screen phones were more reliable (31). Moreover, the existence of an energy source (solar chargers, back-up batteries) for charging devices (28,33), replacement of failing or lost telephones (33), and privacy protection (31,32) were also important elements influencing the success of telehealth projects. Some authors proposed protecting the data with a password since cell phones were shared between staff and members of their families (31). User involvement in design and implementation (27,33), a good understanding of clinical practice by upstream designers, and the implementation of tools such as manuals would facilitate the correct use of the technology (26).
Factors related to user acceptance of technology
A good acceptance of the technology by users (health workers or parturient) is fundamental for the success for telehealth projects. Studies identified motivation and commitment (26,33), and perceived utility for work (26,32) as important success factors. Also, the technology must meet staff demands (28,33) or their needs and expectations (28,31). For example, in the study by Vélez et al. (31), midwives were more interested in collecting data for their periodic reports than for clinical decision-making. Moreover, giving telephones to end users (27) and training them in their use would promote their appropriation and acceptance (31-33). Thus, an adequate level of literacy (29) or competent agents (26) who have previous experience of use (29) would increase acceptance of the technology. For example, having a literate person nearby can help traditional birth attendants to use some advanced telephone functions such as creating and sending SMS and adding credit (30). The use of the local language (26,27), interaction between participants through personalized messages, and the adaptation and integration of the technology to the environment in which it is located were other success factors identified.
Factors related to funding
Funding, although little documented in the included studies, is an essential condition for the success of telehealth projects. It may include the purchase of devices and software, payment for mobile services and, more generally, financing for telehealth projects. In SSA, funding for telehealth projects is further expanded from outside. In the reviewed studies, success factors related to financing include a strong commitment from the private sector to finance telehealth projects (26,33), notably for reducing communication costs (33).
Factors related to the organization
The existence of a well-organized health system and effective coordination of telehealth interventions seem essential. This requires strengthening the capacity of the health team to better manage and supervise activities (33). Hence, the stability of the staff in their posts is important (28,33), which is often a challenge in SSA. In addition, the increased workload for health workers with the introduction of the new technology must be taken into account and compensated (26). Similarly, stakeholder roles must be well delineated and their application well integrated into their practices (33).
Legislative and regulatory factors
These are the least documented aspects in the studies reviewed. Only one study reported the importance of strong commitment from the government to support telehealth projects, especially when it comes to their deployment on a scale (33). To achieve this commitment, projects should be relevant to the needs and priorities of health systems and should be integrated with the national strategies of the countries concerned.
Discussion
Seven studies that identified success factors for the implantation and use of telehealth and mhealth in maternal health in SSA were included in this mixed methods systematic review. Our results are complementary to those reported by Aranda-Jan et al. (5) about mhealth projects in SSA. Unlike the latter, our review has been expanded to include telehealth and we used no date limitations. However, our review only concerned maternal health and focused on factors of success, not on the effects or impact of interventions. However, some of the success factors identified are echoed in the review by Aranda-Jan et al. (5).
The small number of studies and their recent nature indicate that telehealth for maternal health in SSA remains little explored although there is an increasing interest in this field. Our review also shows limited scientific evidence on the factors influencing the successful implementation and use of telehealth for maternal health in SSA. Indeed, none of the reviewed study specifically focused these factors; they were rather addressed as secondary results or in the discussion. In fact, the main purpose of the studies reviewed was to document the effectiveness of telehealth interventions. However, in order to ensure intervention effectiveness, it is important to consider factors that could lead to the success or failure of telehealth projects from the design of interventions to their scaling up.
The fact that six out of the seven studies reviewed focused on mhealth is most likely due to the significant penetration of mobile telephony in SSA, its affordability and ease of use. All studies were in the pilot phase, which would explain why success factors related to the technology and its acceptance were the most documented, as suggested by Broens et al. (19). The factors identified were mostly related to the design of the project and its adaptation to the context of implementation. Thus, these factors are likely to change when the interventions are scaled up.
