Assessing operating room turnover time via the use of mobile application
Introduction
It is well known that the hospital operating room (OR) is the single most important component in the delivery of healthcare within perioperative services. Not only do hospital ORs provide a critical service by accommodating many types of procedures and serving the community’s surgical needs, but ORs also generate more cost and revenue than any other function within the hospital. For these reasons, hospitals pay close attention to the efficiency of their ORs. It is estimated that 15% of the total OR time is wasted in every operative month (1). The factors contributing to the time waste are inappropriate patient preparation, surgeon unavailability, insufficient staffing (nurses and anesthesiologists), congestion of the post anesthesia care unit, equipment sterilization issues, and transport delays (1). The majority of the time waste revolves around non-operative time, and this is also the portion where there is the most opportunity for improvement. Non-operative time means that staff time, a key OR operating cost, is being focused on tasks not directly related to providing surgical care.
To improve OR performance, this research focuses on the reduction of turnover time (TOT). OR efficiency can be measured from the length of TOT (2). Furthermore, the length of TOT is seen as a source of delays in starting procedures (3). In this research, TOT is defined as the “procedure finish” time of the preceding surgical case to “procedure start” time of the following surgical case (4). If TOT can be decreased, then the OR’s throughput would increase and thereby improve the hospital’s revenue (5-7). Moreover, reducing TOT length will reduce overtime in the OR (8) and help increase patient satisfaction by increasing the timeliness of procedure start times (9).
The use of mobile computing and communication technologies in healthcare settings is a rapidly expanding area. To improve healthcare service delivery processes, Free et al. investigated several mobile technology-based interventions and found that short message service (SMS) text appointment reminders significantly increase patient attendance compared to no reminders (10). Boulos et al. developed a mobile application to help healthcare professionals remotely monitor and manage older patient with multiple chronic conditions (11). Kaplan presented the successful use of mobile phones to support telemedicine and remote healthcare in developing countries (12). Additionally, Martinez et al. highlighted the use of mobile phones in off-site medical diagnosis in developing countries (13). Lane et al. successfully implemented an integrated mobile situational awareness application at Vanderbilt University Medical Center (14). Their mobile application is capable of providing a visual map of the flow of patients through the operative suite and prioritizing which patients need attention. Recently, Uddin et al. investigated the use of voice recognition technology in perioperative services to enable staff to record workflow milestones using mobile technology so that patient flow and quality of care could be improved (15).
This study builds on our previous work which evaluated the effectiveness of an app that implements an OR countdown timer for one OR unit of Greenville Memorial Hospital (GMH) in South Carolina (4). The app was revised based on findings from the prior study (4). This study generalizes our previous finding by collecting data and assessing the app’s effectiveness for the timely completion of turnovers in another OR unit of GMH. It is hypothesized that using the countdown timer app will improve turnover success (i.e., the TOT is equal to or less than the allotted time). Specifically, this study evaluates: (I) the effectiveness of the use of the mobile app in meeting OR TOT benchmarks; and (II) the factors that contribute to prolonged OR TOT as well as the impact of each delay factor on OR TOT.
Methods
Mobile application development
We initially met with the hospital’s director of perioperative services to discuss opportunities to enhance OR efficiency. The director showed us a laptop-based excel spreadsheet he had developed to track TOT in the OR. He expressed interest in working with us to transition the tool to a tablet-based mobile application. We then developed a functional Android prototype of the app, named ORTimer, and presented it at a meeting with the director and a group of stakeholders, including surgeons, anesthesiologists, certified registered nurse anesthetists (CRNA), and OR nurses. The CRNA supervisor and CRNAs at the meeting volunteered to pilot the use of the app in an OR. The stakeholders also suggested several modifications to the app’s interface and a few added functions.
