User profile and preferences in fertility apps for preventing pregnancy: an exploratory pilot study
Introduction
Tracking health behaviors using mobile apps and devices offers timely, relevant data to help users gain self-knowledge for monitoring, and even changing, their behavior, with applications ranging from reminders about getting vaccinations to monitoring mental health status (1,2). Self-tracking for health is extremely popular: more than 70% of U.S. adults track or self-monitor a personal health indicator using a digital app (3). Market trends forecast the self-monitoring technologies market to exceed $18B in 2019, as evidenced by growing popularity for wearable technologies and self-monitoring apps (4).
Using tracking apps for menstrual and fertility monitoring is a progressive approach to tailored personal informatics. “Fertility apps” have gained momentum across all age groups and are the fourth most popular health monitoring apps among adults and the second most popular among adolescent girls (5). Fertility apps can assist women in preventing a pregnancy or conceiving. Many are marketed as digital extensions of fertility awareness-based methods (FABM), an evidence-based branch of contraception that relies on women identifying fertility through the interpretation of physiological signs and/or tracking of cycle lengths. Fertility apps on mobile phones provide information about women’s fertility status (whether they are likely to get pregnant if they have unprotected intercourse that day) and can help women keep track of menstrual cycles, estimate fertile days and ovulation, and integrate digital reminders or notifications for monitoring. Dozens of fertility apps are available and are typically branded as offering sophisticated data analytic approaches to predict key reproductive metrics with greater accuracy than traditional forms of self-tracking (6). However, a recent study found that only 30 currently existing apps purport to predict fertile days for a user, and of those apps only 6 were found to accurately identify the fertile window (7). The lack of accuracy is of particular importance to women using fertility apps to prevent a pregnancy, as the incorrect information provided around the fertile window can inform behavior that can lead to unintended pregnancy.
Very little is known about women using fertility apps specifically for pregnancy prevention. For example, it is unclear whether women use apps as a replacement for scientifically-validated FABM, in conjunction with other methods of birth control such as barrier methods, or simply to improve fertility self-knowledge. In addition to motivations for using fertility apps, gaps exist in our understanding about what garners trust in fertility apps for pregnancy prevention. Internet research studies have consistently identified trust as a key ingredient in whether an online resource may influence health-related behaviors (8-13). Users may trust apps’ ability to help them navigate health decisions if app design, including aesthetics (14) and functionality (15), is attractive to users, and if the app is reputable (16,17). Without understanding the characteristics and perceptions of this population, it is difficult to develop strategies to improve consumer behavior.
In this exploratory pilot study, we aim to identify women who currently use or intend to use a fertility app specifically to prevent pregnancy, and explore their preferences and perceptions about using apps for this purpose.
Methods
Recruitment
Women aged 18–39 were invited to participate in an online survey administered by Lab421 about their use and preferences using a fertility app. Users were eligible to participate if they were over the age of 18 and reported either having used an app to prevent pregnancy or their intention to use an app to prevent pregnancy in the future. Lab42 recruited women through Facebook between November 29 and December 8, 2016.
All participants verified their age and gave informed consent for participation in the study. Survey participants were incentivized with points, credits, or loyalty rewards for sites through which they took the survey. Data was downloaded from Facebook and stored in a secure database. Lab42 read all open-ended responses to ensure the respondent provided thoughtful and useful information. If a respondent did not pass their manual data quality inspection, Lab42 re-fielded and collected an additional sample.
Lab42 is a market research firm
Survey
We collected data about interest in and current use of fertility apps, as well as user intentions and goals for using fertility apps for pregnancy prevention. The survey included three questions to assess their level of basic knowledge about fertility and the reproductive cycle. Respondents were also asked to rate 6 app features that appeal to them in selecting an app to assist them in preventing pregnancy (attraction); rate specific app functions to assist users with pregnancy prevention (functionality), and rank which types of evidence were the most important to them personally in selecting an app to prevent pregnancy (reputation). See Table 1 for questions, scale, and item details. Women could also indicate if they had ever received some form of counseling from a provider on FABM. Responses about provider FABM counseling did not indicate parameters, depth, or quality of provider counseling.