Furthermore, many of the success factors identified do not appear to be specific to maternal health, and could be relevant for other health domains. This is the case for most factors related to technology, user acceptance, funding and organizational support. However, some of the factors identified in our review are debated in the literature. This is the case, for instance, of the limitation of free communication time or the use of devices belonging to users versus the provision of new devices (35,36). These measures are sometimes proposed to limit the costs of telehealth interventions. Some authors believe that limiting the use of phones strictly for professional purposes would undermine user commitment (27). Also, it was reported that health workers do not like to use their personal phones for work (33). Difficulties in providing technical support to workers using their personal phones were also highlighted (37,38). This is why free communication time was provided in some projects as a means to increase users’ motivation and their appropriation of the intervention (33). Moreover, users’ expectations in terms of confidentiality remain a controversial topic in the literature. In some cases, technology could be seen as a way to protect confidentiality, as illustrated by the study on the use of mobile phone interviews that enable HIV-infected parturients to maintain their privacy and reduce the feeling of being observed in face-to-face consultations (39).
Conclusions
Our review is consistent with the existing literature which generally notes that telehealth, and mhealth in particular, is still at an early stage in SSA. However, several authors agree that the prospects are promising. In addition, the limited scientific evidence regarding telehealth benefits could be partly explained by a systematic failure to take into account the success factors in the implementation and use of telehealth during project design. This review confirms that telehealth success factors are poorly documented in SSA. More research is needed to better identify these factors based on conceptual frameworks, which could contribute to the success of telehealth and mhealth implementation, as well as their expansion on a large scale and their sustainability. This is why we advocate for specific studies that will focus on these factors of success and take them into account in project design to maximize the chances of successful telehealth interventions in SSA, but also elsewhere.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. The Lancet;387:462-74.
- Goodburn E, Campbell O. Reducing maternal mortality in the developing world: sector-wide approaches may be the key. BMJ 2001;322:917-20. [Crossref] [PubMed]
- World Health Organization, UNICEF, UNFPA and The World Bank. Trends in Maternal Mortality: 1990 to 2008. Estimates developed by WHO, UNICEF. UNFPA and The World Bank. Geneva: World Health Organization, 2010.
- Lee SH, Nurmatov UB, Nwaru BI, et al. Effectiveness of mHealth interventions for maternal, newborn and child health in low-and middle-income countries: systematic review and meta-analysis. Edinburgh University Global Health Society, 2016.
- Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 2014;14:188. [Crossref] [PubMed]
- Bagayoko CO, Traoré D, Thevoz L, et al. Medical and economic benefits of telehealth in low- and middle-income countries: results of a study in four district hospitals in Mali. BMC Health Serv Res 2014;14 Suppl 1:S9. [Crossref] [PubMed]
- Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine; Field MJ, editor. The National Academies Collection: Reports funded by National Institutes of Health. Telemedicine: A Guide to Assessing Telecommunications in Health Care. Washington (DC): National Academies Press (US), 1996.
- Källander K, Tibenderana JK, Akpogheneta OJ, et al. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low-and middle-income countries: a review J Med Internet Res 2013;15:e17. [Crossref] [PubMed]
- Van Dyk L. A Review of Telehealth Service Implementation Frameworks. Int J Environ Res Public Health 2014;11:1279-98. [Crossref] [PubMed]
- Deshpande A, Khoja S, Lorca J, et al. Asynchronous telehealth: a scoping review of analytic studies. Open Med 2009;3:e69-91. [PubMed]
- The World Bank. World Bank Country and Lending Groups. Avaible online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups
- Whetton S. Successes and failures: what are we measuring? J Telemed Telecare 2005;11:S98-100. [Crossref] [PubMed]
- Wootton R, Hebert M. What constitutes success in telehealth? J Telemed Telecare 2001;7:S-7. [Crossref] [PubMed]
- Cradduck T. Sustainability—the Holy Grail of telehealth? J Telemed Telecare 2002;8:7-8. [Crossref] [PubMed]
- Luna D, Almerares A, Mayan JC, et al. Health Informatics in Developing Countries: Going beyond Pilot Practices to Sustainable Implementations: A Review of the Current Challenges. Healthc Inform Res 2014;20:3-10. [Crossref] [PubMed]
- Tanriverdi H, Iacono CS. Knowledge barriers to diffusion of telemedicine. Proceedings of the international conference on Information systems. Helsinki, Finland: Association for Information Systems, 1998:39-50.
- Khoja S, Scott RE, Casebeer AL, et al. e-Health readiness assessment tools for healthcare institutions in developing countries. Telemed J E Health 2007;13:425-31. [Crossref] [PubMed]
- Venkatesh V, Morris MG, Davis GB, et al. User acceptance of information technology: Toward a unified view. MIS Quarterly 2003.425-78.
