m-Health interventions for diabetes remote monitoring and self management: clinical and compliance issues
Mobile diabetes remote monitoring and self-management has been one of the early application areas of mobile health (m-health) (1). This proliferation has been reflected in the numerous pilot studies and the proliferation of hundreds of commercial diabetes applications (apps) and mobile self-management systems since 2007 (2). This is compounded with the recent advances and global popularity of m-health for diabetes self-management and care. It is well known that m-health can provide a vital and important opportunity for alleviating the massive global healthcare challenges and economic burdens associated with diabetes and its long term complications. In this concept, the individual patients play the central participatory role in their diabetes self-management and care process via their smart mobile phone apps that will allow better education and awareness of their disease condition. The clinical benefits of diabetes self-management for both patients and healthcare providers are established. These can be summarised as (2):
- To empower people with diabetes to self-monitor blood glucose (SMBG) or other variables when and as needed (e.g., blood pressure, weight, and diet);
- To engage people in the management of their diabetes by promoting self-efficacy;
- To achieve pre-set care targets and to provide interactive feedback between patients and physicians with respect to disease progress and adherence to therapy;
- To allow physicians to facilitate patient self-care, to improve outcomes with potential cost savings.
These combined advantages complement and support the general clinical values and utility benefits of self-monitoring of blood glucose (SMBG). SMBG is an important clinical adjunct to hemoglobin A1c (HbA1c) testing and control. This is because SMBG can identify and distinguish among fasting, preprandial, and postprandial hyperglycemia; detect glycemic excursions; identify and assist in the monitoring of hypoglycemia. Furthermore, SMBG can also provide the appropriate feedback information back to the diabetic patients on the effects of their food intake, activity, and medication compliance and the impact of these lifestyle and diet factor on their glycemic control (3).
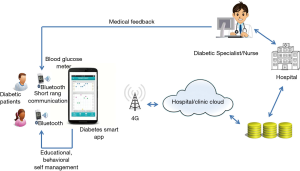
The basic principle of mobile diabetes management system is show in Figure 1 (1,2,4).
The general architecture of m-health diabetes self-management and care systems consist of the following modules (1,2):
- The patient end, which consists of a smart phone equipped with a special diabetes app connected wirelessly via Bluetooth to a blood glucose meter and used for tracking and storing the patient’s daily blood glucose data and status. Hypertensive individuals with diabetes may also be given a wireless blood pressure device and weight scales as required. The patient is then required to complete basic training and an educational program on using these systems;
- The acquired blood glucose data are usually transmitted wirelessly via the individual patient’s smart phone and stored in a remote portal hosted in a health clinic or hospital. This portal consists of the patient’s EHR, supported with intelligent data analytic tools that can process the data and produce simple illustrative graphics. These can be accessed and viewed by the patient and physician via two separate web portals, each designed and developed for separate access. The graphics provide information and decision support messages, such life style change, educational notes, and medication required to improve the patient’s daily management routine;
- The adaptation of any medication and treatment plans required for individual patients. This is based on their self-management history, daily blood glucose profiles, treatment progress, and designated therapy protocol plans assessed regularly at 3–6 months follow-up intervals.
The schedule and frequency of taking daily blood glucose readings and other medical data are dependent on the individual care plan made for each patient by their specialist and based on their individual diabetes type, treatment and progress. The timings of these readings are usually programmed in the patient’s smart phone app as reminders to take readings according to pre-set schedules. Smart devices, such as continuous glucose monitors (CGM) and continuous subcutaneous insulin infusion (CSII) pumps used by people with type 1 diabetes (T1D), can also communicate wirelessly to their smart phones for monitoring their purposes. Patients are usually required to test their blood glucose concentrations several times daily, usually before meals and 2–4 hours after meals.
The basic principles of m-health interventions used for digital diabetes care and self-management depend on the following tasks usually embedded in most of the current smart phone apps (1,2):
- Mobile blood glucose self-measurements and logging;
- Improved diet and healthy eating;
- Better physical exercise;
- Medication adherence;
- Enhanced education and awareness;
- Insulin dosage calculation;
- Real time feedback and information exchange between patient and doctors.
There are other secondary tasks or functionalities that can be included in these smart apps as required clinically.