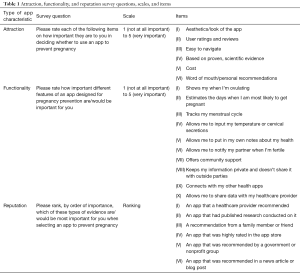
Full table
Most survey questions consisted of 5-point response scales. Due to few responses, those who selected “Not at all important” and “Low Importance” on importance questions were collapsed into a single category. For the survey question asking respondents to rank items by order of importance, rankings were grouped into top-ranked (rank 1 or 2), middle-ranked (rank 3 or 4), or low-ranked (rank 5 or 6).
Respondents also entered free-text examples of search terms they would use to search and find apps.
Fertility knowledge scales
Responses to survey knowledge questions about the menstrual cycle and fertility were assessed for accuracy. Survey items used were “What is considered the first day of a woman’s menstrual cycle?” and was considered correctly answered as “The first day of her period (bleeding);” “True or False: A woman can get pregnant at any time in her cycle,” correctly answered as “False;” and “What days in the menstrual cycle is a woman most likely to become pregnant?” correctly answered as “For a few days about halfway between two periods.” “Other” write-in responses to the third item were also coded for accuracy.
Respondents were grouped into two categories based on the proportion of knowledge questions they answered accurately: respondents with “moderate knowledge” answered any of the three knowledge items correctly; respondents with “limited knowledge” answered zero of the 3 correctly. Respondents who indicated they had received any form of counseling from a provider on FABM comprised a third group. We assessed this third self-reported provider-counseled group separately. Our hypothesis was that provider counseling on FABM would indicate the participant was more knowledgeable about fertility, and may be differently motivated than other fertility app users.
Statistical analysis
To examine the relationship between the provider-trained group and scoring on the knowledge items, chi-square tests were conducted to test for independence of the accuracy of responses to knowledge questions and whether a respondent had received training or counseling in FABM from a provider. Chi-square tests were then used to test for independence of the groupings and how users rated attraction and functionality and ranked types of evidence. The adjusted residuals were calculated to determine where the largest differences between observed and expected counts arose, while accounting for sample size of each of the three respondent groups. Statistical analyses were conducted in Stata v. 15 (StataCorp LLC; College Station, TX).
Qualitative analysis
Free-text search terms were extracted and collated for qualitative content analysis (18). Content analysis of app search terms is an emerging facet of analysis for web-based qualitative data, and is an appropriate approach to explore user intentions to find apps that match their preferences and desires (19). Using MaxQDA (v.2018), all search terms were assessed for content, frequency, and reading level. Differences in search terms according to user groupings were explored. Codes were constructed based on keywords and phrases that appeared most often within search terms. All data was coded and interpreted for content meanings.
Results
User statistics
One thousand (1,000) eligible female users completed the survey: 654 “moderate knowledge” users, 165 “limited knowledge” users, and 181 users who reported some form of provider counseling. Approximately 77% of respondents (n=769) indicated interest in using an app to prevent pregnancy in the future, while 23% (n=231) said they have used or currently use an app for this purpose. The majority of current app users reported that they had used Period Tracker (53.7%); other reported apps used included Fertility Calendar (26.0%), Fertility Friend (11.7%), Natural Cycles (11.3%), Ovia (7.4%), Ovuline (7.4%), Glow (6.9%), Dot (6.5%), Pink Pad Pro (6.5%), OvaGraph (6.1%), Kindara (5.2%), iCycleBeads (4.3%), Conceivable (3.9%), Clue (3.0%), 2DayMethod (3.0%) and unnamed others (9%).
About a quarter of current fertility app users reported they were “very confident” that the app they used would help them avoid pregnancy (23.8%); 46.3% were somewhat confident and another quarter (23.4%) were not sure. Among those who intended to use a fertility app in the future, nearly half (43.6%) were not sure if an app could help them successfully avoid pregnancy; one third (34.6%) were somewhat confident and 10.3% were very confident.
The age distribution of users with moderate knowledge was similar to the sample as a whole, while users with limited knowledge were slightly older. A higher percentage of women reporting provider training were between 18–24 years old (Table 2). The majority of survey respondents identified as Caucasian/White (74.1%), while 7.6% reported being Hispanic/Latino, 7.5% African American/Black, and 6.6% Asian. Of all respondents, 71.5% identified as either married, living with their significant other, engaged, or dating, while 25.4% reported being single. Table 2 summarizes our complete demographic results by user group.
