Evaluation of a digital health resource providing physiotherapy information for postnatal women in a tertiary public hospital in Australia
Introduction
Globally, countries with developed health care services are facing sustained pressure to meet the competing demands of increasing quality of care, while also improving efficiency and reducing expenditure, essentially ‘to do more and better for less’ (1). A key measure of a health care organisations ability to meet these demands is monitoring the average length of inpatient stay (LOS) in relation to the national average indicated for any given condition/hospitalisation category (2).
At our institution, the Women’s and Children’s Hospital (WCH; Adelaide, South Australia), the Physiotherapy Department endeavours to provide an individual consult to all postnatal women who have elected to birth at the centre, as well as those who have been transferred for their postnatal care. This consultation allows for early screening of significant pain, mobility issues and voiding dysfunction, and provides the opportunity for timely advice regarding perineal/wound care, as well as education on pelvic floor muscle function and rehabilitation. In addition to this, women can be referred to physiotherapy for specific complaints such as musculoskeletal discomfort and symptoms of pelvic floor dysfunction. Women are provided with two comprehensive handouts which supplement the consultation.
Historically, further postnatal education regarding abdominal muscle structure, function and recovery, back care and postural advice, and returning to exercise and activities of daily living was presented in a ward-based class format of approximately 30 minutes duration. Attendance at this class was voluntary and women who were not appropriate for class attendance (e.g., women from non-English speaking backgrounds, those with learning difficulties and those of young maternal age) were offered an extension of the individual consultation so that the class content was incorporated into their education session. The ward-based postnatal education classes presented several benefits for the women: additional education on relevant topics, opportunity for further input and tailored advice from physiotherapy staff during their inpatient admission and a group environment with the chance to interact and share experiences with other newly postnatal women.
In recent years, increasing pressure on the public health system to reduce LOS has resulted in the implementation of a number of initiatives at our institution to facilitate early discharge from the postnatal ward. These changes coincided with a persistent reduction in attendance at the ward-based physiotherapy-led postnatal education class despite numerous initiatives to boost attendance.
Reducing attendance at ward based postnatal education sessions prompted physiotherapy staff to investigate further, and in 2012, a consumer-focussed project was completed with the assistance of health promotion physiotherapy students from the University of South Australia (UniSA). The project investigated the real and perceived barriers to class attendance, seeking alternative suggestions to class format and location, and evaluating the perceived usefulness of the class for attendees (3). The results of this project demonstrated that the majority of women who attended the class found it extremely useful but that many women were unable to attend due to the number of competing priorities during their short inpatient stay. During the survey, women expressed a desire for the information to be presented in an alternate format, with the most popular method being via the internet followed by DVD/video (3). To the best of our knowledge, there was no other resource to meet our needs available nationally or described in the literature at the time of project development.
In 2014 a grant application was submitted and supported by the Queen Victoria Auxiliary (WCH) which secured funding for the development of a digital version of the postnatal education class. In 2015 a second project was completed with the help of health promotion physiotherapy students from UniSA to assist in script development (4). Filming and editing commenced in 2015 and was completed in 2016 with the launch of the digital resource occurring in May of that year. This paper outlines the process for evaluating the Digital Health Resource, the first of its kind produced by the Physiotherapy Department at the WCH.
Methods
Approval for this quality assurance project was granted by the WCHN Human Research Ethics Committee in March 2017 (Audit 903A/March/2017) and was also supported by the University of South Australia Human Research Ethics Committee. Two final year physiotherapy students were again recruited from UniSA to assist in the evaluation of the digital postnatal physiotherapy resource.
Women admitted to the Postnatal Ward at the WCH were invited to participate in a survey to be undertaken at approximately 2 weeks postnatal during their individual postnatal consult with the physiotherapist (Supplementary file). Physiotherapy staff provided patients with a participation information sheet outlining the purpose of the study and its voluntary and anonymous nature. Patients were asked to sign the consent form if they were willing to participate and to choose their preferred method of completion, as the survey was available in online and hardcopy formats. If the postnatal woman preferred an online survey, an email address was collected at the time of consent. Women were advised they could access the resource while an inpatient or at home, and they could use either the QR code in the written handout or follow the documented instructions to the webpage with the video embedded to view it.
