Perceptions on mobile health in the primary healthcare setting in Belgium
Introduction
Mobile health or mHealth refers to the use of electronic tools to deliver healthcare remotely (1) and it has the potential to increase life expectancy (2-5), prevent disease (6), increase quality of life (7), prolong the amount of time that elderly can live in their own homes (2), decrease hospitalisation rates (2,3), and even lower healthcare costs (2). Mobile health, is a sub-segment of e-health that entails the use of mobile communication devices, such as mobile phones, tablet computers, and PDAs, to provide health services and information (1).
Many different definitions of mobile health exist, with a few recurring concepts. The fundamental notion underlying mobile health is the use of electronic tools to provide health services and information remotely (8). Another important characteristic is that mobile health is platform agnostic, meaning that it can be utilised on a variety of devices (e.g., desktop computer, laptop, tablet, mobile phone) (8). It is used in many different ways, with seven main areas of application: (I) education and awareness; (II) helplines; (III) diagnostic and treatment support; (IV) communication and training for healthcare workers; (V) disease and epidemic outbreak tracking; (VI) remote monitoring; and (VII) remote data collection (9).
Mobile health is delivered in a variety of forms. In one form, known as synchronous technology, patients communicate with healthcare practitioners in real time (e.g., via video), conducting consultations (10). In the asynchronous form of mobile health, communication does not take place in real time; for example, a family physician may take a photograph of a patient’s skin lesion, send it to a dermatologist, and receive an evaluation of the condition afterwards (10).
In Belgium, an e-health platform was introduced in 2008 as part of the Federal Public Service for Health, Food Chain Safety, and Environment Health. This platform enables all actors in the healthcare sector to exchange information safely and efficiently. A key function of the e-health platform is the standardisation of data collection, norms, terminology, and information and communications technology specifications, which is essential for interoperability (11). Currently, this e-health platform does not support mobile health at any level.
More than 100,000 mobile health applications (apps), providing a wide range of health services, are currently estimated to be available. The quality of these apps is not guaranteed and they use their own formats, making integration with other health data extremely difficult and obstructing a large part of their potential benefits. They are used in a very individual way, with no transfer of the data to the software of healthcare providers, which again is a missed opportunity in their potential use. In addition, little evidence-based research on the efficacy of mobile health apps was conducted.
The aim of this study was to examine the perceptions of the adult general population and family physicians in Belgium regarding the use of mobile health apps in primary care. We focused on (I) possible differences in use between the general population and family physicians; (II) the main obstacles the use of mobile health and (III) structural changes that are needed to expand its use.
Methods
Questionnaires
We administered a questionnaire-based survey with closed-ended questions in March 2016. We developed two questionnaires, one for family physicians and one for non-physician respondents, respectively (Supplement I). The questionnaires were designed to explore each group’s viewpoints and to properly direct questions that only physicians could answer. They contained yes-no, multiple-choice, and Likert-scaled questions.
Each questionnaire had two parts: a section containing socio-demographic information and a section containing questions about mobile health. Questionnaire items were validated with a small sample (n=5) selected from each group to ensure clarity of item construction and terminology used. The individuals who participated in the validation of both questionnaires did not participate in the main survey.
Participants
The questionnaires were distributed to potential respondents using email invitations for 300 people from the general population and 300 family physicians and a variety social media channels for non-physicians. The required sample size was not determined a priori. The inclusion criteria were age ≥18 years and internet use. Electronic survey data were collected using the online LimeSurvey tool (LimeSurvey Project Team Hamburg, Germany). The survey was open during 8 weeks and all potential respondents received a reminder to participate in the study. Family physicians received a direct link to the questionnaire that was designed for them and the general population received another link to their questionnaire.
Ethical approval
At the start of the study in March 2016 a permission from an ethics commission was not required, as no patient data or personal health information was obtained. Shortly after the end of the study the regulations were adapted in our country. Nowadays this permission is required for all information collected on individuals.
Statistical analysis
Data cleaning was performed to eliminate duplicate recordings and questionnaires which were completed voluntarily incorrect. Only fully completed questionnaires were withheld. Categorical data were analysed by calculating frequency and relative frequency statistics in Microsoft Excel (Microsoft Office 2016).