We refined the app based on the list of change requests and delivered the new prototype to the two CRNAs who had attended the previous meeting. We provided the app on three Google Nexus tablets for testing during the performance of surgical procedures in a few ORs. We then pursued a series of test-refine-retest cycles with these CRNAs. The CRNAs reported they were having difficulty in achieving “buy-in” from the entire team of over 40 CRNAs to adopt the app. We decided at this point to radically reduce the functionality and associated interface complexity of the app. For example, rather than collect timing data and causes of delays for four relatively distinct phases of the OR turnover—procedure finish to patient out of room, patient out of room to next patient in room, next patient in room to anesthesia ready, and anesthesia ready to procedure start—we elected to collect timing data and causes of delay for only the entire turnover. This greatly reduced the amount of time and effort the CRNAs needed to devote to the app during a turnover. Collectively, the management, the users, and the developers recognized that the CRNAs, while potentially willing to serve as the users of the app, already had several patient-centered tasks to complete. We agreed it was necessary to reduce the intrusiveness of the app in the OR at the expense of being able to collect fine-grained detail on the durations of each phase of the turnover and the times at which specific sorts of delays occurred. At this point, the OR timer application was implemented in ORs for daily use.
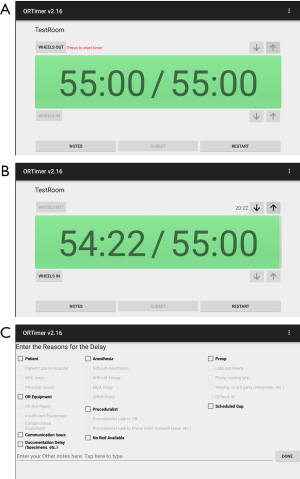
The ORTimer app runs on an Android tablet, and in some ORs, the display was mirrored on the large monitor. The application has a large green timer countdown bar which shows both the total allotted time and the remaining time. Both numbers start out with the same value (Figure 1A). The timer starts the countdown when the user taps on the “Wheels Out” button and stops when the user taps on “Wheels In” (Figure 1B). The bar turns red when 90% of the allotted time has passed. There are up and down arrow buttons for changing the start time and the end time of the timer, in case the CRNA forgets to press either (Wheels Out or Wheels In) at the exact time. The “Notes” button takes the user to a separate screen with checkboxes where the user can identify the reasons for a delay (Figure 1C). This screen also has a textbox where the user can make general comments. All data are saved to the device. There is also an administrative screen from which we can send out an email containing the data.
Description of OR units
The Memorial Medical Office Building (MMOB) Gastro Intestinal Laboratory (GI-Lab) at Greenville Health System conducts 7,500 endoscopy procedures each year. The unit is a non-sterile environment with six ORs. The case load primarily consists of colonoscopy and esophagogastroduodenoscopy cases, and general anesthesia is the primary method of sedation. Nurses in this area are cross-trained to routinely work in each area of care (preoperative, intraoperative, and recovery).
The D-Core, on the other hand, is part of the larger Greenville Memorial Hospital (GMH), which is designated as a level 1 trauma center. This means that they must have a room and staff to accommodate a trauma at any hour of the day. The entire OR routinely performs 25,000 cases per year. The D-core consisting of eight rooms performs 6,000 cases per year. This core area must also abide by sterile protocols and generally uses much more equipment to perform cases. The D-core performs most cases with general anesthesia and the case load primarily consists of orthopedic, orthopedic trauma, neurological, and general surgical cases. Nurses in this area are trained specific to their specialty and work area (i.e., preoperative nurses won’t work in the OR and vice versa).
Data collection
The ORTimer app was used in the D-core of GMH from May 1, 2016 to August 15, 2016. The tablets with the ORTimer app installed were placed above the computer at the anesthesia workstation using off-the-shelf tablet mounting hardware. The CRNA was responsible for recording the event milestones and recording the delay reasons, if applicable. To minimize the CRNAs’ workload, the tablets and ORTimer apps were automatically turned on at the beginning of the day using a third-party software. This setup made it more convenient for the CRNAs to use the app.
The ORTimer app was used in the GI-Lab of the MMOB at Greenville Health System from November 28, 2016 to March 3, 2017. In contrast to the D-core implementation, the nurses were directed to use the application to record TOTs between surgical cases instead of the CRNAs.