Postnatal women were consented by physiotherapy staff during a 17-day recruitment period (March 28th–April 13th). To determine the percentage of women birthing at WCH who would be represented by the survey responses, data was obtained from the WCH Health Informatics, Performance, Planning and Outcome (HIPPO) unit which showed that 213 women birthed at WCH during the recruitment period. Women who discharged direct from the delivery suite and those admitted to the antenatal ward after their births were not included in the project. Women from non-English speaking backgrounds were also excluded from the project. Online surveys were emailed to women at approximately 2 weeks postnatal and a thematic analysis of the responses was completed.
Results
A total of 88 women agreed to take part in the project representing 41% of the postnatal population during the recruitment period, all women chose to complete the online version of the survey using Survey Monkey™. Of the 88 women who provided their consent and email address, 65 opened the email invitation (74%), 29 clicked through to the survey page (33%) and 27 commenced the survey (31%). Not all 27 participants answered each question as there was opportunity to ‘skip’ questions throughout the survey.
Viewing habits
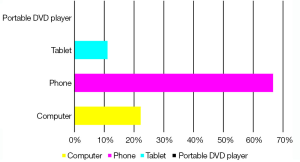
Nine of the 27 respondents watched the digital video clip ‘physiotherapy advice to help you recover from pregnancy and birth’ (six watched ‘all of it’ and three ‘only some of it’). Of the nine who watched at least some of the video clip, none had watched it on the day of delivery, one watched it within 1–3 days, two women had watched by 1 week and the remaining six watched the clip by the second postnatal week. The majority of women watched the video once (8/9), with one respondent watching the video more than twice. None of the women had watched the digital resource while in hospital (either via website or ward DVD), all watched it while at home and the most common technology used to view the video was phone (6/9) followed by computer (2/9) and one person watching it on a tablet (Figure 1).
Format and content appraisal
In regards to the length of the video, the majority of women felt it was ‘just right’ (6/9), three felt it was ‘too long’ but none felt it was ‘too short’. Most women watched the video because they wanted to learn more about how to help their body recover after giving birth (n=8), other reasons listed (multiple reasons allowed) included fitness and health being very important to them (n=3), the physiotherapist/midwife/doctor reminded me (n=3), my friend told me about it (n=0) and I was worried about recovery after pregnancy and birth (n=3).
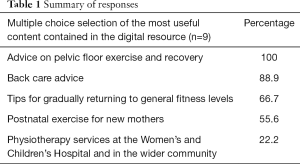
The same nine women provided information on what they found most useful from the video clip (multiple options could be selected) (Table 1).
Full table
All of the women knew about the digital resource from their visit with the physiotherapist at the hospital and two also noted that they read about it in their handout.
Barriers to viewing
Though only three women reported they watched only some of the clip, six women provided further information in response to the question directed to this particular group as to why they stopped. Answers were as follows: I was too busy (n=3), I had other things that required my attention (n=2), I watched the entire video (n=2), I already knew the information (n=1), I felt unwell/tired (n=1). One woman chose to complete the free-text option and commented that her newborn baby was not sleeping throughout the day and this was impacting on her time to watch the video. No women chose the following responses: I didn’t find it helpful, the visit from the Physiotherapist in hospital covered everything, I lost interest, the video was too long. No women answered that they were not intending to finish the video if they had only watched some of it.
Eighteen women initially reported having not watched the video and 18 women responded to the question relating to why this was the case. Answers are listed in terms of popularity; I was too busy (n=7), I forgot (n=6), I already watched the entire video (n=5), I have already had a baby and knew the information (n=4), I felt that the paper handout and physiotherapy consultation was enough (n=4), I didn’t have the technology to access it (n=2). No women selected: I felt unwell/tired, I was overwhelmed by the information, I plan on doing so soon. Eight women provided free-text responses, one relating to feeding issues with the baby which impacted on time available to watch the video, all other responses were from women reporting they were either unaware of the video or had been expecting to receive this as a link with the email.