- Broens TH. Determinants of successful telemedicine implementations: a literature study. J Telemed Telecare 2007;13:303-9. [Crossref] [PubMed]
- Khoja S, Durrani H, Scott RE, et al. Conceptual framework for development of comprehensive e-health evaluation tool. Telemed J E Health 2013;19:48-53. [Crossref] [PubMed]
- Finch TL, Mair FS, May CR. Teledermatology in the UK: lessons in service innovation. Br J Dermatol 2007;156:521-7. [Crossref] [PubMed]
- Leon N, Schneider H, Daviaud E. Applying a framework for assessing the health system challenges to scaling up mHealth in South Africa. BMC Med Inform Decis Mak 2012;12:123. [Crossref] [PubMed]
- Yellowlees PM. Successfully developing a telemedicine system. J Telemed Telecare 2005;11:331-5. [Crossref] [PubMed]
- O'Cathain A, Murphy E, Nicholl J. The quality of mixed methods studies in health services research. J Health Serv Res Policy 2008;13:92-8. [Crossref] [PubMed]
- Pluye P, Gagnon MP, Griffiths F, et al. A scoring system for appraising mixed methods research, and concomitantly appraising qualitative, quantitative and mixed methods primary studies in Mixed Studies Reviews. Int J Nurs Stud 2009;46:529-46. [Crossref] [PubMed]
- Medhanyie AA, Little A, Yebyo H, et al. Health workers’ experiences, barriers, preferences and motivating factors in using mHealth forms in Ethiopia. Hum Resour Health 2015;13:2. [PubMed]
- Little A, Medhanyie A, Yebyo H, et al. Meeting community health worker needs for maternal health care service delivery using appropriate mobile technologies in Ethiopia. PloS One 2013;8:e77563. [Crossref] [PubMed]
- Medhanyie AA, Moser A, Spigt M, et al. Mobile health data collection at primary health care in Ethiopia: a feasible challenge. J Clin Epidemiol 2015;68:80-6. [Crossref] [PubMed]
- Perosky JE, Munro ML, Kay JL, et al. Texting From the Bush: Data Collection Using SMS Text Messaging in Areas of Low Network Coverage From Low-Literacy Providers. J Health Commun 2015;20:1052-9. [Crossref] [PubMed]
- Munro ML, Lori JR, Boyd CJ, et al. Knowledge and skill retention of a mobile phone data collection protocol in rural Liberia. J Midwifery Womens Health 2014;59:176-83. [Crossref] [PubMed]
- Vélez O, Okyere PB, Kanter AS, et al. A usability study of a mobile health application for rural Ghanaian midwives. J Midwifery Womens Health 2014;59:184-91. [Crossref] [PubMed]
- Van Heerden A, Norris S, Tollman S, et al. Collecting maternal health information from HIV-positive pregnant women using mobile phone-assisted face-to-face interviews in Southern Africa. J Med Internet Res 2013;15:e116. [Crossref] [PubMed]
- Ngabo F, Nguimfack J, Nwaigwe F, et al. Designing and Implementing an Innovative SMS-based alert system (RapidSMS-MCH) to monitor pregnancy and reduce maternal and child deaths in Rwanda. Pan Afr Med J 2012;13:31. [PubMed]
- Solano M, Kim E, Christiansen M, et al. Asynchronous telemedicine with ultrasound: Improving maternal health in developing countries. Ultrasonics Symposium (IUS), 2009 IEEE International.
- Asiimwe C, Gelvin D, Lee E, et al. Use of an innovative, affordable, and open-source short message service-based tool to monitor malaria in remote areas of Uganda. Am J Trop Med Hyg 2011;85:26-33. [Crossref] [PubMed]
- Barrington J, Wereko-Brobby O, Ward P, et al. SMS for Life: a pilot project to improve anti-malarial drug supply management in rural Tanzania using standard technology. Malar J 2010;9:298. [Crossref] [PubMed]
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health 2006;2:9. [Crossref] [PubMed]
- Chib A. The Aceh Besar midwives with mobile phones project: Design and evaluation perspectives Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? using the information and communication technologies for healthcare development model. Journal of Computer-Mediated Communication 2010;15:500-25. [Crossref]
- Zurovac D, Talisuna AO, Snow RW. Mobile phone text messaging: tool for malaria control in Africa. PLoS Med 2012;9:e1001176. [Crossref] [PubMed]
Cite this article as: Ag Ahmed MA, Gagnon MP, Hamelin-Brabant L, Mbemba GI, Alami H. A mixed methods systematic review of success factors of mhealth and telehealth for maternal health in Sub-Saharan Africa. mHealth 2017;3:22.