The staff recorded the primary reasons (i.e., patient, OR equipment, anesthesia, surgeon, Preop, documentation delay, and scheduled gap) for the delay (Figure 1C). More than one primary reasons can be selected for one delay if multiple reasons contributed to the prolonged TOT. Additionally, the app collected the elapsed TOT between the preceding and following surgical cases. Perioperative management at GMH set the TOT benchmark for GI-Lab at 16 and 75 minutes for D-Core. Additional OR case information was extracted from GMH’s electronic medical record system. Such case information includes whether the patient was outpatient or inpatient, whether the case was add-on or scheduled, the number of procedures in the case, etc. Case information was combined with the data collected from the ORTimer app using the unique case ID.
Our data did not include TOTs for cases that were not scheduled back-to-back. The “scheduled gap” between the two cases would increase the recorded value, so it would not reflect the true TOT. Therefore, we removed these cases from consideration.
Statistical analysis
For the hypothesis test, we introduced a new variable named turnover success. Turnover success is coded as: 1 (if actual TOT is less than or equal to the allotted TOT) and 0 (if actual TOT is greater than the allotted TOT). For the multiple regression analysis, the response variable considered was turnover excess, which is defined as the difference between the actual TOT and the allotted TOT (4). Turnover excess is used to measure the amount of delay during the TOT. Please note that turnover excess was set to zero if it was negative.
First, a two-sample proportionality test was employed to test the hypothesis that the use of the ORTimer app is effective in improving success rate of meeting established TOT benchmarks. We then estimated the Pearson intercorrelation matrix between the factors (i.e., delay reasons and surgical case information). Lastly, we performed multiple linear regression analysis to determine how the factors influenced turnover excess times. P values <0.05 were considered significant. All analyses were performed using the STATA statistical software version 12.0 (College Station, TX, USA).
Results
Hypothesis test
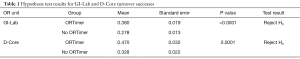
We collected data for 1,782 turnover observations from GI-Lab and 694 turnover observations from D-Core, respectively, during the data collection period at Greenville Memorial Hospital (GMH). For GI-Lab, we divided these 1,782 records into two groups based on whether the ORTimer app was used or not. The groups are “ORTimer” (640 records) and “No ORTimer” (1,142 records). A two-sample proportionality test was conducted to determine whether there is a statistical difference between turnover success in the “ORTimer” and “No ORTimer” groups (Table 1). The null hypothesis (H0) is that there is no difference between the two turnover groups and the alternative hypothesis (H1) is that the “ORTimer” turnover success is greater than that of “No ORTimer”. The proportionality test yields a P value of <0.0001. Thus, the null hypothesis can be rejected at the 95% confidence level. Similarly, for D-Core, we divided 694 turnover observations into two groups: “ORTimer” (236 records) and “No ORTimer” (458 records). It is clear that the null hypothesis can also be rejected at the 95% confidence level (P=0.0001). Therefore, we can conclude that the use of the ORTimer app was effective in improving OR performance at GMH.
Full table
Pearson correlation analysis
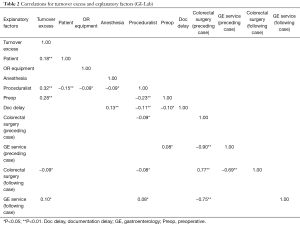
We performed the Pearson correlation analysis on the factors that pertain to the GI-Lab, as well as the D-Core. For the GI-Lab, patient, proceduralist, preoperative, colorectal surgery (following case), and gastroenterology service (following case) had statistically significant correlation with turnover excess (Table 2). These correlation values were found to be low to medium (ranging from 0.09 to 0.32). All of the delay reasons considered as factors had low correlations between them. Conversely, some of the case information had strong correlations with each other. For example, the correlation between colorectal surgery (preceding case) and gastroenterology services (preceding case) was −0.90 (P<0.01), and the correlation between gastroenterology services (preceding case) and colorectal surgery (following case) was −0.69 (P<0.01).
Full table
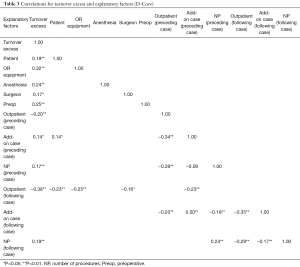
For the D-Core, all factors but add-on case (following case) had statistically significant correlation with turnover excess (Table 3). These correlation values were found to be low to medium (ranging from 0.17 to 0.38). Among the explanatory factors, the correlations were found to be low to medium. However, there is a strong correlation between add-on case (preceding case) and add-on case (following case): 0.50 (P<0.01).