From the clinical perspective, the volume of the clinical studies and randomised clinical trials reported in recent years on the effectiveness of mobile diabetes management for both type-1 diabetes (T1D) and type-2 diabetes (T2D) patients are well documented (1,2). A review study estimated that 212 articles published on m-health for diabetes care and self-management since 2010. However, only 20 of these were considered as valid robust clinical studies (5). The usual randomized controlled trials (RCTs) and other clinical observational studies typically categorise these m-health interventions into T1D or T2D interventions. Another recent review of 15 systematic reviews and meta-analysis studies of these m-health interventions published between 2008 and 2014 including 52 unique studies, mostly were RCTs have shown a clear impact of the m-health intervention for both types (6). This review demonstrated that on average, mobile phone-based interventions with clinical feedback improve glycemic control (HbA1c) compared to standard care or other non-m-health approaches by as much as 0.8% for patients with T2D and 0.3% for patients with T1D, at least in the short-term (≤12 months) (6). However, another meta-analysis study of (15 RCT) of m-health interventions for T2D has shown that the overall effect on HbA1c from these studies had shown that the mean difference (MD) was −0.40% (−4.37 mmol/mol) [95% confidence interval (CI), −0.69% to −0.11% (−7.54 to −1.20 mmol/mol); P=0.007] and the standardized mean differences (SMD) was −0.40% (−4.37 mmol/mol) [95% CI, −0.69% to −0.10% (−7.54 to −1.09 mmol/mol); P=0.008] (7). These outcomes indicate that the clinical benefits of e m-health interventions are clearly beneficial for diabetes patients and healthcare providers in providing better glycemic control and also improved quality of life and other outcomes. However, larger and more robust clinical studies with empirical evidence are still needed in this area.
Although, there has been major advances in m-health technologies for diabetes care in the last decade. There are still major challenges in both technical and clinical areas. These include for example; regulatory and efficacy challenges (8), long terms patient compliance and usage (9), behavioural change (10), security and privacy issues (1) among others. These and other challenges constitute major barriers in this area. These require further research and work for the development of the next generation of m-health systems that will allow the wider usage and clinical acceptability of these innovations in the future of digital diabetes care and management systems.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
ReferencesOther Section
- Istepanian RSH, Woodward B. m-Health: Fundamentals and Applications. Hoboken, NJ: Wiley-IEEE Press, 2017.
- Istepanian RSH, Casiglia D, Gregory JW. Mobile health (m-Health) for diabetes management. British J Health Management 2017;23:3.
- Dailey G. Assessing glycemic control with self-monitoring of blood glucose and hemoglobin A(1c) measurements. Mayo Clin Proc 2007;82:229-35. [Crossref] [PubMed]
- Alanzi T, Istepanian R, Philip N. Design and Usability Evaluation of Social Mobile Diabetes Management System in the Gulf Region. JMIR Res Protoc 2016;5:e93. [Crossref] [PubMed]
- Garabedian LF, Ross-Degnan D, Wharam JF. Mobile Phone and Smartphone Technologies for Diabetes Care and Self-Management. Curr Diab Rep 2015;15:109. [Crossref] [PubMed]
- Kitsiou S, Paré G, Jaana M, et al. Effectiveness of mHealth interventions for patients with diabetes: An overview of systematic reviews. PLoS One 2017;12:e0173160. [Crossref] [PubMed]
- Cui M, Wu X, Mao J, et al. T2DM Self-Management via Smartphone Applications: A Systematic Review and Meta-Analysis. PLoS One 2016;11:e0166718. [Crossref] [PubMed]
- Istepanian RSH. Mobile Applications (Apps) for Diabetes Management: Efficacy Issues and Regulatory Challenges. The Lancet 2015;3:921-3. [PubMed]
- Istepanian RS, Sungoor A, Earle KA. Technical and compliance considerations for mobile health self-monitoring of glucose and blood pressure for patients with diabetes. Conf Proc IEEE Eng Med Biol Soc 2009;2009:5130-3. [PubMed]
- Alanzi TM, Istepanian RS, Philip N. A Novel Smart Approach for Social Behavioral Change Intervention and Management for Saudi Diabetic Patients. 7th International Conference on Advanced Technologies & Treatments for Diabetes, Austria, 2014.
Cite this article as: Istepanian RS, Al-anzi TM. m-Health interventions for diabetes remote monitoring and self management: clinical and compliance issues. mHealth 2018;4:4.