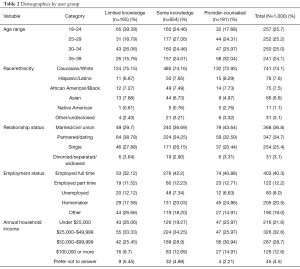
Full table
Of the 181 users who reported provider counseling, 80.1% had some knowledge of fertility awareness and 19.9% did not score any of the knowledge questions correctly. Overall, users who reported provider counseling on FABM were not more knowledgeable about fertility or basic reproductive health. Accuracy of the knowledge items in the survey was independent of whether a user reported having been personally counseled by a provider on FABM.
Fertility knowledge impacts on app selection and user preferences
Attraction
Users across all categories (63.4%) ranked an app being “based on proven scientific evidence” as “highly” important to them when choosing an app. A majority of users across all categories also placed “user ratings and reviews” (81.4%), “app cost” (80.4%), and “word of mouth/reputation” (68.4%) as either “Somewhat” or “Very important” to them when choosing an app. No differences were observed between users in different knowledge categories for these three aspects of app attraction.
Aesthetics of an app were less important to users with limited knowledge, but more important to provider-counseled users (P<0.001) compared to users with moderate knowledge. A greater proportion of users with limited fertility knowledge indicated that ease of use of an app was neither important nor unimportant to them in their app selection process, compared to other user groups (P<0.001). Table 3 provides full reporting on how user groups characterize aspects of attraction for selecting apps.
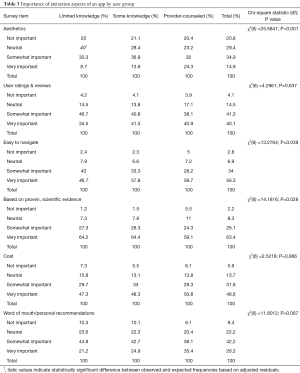
Full table
Functionality
Overall, women who reported some form of provider counseling on FABM were more likely to report app features/functions as very important compared to users with either moderate or limited knowledge for 7 out of 10 items. The three functionality aspects with no significant differences between groups were also reported as “Very Important” to a large proportion of respondents across categories, including: (I) an app that “show[s] me when I’m ovulating” (90.7%); (II) an app that “track[s] my menstrual cycle” (89.8%); and (III) an app that “keeps my information private and doesn’t share it with outside parties” (78.9%).
Users in all groups indicated that an app that “estimates days I’m most likely to get pregnant” was very important (72.6%), although a significantly greater proportion of provider-counseled users indicated that this function was very important compared to other groups (80.7%, P=0.006). Fertility apps that “allow me to notify my partner when I’m fertile” were not as important for users with moderate fertility knowledge compared to users who had received provider counseling (P=0.001). Apps that “offer community support” and “allow me to share data with my healthcare provider” were also not as important to moderately knowledgeable users when compared to provider-counseled and limited knowledge users (P=0.001 and P<0.001, respectively). Users reporting provider counseling placed differential importance on apps that “allow me to input my temperature or cervical secretions” (P=0.04) and “allow me to put in my own notes about my health” (P=0.035) compared to the other groups.
Table 4 further details user group preferences for fertility app functions.
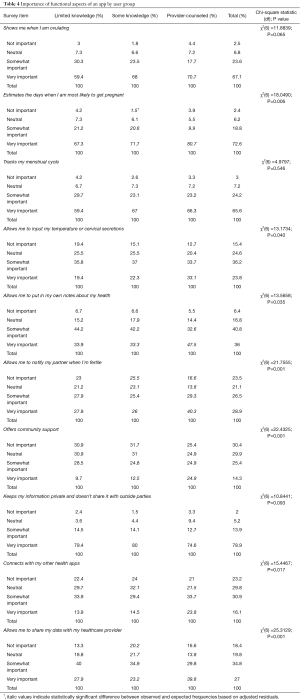
Full table
Reputation
Apps that “a healthcare provider recommended” were ranked “Very Important” for a large majority of users in both knowledge groups (70.0%), but were less important for selecting an app among users reporting provider counseling (P=0.006). Apps that “had published research conducted on it” was also highly important to many users; 54% of all users ranked it as “Very Important.” Users generally ranked apps that were “recommended in a news articles or blog post” and those “recommended by a government or nonprofit group” the lowest of the six reputational app influencers.