Full table
Multiple regression analysis
After determining the correlation between the factors, those factors having lower correlation were analyzed together using multiple linear regression analysis. The results of the analysis for the GI-Lab data are presented in Table 4. Please note that we included only those factors in the model that were statistically significant at the 95% confidence level. The response variable, turnover excess, varied from 0 to 56.97 minutes with a mean of 6.67 minutes and standard deviation of 8.71 minutes. All of the explanatory factors were binary (0 or 1). About 58% of the variability in the turnover excess time was explained by the explanatory factors (R-squared =0.583).
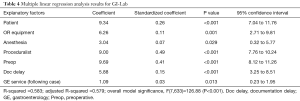
Full table
For the GI Lab, delays due to proceduralist-related issues were the dominant factor influencing turnover excess time (highest standardized regression coefficient). Holding all other factors fixed, delays due to patient-related issues contributed an estimated 9.3 minutes to turnover excess time. In other words, the following surgical case was pushed backed by estimated additional 9.3 minutes when OR TOT exceeds the allotted time threshold and there were patient-related issues. With a 95% confidence interval, this extra TOT was between 7.0 and 11.8 minutes. Similar explanation can be done for other factors since they are binary.
For the D-Core, the response variable, turnover excess, varied from 0 to 106.32 minutes with a mean of 11.82 minutes and standard deviation of 20.02 minutes. About 54% of the variability in the turnover excess was explained by the explanatory factors (R-squared =0.548, Table 5). Preoperative delay was the dominant factor influencing turnover excess time. It added about 28.8 minutes to the turnover excess while holding other factors fixed, i.e., the following case was pushed back by 28.8 minutes. With a 95% confidence interval, this time is between 20.2 and 37.4 minutes. Interestingly, having an outpatient as opposed to inpatient in the following case was found to reduce the turnover excess by about 5.4 minutes, holding all other factors fixed.
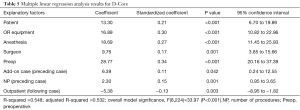
Full table
Discussion
There are many obstacles in implementing procedural changes to the TOT, patient preparation, and overall non-operative time phases. Due to fears of damaging relationships between clinicians, staff, and managers, some recommendations will not be adopted (2). In this research, we provide an alternative that requires minimal procedural change and minimal conflict among stakeholders.
This study examined the effectiveness of the ORTimer app in two different OR units at GMH. For both units, it was found that the ORTimer app can improve the turnover success, which in turn would improve OR efficiency. This can be attributed to the staff being more aware of time, things to be done, reasons for turnover delay, etc. However, additional research is required to identify the exact reason for this success.
In D-Core, the procedures performed were longer and more complex, so more time was allowed for the OR turnover, since the number of activities to be performed was higher than in the GI-Lab. However, the surgical cases in the GI-Lab were both simpler and shorter, so the turnover staff could learn faster from repetition. However, the D-Core had a higher turnover success rate than the GI-Lab. The shorter TOT target for the GI-Lab may contribute to the lower success rate, as there was less room for further time reductions. Given that the GI-Lab and D-Core have very different characteristics, the finding from this study suggests that the ORTimer app can be effective in different settings. Additional study sites will need to be assessed before this finding can be generalized.
When possible, the Android tablet that ran the app was connected to a monitor in the OR to increase visibility, but there were some rooms where this was not possible. Since many of the ORs already had large screens connected to computers which could run a web browser, we re-wrote the Android app as a web application so it could run in any room with a screen and a web-browser. This approach reduced the workload somewhat since the Android tablets did not have to be maintained in those rooms.
The plan is to deploy our web application in a server inside the hospital so it will be accessible by the computers within the hospital, but not from outside the hospital. Once we deploy it, we will be able to gather data from all the rooms by simply logging into the web application with a special administrative account. Moreover, the web application will be integrated with GMH’s electronic medical record system. Thus, once implemented, manual entries by staff will no longer be needed. In addition to this automation, this new functionality will allow us to explore other areas where we can improve communication and coordination within the group. Preoperative care, core coordinator, and charge nurse workload could be reduced by providing them with a single source where they can get all of their case timing information that is relevant to their area.