Discussion
The results of the survey allowed us to evaluate the digital health resource, created in response to consumer feedback and as a method to ensure postnatal women had access to important physiotherapy information, despite the changing health care landscape.
It is now well established that pregnancy and childbirth has a profound and lasting effect on the female body and is associated with a number of conditions including urinary and faecal incontinence, pelvic organ prolapse and lumbo-pelvic pain (5,6). These conditions can have a significant impact on quality of life but can also be prevented, managed, improved and/or cured with conservative management provided by a physiotherapist (7-9). In Australia, almost all deliveries occur in the hospital setting making this an ideal time to capture women for early education regarding postnatal recovery and the services available to them after discharge, supported by the fact that all survey respondents reported knowing about the digital health resource because the physiotherapist had taken the opportunity to raise this with them while they were an inpatient (10).
Only nine of the 27 survey respondents had watched the digital video clip ‘physiotherapy advice to help you recover from pregnancy and birth’ but information on the viewing habits could still be ascertained from the responses. Six of these women had watched the entire video and three had only viewed part of it, though the responses indicated these women did intend to watch the remainder of the video at a later date. Splitting the video into sections with a direct link to each individual topic may make it easier for women who are watching the video over a number of sessions to click straight through to the relevant information. This would also allow the few women who indicated it was ‘too long’ to prioritise the content they watched. It was interesting to note that most women watched the video between postnatal week 1 and 2, and the majority (6/9) watched the video on their phone. The survey was sent to women at approximately 2 weeks postnatal, this may have prompted some women to watch the video that had forgotten or were not intending to view the resource at all, presenting a potential bias in the results. No women accessed the video on the portable DVD player available on the postnatal ward. This may be due to a lack of awareness of the option, though the majority of the population now have access to internet via mobile and other devices and still did not watch the video in the early 1–2 days post birth, this is more likely related to timing and/or poor promotion of this option by postnatal ward staff, rather than lack of access to technology (11). However, it should still be noted that two women in the survey did comment that they did not have the technology to access the video, raising a need for alternate viewing options to be provided during the inpatient stay.
Women listed themes of recovery, health and fitness as motivators for watching the video and it is encouraging to see that all women found the advice on pelvic floor exercise and recovery most useful on reflection, along with other information considered important for long term recovery in the postnatal period such as back care and general fitness. Clark et al. in 2009 explored women’s experiences of their body in pregnancy and postpartum and found that while women responded positively to the changes in their body during pregnancy, this was not maintained in the postpartum period, where women reported increased levels of dissatisfaction with their body image (12). Much of the literature focuses on women’s concerns in relation to the infant, breastfeeding and mental health during the postpartum period, with little research into maternal views of their own recovery, body image and experiences. These responses represent only 10% of the postnatal women recruited to the project and 33% of respondents, and are therefore subject to a degree of non-response bias. The influence of non-responders on survey outcomes is debatable, while some literature has suggested under-representation of minorities and those of low socioeconomic and education backgrounds, other studies have demonstrated only a weak relationship exists with response rate and non-response bias, with respondents to health-related surveys more likely to participate in a healthier lifestyle than non-respondents, but only by a much smaller rate than expected (0.97% prevalence) (13,14).
The most common reasons for not watching the video were not surprising, with the most frequently cited barrier being lack of time. Some of these women had already watched the video or forgotten about the video, some reported knowing the information already and others felt the paper handout and physiotherapy consultation was enough on its own. While there is certainly some repetition of information between the individual consultation, paper handout and digital resources available at our institution, the video does expand on back care, fitness and general exercise advice further. More effort to communicate this difference should be considered. It is also worth noting that providing information in multiple formats allows us to cater to various learning styles with evidence suggesting that customising educational materials to the consumer’s health literacy level and their preferred learning style (whether that be visual, auditory or kinaesthetic) improves the individual’s retention of health information (15). Unfortunately, a number of women (7/18) reported being unaware of the video despite being consented to the project in person, and supplied with written information containing a link to view this. Women are commonly overwhelmed with information in the immediate days postpartum and there may be merit in considering a way to communicate or remind women of the video link at another time-point in the postpartum period.