Table 5 summarizes how users ranked reputational aspects of apps.

Full table
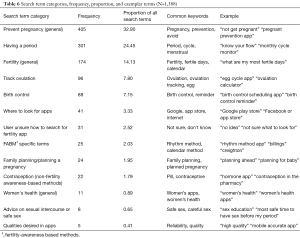
Search terms
A total of 1,388 discreet search terms were recorded. In aggregate, terms scored a 28.4 on the Flesch Reading Ease scale, representing a Grade 9.9 reading level. “Pregnancy” (14.72% of all words) and “tracker” (8.85%) were the two most common words used across all search terms. “Pregnancy prevention,” “period tracker,” “prevent pregnancy,” “birth control,” and “fertility tracker” were the five most common combined search terms.
The majority of search terms (71.5%) contained keywords or phrases indicating an interest in finding apps to help prevent pregnancy generally (n=405), apps that focus on the experience of menstruating or having a period (n=301), and apps focused on fertility generally (n=174). Terms indicating a desire to locate apps with the specific functionality to track ovulation (n=96) comprised 7.8% of all terms. Users also keyed terms indicating a desire to find apps focused on reminders to take birth control (7.2%); FABM specific methods (e.g., “billings”) (2.0%); planning a pregnancy (not preventing) (2.0%); non-FABM of contraception (e.g., “plan b,” “pill reminder app”) (1.8%); women’s health (0.9%); and advice on timing of sexual intercourse or safer sex (e.g., “safe times to have sex”) (0.7%). In addition, 41 terms included places on the Internet or search engines they would consult to find apps, and 31 terms indicated the user did not know what to search for to find an app. Differences in search term themes between user groups were not identified.
Table 6 details search term analysis and results.
Full table
Sensitivity analysis
Our sample included women who have used or currently use fertility apps to prevent pregnancy as well as women who were interested in doing so in the future. In our analysis, we combined these two response groups (n=1,000) in order to maximize available sample size and assess knowledge differences. However, we also conducted a sensitivity analysis to assess if there were differences between current users and women who are interested in using fertility apps, as it is probable that there are differences between people who are actively using an app versus those who are interested in doing so in the future. To test this, we ran the same statistical analysis restricted to current users only (n=231). Trends across knowledge groups when restricted to users were consistent with the results from the overall sample, although statistical power was too low to detect most statistical differences between knowledge groups.
Discussion
Our findings demonstrate an interest in and increasing demand for fertility apps that can be used to prevent pregnancy. In our recruitment process and in our final sample, the number of women who have used these apps to prevent pregnancy is small, compared to the number who indicate that they intend to do so in the near future, suggesting that future interventions aimed at educating women around appropriate fertility apps are needed, in order to help growing numbers of women prevent unintended pregnancy.
In short, users wishing to prevent pregnancy with a digital tracking tool want the app to be science- and research-backed, have sophisticated features like predicting ovulation and menses, while maintaining assurances of privacy. Not surprisingly, women’s clear preferences for evidence, assurances and medical accuracy are consistent with documented antecedents of online trust in apps (20). Fertility app users seem to correlate scientific evidence used in the development and marketing of an app with the likelihood of intended results, similar to how other forms of birth control are viewed. Yet, despite this noted preference, few of the fertility apps that users reported actually using were intended to help a woman prevent pregnancy. It is possible that app developers who use scientific jargon to promote their apps are perceived as being “scientifically-based” in a similar manner to the way that the use of “scientific” terminology has been used to improve consumer confidence in beauty products (21). Further research is needed in this area to understand how women determine if an app is based on scientific evidence, and how credibility assurances are communicated to women selecting apps.