Conclusions
In this study, we created a mobile app named ORTimer to use in the OR to display the time left to complete the OR turnaround. The app serves as both a visual management tool as well as a TOT data collection tool. The visual component helps to focus the team on the team’s goal, and at the same time it facilitates data collection by making it clear when the goal was not met and requesting the team to provide reasons for the delays. By identifying barriers to the on-time completion of the turnaround, the app allows for continuous improvement of the turnover process. The results of this study showed that using the developed ORTimer app helped two different OR units of Greenville Memorial Hospital improve their success rate in meeting the established benchmarks set by perioperative management. It also identified the factors (i.e., delay reasons and surgical case information) that resulted in an extended TOT in an OR and quantified the amount of delay contributed by each those factors.
Acknowledgements
The authors would like to acknowledge the Perioperative Services Department at Greenville Health System for their continued leadership support of the research. In addition, the authors appreciate the time and energy spent by participating CRNA staff (D-Core) and nursing staff (Memorial Medical Office Building GI-Lab) during the research period.
Funding: Research reported in this manuscript was supported by the National Science Foundation under grant IIS-1237080. The authors are solely responsible for the content and views expressed in this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Weinbroum AA, Ekstein P, Ezri T. Efficiency of the operating room suite. Am J Surg 2003;185:244-50. [Crossref] [PubMed]
- Kodali BS, Kim D, Bleday R, et al. Successful strategies for the reduction of operating room turnover times in a tertiary care academic medical center. J Surg Res 2014;187:403-11. [Crossref] [PubMed]
- Porta CR, Foster A, Causey MW, et al. Operating room efficiency improvement after implementation of a postoperative team assessment. J Surg Res 2013;180:15-20. [Crossref] [PubMed]
- Uddin M, Allen R, Huynh N, et al. Effectiveness of a countdown timer in reducing OR turnover time. J Mob Technol Med 2017;6:25-33. [Crossref]
- Macario A, Dexter F, Traub RD. Hospital profitability per hour of operating room time can vary among surgeons. Anesth Analg 2001;93:669-75. [Crossref] [PubMed]
- Seim AR, Dahl DM, Sandberg WS. Small changes in operative time can yield discrete increases in operating room throughput. J Endourol 2007;21:703-8. [Crossref] [PubMed]
- Krupka DC, Sandberg WS. Operating room design and its impact on operating room economics. Curr Opin Anaesthesiol 2006;19:185-91. [Crossref] [PubMed]
- Collar RM, Shuman AG, Feiner S, et al. Lean management in academic surgery. J Am Coll Surg 2012;214:928-36. [Crossref] [PubMed]
- Warner CJ, Walsh DB, Horvath AJ, et al. Lean principles optimize on-time vascular surgery operating room starts and decrease resident work hours. J Vasc Surg 2013;58:1417-22. [Crossref] [PubMed]
- Free C, Phillips G, Watson L, et al. The effectiveness of mobile-health technologies to improve health care service delivery processes: a systematic review and meta-analysis. PLoS Med 2013;10:e1001363. [Crossref] [PubMed]
- Boulos MN, Wheeler S, Tavares C, et al. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online 2011;10:24. [Crossref] [PubMed]
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries? Global Health 2006;2:9. [Crossref] [PubMed]
- Martinez AW, Phillips ST, Carrilho E, et al. Simple telemedicine for developing regions: camera phones and paper-based microfluidic devices for real-time, off-site diagnosis. Anal Chem 2008;80:3699-707. [Crossref] [PubMed]
- Lane JS, Sandberg WS, Rothman B. Development and implementation of an integrated mobile situational awareness iPhone application VigiVU™ at an academic medical center. Int J Comput Assist Radiol Surg 2012;7:721-35. [Crossref] [PubMed]
- Uddin MM, Huynh N, Vidal JM, et al. Evaluation of Google’s voice recognition and sentence classification for health care applications. Eng Manag J 2015;27:152-62. [Crossref]
Cite this article as: Uddin M, Allen R, Huynh N, Vidal JM, Taaffe KM, Fredendall LD, Greenstein JS. Assessing operating room turnover time via the use of mobile application. mHealth 2018;4:12.