All of those who did watch the video reported finding out about it from their consult with the physiotherapist, highlighting this as an important visit during their short postnatal ward stay. With the increasing pressure of early discharge there is less time for women to gain important information on common postnatal tasks and aspects of their own recovery, this finding is a positive reflection on the role of the physiotherapy visit during their postnatal inpatient stay. A local clinical audit was conducted to determine how many women had physiotherapy contact following the birth of their baby. Over a 3-month period, there were 1,108 confinements and 91% of these (n=1,008) had at least one episode of physiotherapy contact. Of the 100 women who did not have physiotherapy contact, 67 of these discharged early, direct from delivery suite, often within 4 hours of the birth of their baby.
While the women listed common barriers that encroach on postpartum women’s time such as being too busy or having other competing priorities, it was positive to see that no women reported the length of the video or their level of interest as barriers to completion. It is quite possible that the women, who consented to the study but did not click-through to complete the survey, did so because they had not read or watched the resources being investigated. It is reassuring to know that all of these women have access to an individual consultation with the physiotherapist, and are therefore aware that the physiotherapy team play a role in postnatal recovery.
While conclusions can be drawn regarding the satisfaction of a small group of women birthing at our institution during the study period, women who did not speak English were excluded from the survey owing to the absence of funding for translation of the survey into multiple languages. While a significant proportion of women accessing care at WCH are considered to be of culturally and linguistically diverse (CALD) background, information on the number of women requiring an interpreter during their health care is limited in its accuracy; some women who need interpreter services on the postnatal ward may have used their family members to translate consults and are therefore not recorded, and statistics tend to be available across the whole year rather than specific time points in the antenatal or postnatal period such as inpatient admissions. In 2015, Clinical Information Services data showed that 368 women used an interpreter at least once which represented 13% of the 4,714 births in that year; the most common languages required for postnatal women were Mandarin, Dari, Vietnamese, Persian and Arabic. Translating the digital resource into key languages would allow these women the benefit of accessing information about postnatal recovery at home in their own time, an advantage of which only English-speaking women benefit from at present.
The WCH specific written and digital postnatal physiotherapy resources are only available in the English language. In an attempt to minimise the known disadvantage and inferior health outcomes experienced by women of CALD backgrounds, those who do not speak or have limited proficiency in English, are offered an extension of their individual consult to allow the content of the digital and written resources to be covered in person via an interpreter, in line with best practice guidelines (16). This improves access to the information; however, from the survey results we know that some women choose to access this information a number of times after discharge or prefer to expose themselves to this education over a number of separate sessions. This seems an appropriate way to synthesise the information given the days immediately postpartum are filled with visits from multiple health care professionals, all providing important information relevant to their disciplines. In addition to the amount of information, the time taken to absorb this has been condensed into shorter timeframes with the introduction of early discharge initiatives and reduced LOS. The advantages of providing written advice to supplement verbal health education has been well documented in the literature, and while attempts are made to provide written postnatal information available from other health services to women where possible, this cohort at WCH continue to be disadvantaged by their lack of English proficiency in many respects (17). The value of translating the digital resource with voiceover (rather than subtitles to overcome literacy barriers) in key languages spoken by the women birthing at our hospital should be considered. This would provide an opportunity to compare digital media access between the CALD and non-CALD populations and also determine the cultural competency of the digital content. The implementation of this would be an important step towards reducing the gap and inequalities experienced by CALD populations in the health care system.