Surprisingly, users who reported some form of provider counseling were not more knowledgeable about basic fertility than other women in the sample, disproving our hypothesis. Some women believe they have been counseled by a provider on FABM when in fact there may not be a common base of understanding among app users about what constitutes a FABM or what is simply fertility awareness, or period or ovulation monitoring. Provider willingness to discuss FABMs is generally very low, and most FABM take months to appropriately train (for example, symptothermal method requires a trained person teaching a woman how to chart menses and helping her interpret charts over the course of several months). When searching for a fertility app to help prevent pregnancy, a sizable user portion (about one fifth) looked for apps using terms unrelated to pregnancy prevention, having a period, or ovulation—some terms even pointed to a desire to use an app to remind them to take birth control pills. These findings underscore a general unreliable base of knowledge among women about what FABM are and what they are not. It is important for comprehensive sexuality education programs to include FABM and showcase the breadth of science behind these methods for fertility planning.
One of the most striking observations we note is that most fertility apps women reported that they have used were not designed as a digital FABM platform to facilitate the recording of fertility signs and deliver interpretative capability. This poses a highly problematic disconnect between the capacities of apps for pregnancy prevention and the clearly stated preferences among women for features and design based on scientific evidence. It is likely that there is a preference for monitoring apps about health to be based in science globally, but this is an understudied area. Given the consumer demand we observe in this study for fertility apps used specifically for pregnancy prevention, much more research is needed in this unique consumer space to understand how women can be informed consumers.
Our study has several limitations. Our strategy to sample fertility app current and interested users exclusively from a social networking platform and the self-reported nature of the online survey limit how generalizable our findings will be for a broader population. There is diversity among fertility app users, particularly outside of the U.S. context, that is not represented in our study. Our survey and knowledge questions are not validated items. We also acknowledge our small sample size for actual fertility app users compared to intended users, which may contain more meaningful differences that we were able to explore in this study.
Conclusions
Despite limitations, this is the first study of its kind to look at women who specifically wish to use fertility apps to prevent pregnancy. Perhaps most importantly, our study speaks to a growing trend among women to use apps to prevent pregnancy. It is critical that app developers, researchers, and women’s health advocates collaborate to develop apps with the preferred functionality women desire. Equally critical is for developers to clearly delineate limitations of apps, and the extent to which an app should be marketed as having the capacity to help prevent pregnancy. While it is beyond the scope of this study to examine the accuracy or efficacy of fertility apps for pregnancy prevention, our study points to women’s confidence and trust in apps for this purpose already. Research is needed to not only investigate accuracy and efficacy for fertility apps for pregnancy prevention, but also so we may build accountability structures and transparency for the app marketplace. The development of a validated fertility knowledge instrument would also be useful in advancing this research. Informed consumer campaigns have a role to play in marketing apps to women that do have the capacity to act as digital platforms for proven FABM and have research to support their efficacy (22-24). For women who want to use these tools to prevent pregnancy, consumer education and behavior change communications to bolster informed health decision-making, including educating about app credentials and selection criteria, will also improve informed utilization.
Acknowledgements
The authors would like to thank Drs. Victoria Jennings and Dominick Shattuck at the Institute for Reproductive Health at Georgetown University for their substantive contributions in the scope, design, and execution of this pilot study.
Funding: This study was supported by the United States Agency for International Development grant (No. AID-OAAOAO13O00083) under the FACT Project.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: The objective of this pilot study was to understand fertility app preference from aggregate data. Identifiable information was not collected, the sample size is not reflective of the general population and thus limits generalization, and due to these factors IRB approval was not sought out. All participants in this study confirmed they were over the age of 18 and gave informed consent to participate in the study.
1Lab42 is a market research firm.