There were a number of limitations encountered with the project design and methods used. Collecting patient consent and email address in written form meant the interpretation of contact details was difficult at times and may have resulted in some women not receiving the follow up survey at all. Women consented to receiving the survey initially via email but had not consented to any further follow-up. Reminder emails to complete the survey and/or watch the video may have resulted in a higher response rate, less potential bias and better generalisability of our findings. The survey design itself allowed for imprecision in response groups. Women were not prevented from answering any of the proposed questions, and many women appear to have answered questions directed at different response groups (i.e., those who watched all of the digital resource could also answer questions directed to women who had watched none of it) which reduced the value of those answers. Women who discharged directly from delivery suite (usually within 4 hours of birth) were excluded from the study as consent to the project was unable to be obtained. It would have been useful to learn the viewing habits of this group, who typically have low-intervention labours and births (enabling them to qualify for early discharge) and whether they were more or less motivated to engage in the physiotherapy digital resource available to them.
Conclusions
This quality assurance project has demonstrated that the digital health resource provides useful information on postnatal recovery to women birthing at a tertiary public hospital with early discharge initiatives in place. It appears to provide a flexible platform to access physiotherapy education after discharge from hospital, though it appears to be under-utilised. Efforts should be made to improve its format so that women can more easily prioritise which content they view and when, to overcome commonly cited barriers such as lack of time. Additionally, further consideration of strategies to remind women of the resource available to them beyond the first few weeks postpartum is warranted. Finally, access to the digital health resource on discharge should be available to all women, including those of non-English speaking backgrounds, thus translation of supplementary written information and voiceover of the digital resource should be strongly considered by the institution.
Survey questions
1) Did you watch the digital video clip ‘physiotherapy advice—to help you recover from pregnancy and birth’?
a) Yes
b) Only some of it
c) No (skip to Question 12)
2) How soon after the birth of your baby did you watch the digital video clip?
a) Immediately
b) 1–3 days
c) 1 week
d) 2 weeks
3) How many times did you watch the digital video clip?
a) Once
b) Twice
c) More than twice
4) Where did you watch the digital video clip?
a) In hospital
b) At home
c) Other
5) How did you watch the digital video clip?
a) Computer
b) Phone
c) Tablet
d) Portable DVD player (available on ward)
e) Other
6) The length of the digital video clip was:
a) Too long
b) Too short
c) Just right
7) Please tick one or more reasons why you watched the digital video clip?
a) I wanted to learn about how to help my body recover after giving birth
b) Fitness and health are very important to me
c) My physiotherapist/midwife/doctor reminded me
d) My friend told me about it
e) I was worried about recovery after pregnancy and birth
f) Other
8) What did you find useful from the digital video clip? (Select as many options as needed)
a) Advice on pelvic floor exercise and recovery
b) Postnatal exercises for new mothers
c) Back care advice
d) Tips for gradually returning to general fitness levels
e) Physiotherapy services at the Women’s and Children’s Hospital and in the wider community
9) How did you find out about the digital video clip?
a) The physiotherapists at the WCH told me about it
b) I read about it in my physiotherapy handout
c) I saw the poster in my hospital room
d) Medical staff (midwives, doctor) at the WCH told me about it
e) Friends and family
f) When searching online
g) Other
10) If you answered ‘only some of it’ to Question 1, please give one or more reasons why you stopped:
a) I felt unwell/tired
b) I didn’t find it helpful
c) The visit from the physiotherapist in hospital covered everything
d) I already knew the information
e) I lost interest
f) I was too busy
g) The video was too long
h) I had other things that required my attention
i) Other
11) Do you intend to watch the rest of the video at some stage?
a) Yes
b) No
12) If you answered ‘No’ to Question 1, please circle as many as apply.
a) I felt unwell/tired
b) I was too busy
c) I was overwhelmed by the information
d) I have already had a baby and knew the information
e) I felt that the paper handout and physiotherapy consultation was enough
f) I forgot
g) I plan on doing so soon
h) I didn’t have the technology to access it
i) Other
Acknowledgements
The author wishes to acknowledge the Women’s Physiotherapy Department, Queen Victoria Auxiliary and Digital Media team at the Women’s and Children’s Hospital and the School of Physiotherapy at the University of South Australia for their support in the development of the digital resource. The author also wishes to acknowledge the support of Tara Beaumont, Head of Unit, Women’s Health Physiotherapy for providing guidance and support during the project.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
Ethical Statement: Approval for this quality assurance project was granted by the WCHN Human Research Ethics Committee in March 2017 (Audit 903A/March/2017) and was also supported by the University of South Australia Human Research Ethics Committee. Written informed consent was obtained from all patients.