References
- Paradis M, Atkinson KM, Hui C, et al. Immunization and technology among newcomers: A needs assessment survey for a vaccine-tracking app. Hum Vaccin Immunother 2018.1-5. [Crossref] [PubMed]
- Rathbone AL, Prescott J. The Use of Mobile Apps and SMS Messaging as Physical and Mental Health Interventions: Systematic Review. J Med Internet Res 2017;19. [Crossref] [PubMed]
- Fox S, Duggan M. Tracking for Health. Pew Research Center, 2013. Available online: http://www.pewinternet.org/2013/01/28/tracking-for-health
- Mobile devices driving unprecedented growth in self-monitoring technologies markets, according to bcc research [press release]. BCC Research LLC, June 29 2015. Available online: https://www.bccresearch.com/pressroom/hlc/mobile-devices-driving-unprecedented-growth-in-self-monitoring-technologies-markets
- Moglia ML, Nguyen HV, Chyjek K, et al. Evaluation of Smartphone Menstrual Cycle Tracking Applications Using an Adapted APPLICATIONS Scoring System. Obstet Gynecol 2016;127:1153-60. [Crossref] [PubMed]
- Sohda S, Suzuki K, Igari I. Relationship Between the Menstrual Cycle and Timing of Ovulation Revealed by New Protocols: Analysis of Data from a Self-Tracking Health App. J Med Internet Res 2017;19. [Crossref] [PubMed]
- Duane M, Contreras A, Jensen ET, et al. The Performance of Fertility Awareness-based Method Apps Marketed to Avoid Pregnancy. J Am Board Fam Med 2016;29:508-11. [Crossref] [PubMed]
- Sillence E, Briggs P, Harris P, et al. Health Websites that people can trust - the case of hypertension. Interacting with Computers 2007;19:32-42. [Crossref]
- Sillence E, Briggs P, Peter H, et al. A framework for understanding trust factors in web-based health advice. International Journal of Human-Computer Studies 2006;64:697-713. [Crossref]
- Cheshire C. Online Trust, Trustworthiness, or Assurance? Daedalus 2011;140:49-58. [Crossref] [PubMed]
- Fogg BJ, Marshall J, Laraki O, et al. What makes web sites credible? A report on a large quantitative study. In: Beaudouin-Lafon M, Jacob RJK. editors. ACM CHI 2001 Human Factors in Computing Systems Conference; March 31-April 5, 2001; Seattle, Washington, USA, 2001:61-8.
- Friedman B, Kahn PH, Howe DC. Trust online. Commun Acm 2000;43:34-40. [Crossref]
- Briggs P, Burford B, De Angeli A, et al. Trust in online advice. Social Science Computer Review 2002;20:321-32. [Crossref]
- Sillence E, Briggs P, Fishwick L, et al. Trust and mistrust of online health sites. In: Dykstra-Erickson E, Tscheligi M. editors. ACM CHI 2004 Conference on Human Factors in Computing Systems; April 24-29, 2004; Vienna, Austria, 2004:663-70.
- Taraborelli D. How the web is changing the way we trust. In: Waelbers K, Briggle A, Brey P. editors. Current Issues in Computing and Philosophy. Amsterdam, The Netherlands: IOS Press, 2008:194-204.
- Josang A, Ismail R, Boyd C. A survey of trust and reputation systems for online service provision. Decision Support Systems 2007;43:618-44. [Crossref]
- Yi MY, Yoon JJ, Davis JM, et al. Untangling the antecedents of initial trust in Web-based health information: The roles of argument quality, source expertise, and user perceptions of information quality and risk. Decision Support Systems 2013;55:284-95. [Crossref]
- Krippendorff K. Content Analysis: An Introduction to its Methodology. Third ed. Thousand Oaks, CA: Sage Publications, 2013.
- Krippendorff K, Bock MA. The content analysis reader. Thousand Oaks, CA: Sage Publications, 2009.
- Beldad A, de Jong M, Steehouder M. How shall I trust the faceless and the intangible? A literature review on the antecedents of online trust. Computers in Human Behavior 2010;26:857-69. [Crossref]
- Arroyo MD. Scientific Language in Skin-Care Advertising: Persuading through Opacity. Revista Espanola De Linguistica Aplicada 2013;26:197-213.
- Shelus V, Ashcroft N, Burgess S, et al. Preventing Pregnancy in Kenya Through Distribution and Use of the CycleBeads Mobile Application. Int Perspect Sex Reprod Health 2017;43:131-41. [Crossref] [PubMed]
- Li D, Heyer L, Jennings VH, et al. Personalised estimation of a woman's most fertile days. Eur J Contracept Reprod Health Care 2016;21:323-8. [Crossref] [PubMed]
- Simmons RG, Shattuck DC, Jennings VH. Assessing the Efficacy of an App-Based Method of Family Planning: The Dot Study Protocol. JMIR Res Protoc 2017;6. [Crossref] [PubMed]
Cite this article as: Starling MS, Kandel Z, Haile L, Simmons RG. User profile and preferences in fertility apps for preventing pregnancy: an exploratory pilot study. mHealth 2018;4:21.