References
- Bowers J, Cheyne H. Reducing the length of postnatal hospital stay: implications for cost and quality of care. BMC Health Serv Res 2016;16:16. [Crossref] [PubMed]
- Admitted patient care 2015-16. Australian hospital statistics. Australian Institute of Health and Welfare, 2017. Available online: https://www.aihw.gov.au/getmedia/3e1d7d7e-26d9-44fb-8549-aa30ccff100a/20742.pdf.aspx?inline=true
- Gray R, Colsey. Improving postnatal physiotherapy class attendance. Health Promotion - REHB 4035 Project. Adelaide: University of South Australia, 2012.
- Gray A, Jackson N. Script development for implementation in a health promotion video for postnatal women. Health Promotion - REHB 4035 Project. Adelaide: University of South Australia, 2015.
- Woodley SJ, Boyle R, Cody JD, et al. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 2017;12. [PubMed]
- Hallock JL, Handa VL. The Epidemiology of Pelvic Floor Disorders and Childbirth: An Update. Obstet Gynecol Clin North Am 2016;43:1-13. [Crossref] [PubMed]
- Moore K, Dumoulin C, Bradley C, et al. Committee 12: Adult conservative management. In: Abrams P, Cardozo L, Khoury S, et al. (eds). Incontinence: 5th International Consultation on Incontinence. Plymbridge, UK: Health Publication Ltd, 2013;1101-227.
- Bliss DZ, Mellgren A, Chiarioni G et al. Committee 16: Assessment and conservative management of faecal incontinence. In: Abrams P, Cardozo L, Khoury S, et al. (eds). Incontinence: 5th International Plymbridge, UK: Health Publication Ltd, 2013;1443-79.
- Vleeming A, Albert HB, Ostgaard HC, et al. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 2008;17:794-819. [Crossref] [PubMed]
- Australia’s mothers and babies 2015; in brief. Australian Institute of Health and Welfare, 2017. Available online: https://www.aihw.gov.au/getmedia/728e7dc2-ced6-47b7-addd-befc9d95af2d/aihw-per-91-inbrief.pdf.aspx?inline=true
- Using technology in service delivery to families, children and young people. Australian Institute of Family Studies, 2013. Available online: https://aifs.gov.au/cfca/publications/using-technology-service-delivery-families-children/technology-use-australia
- Clark A, Skouteris H, Wertheim EH, et al. My baby body: A qualitative insight into women’s body‐related experiences and mood during pregnancy and the postpartum. J Reprod Infant Psychol 2009;27:330-45. [Crossref]
- McLeod TG, Costello BA, Colligan RC, et al. Personality characteristics of health care satisfaction survey non-respondents. Int J Health Care Qual Assur 2009;22:145-56. [Crossref] [PubMed]
- Klesges RC, Williamson JE, Somes GW, et al. A population comparison of participants and nonparticipants in a health survey. Am J Public Health 1999;89:1228-31. [Crossref] [PubMed]
- Giuse NB, Koonce TY, Storrow AB, et al. Using health literacy and learning style preferences to optimize the delivery of health information. J Health Commun 2012;17 Suppl 3:122-40. [Crossref] [PubMed]
- Gray B, Hilder J, Donaldson H. Why do we not use trained interpreters for all patients with limited English proficiency? Is there a place for using family members? Aust J Prim Health 2011;17:240-9. [Crossref] [PubMed]
- Johnson A, Sandford J, Tyndall J. Written and verbal information versus verbal information only for patients being discharged from acute hospital settings to home. Cochrane Database Syst Rev 2003. [PubMed]
Cite this article as: Goode K. Evaluation of a digital health resource providing physiotherapy information for postnatal women in a tertiary public hospital in Australia. mHealth 2018;4:42.