Results
Demographic characteristics
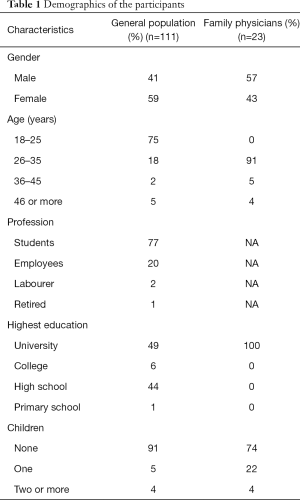
A total of 111 people from the general population [45 (41%) men and 66 (59%) women] completed the questionnaire. A total of 23 family physicians [13 (57%) men and 10 (43%) women] completed their questionnaire. Most of the participants from the general population were aged 18–25 years (75%) and most of the family physicians were aged 26–35 years (91%) (Table 1).
Full table
Awareness and use
Thirty-eight percent of respondents from the general population and 43% of family physicians had ever heard of the term ‘mHealth’ or ‘mobile health.’
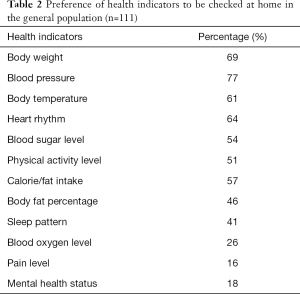
The general-population respondents prefer to have checked their blood pressure (77%), body weight (69%), and heart rhythm (64%) at home, instead of having to visit the doctor or hospital (Table 2). They listed the following main reasons for choosing to use a mobile health app: to save time (72%), due to ease and convenience (61%), and to save on costs (35%); 9% indicated that they would never use an mobile health app. Types of care that general-population respondents indicated they would receive via an mobile health app instead of at doctor or hospital visits were general health check-ups (41%), teleconsultation (5%), follow-up of chronic illness (18%), and monitoring after hospitalisation (12%). Twenty-three percent did not wish to receive any healthcare service via a mobile health app. None of the respondents chose mobile health as an alternative for palliative care. Thirty-five percent of general-population respondents indicated that they received insufficient information about their health or illness in regular consultations, and 33% indicated that they had little face-to-face time with their physician.
Full table
The family physicians indicated that they would like to use mobile health apps to monitor chronically ill patients (17%), to monitor patients who were recently discharged from hospital (17%), and for teleconsultation (4%). Almost two-thirds of the family physicians indicated that they were not interested in offering any type of mobile health service. Among family physicians, 43% reported problems with the exchangeability of data, 37% complained about the difficulties putting relevant data in patient files, and 30% experienced time constraints.
Problems and concerns
The general population sample experienced the following problems as the most important problems outside the visit with the family physicians: 33% indicated that they forgot to take their medication, 25% had difficulties reaching their doctors, and 6% took medication at the wrong time. The main problems that family physicians experienced outside of consultations were answering patients’ post-consultation questions about medication/dosage/side effects (83%) and assessing patient compliance (17%).
The most important concern of general-population respondents about mobile health was related to the quality of care (46%), the impersonal nature of care (23%), and the safety of patient information (23%). The most important concern of family physicians was related to the impersonal nature of care (56%), quality of care (30%) and the safety of patient information (13%).
Twenty-four percent of general-population respondents were prepared to pay more to receive mobile health services. Their main sources of health information besides their personal contact with the physician were: the internet (56%), family members (14%), friends (9%), television (2%), posters at doctors’ practices (2%), fliers at doctors’ practices (1%), and fliers outside of doctors’ practices (1%). Sixty-nine percent of respondents asked their physician for more information after consulting another information source.
Discussion
Awareness
In this survey, a minority of respondents from the general population stated that they had heard of the term ‘mHealth’ or ‘mobile health’. This result is not surprising, as mobile health is not being actively promoted or integrated into the current healthcare system in Belgium (2). Similarly, only 28% of 2,000 UK citizens were able to define the term ‘mobile health’ in a study conducted in 2013 (12). Contrary to our expectation, fewer than half of family physicians in this survey stated that they were familiar with the term. This finding reflects a low degree of awareness of mobile health, even within the medical field. According to the technology acceptance model of Davis et al. (13), awareness of mobile health apps and services, along with their advantages and ease of use, could play an important role in the wider acceptance and adaption of such technologies. Family physicians will need to play a crucial role in their implementation.
Preferred use
Survey results indicated that the preferred model of mobile health services was asynchronous, rather than synchronous. Very few respondents from our study indicated a willingness to use teleconsultation. These results could reflect concern about a lack of quality control and/or the perceived impersonal nature of teleconsultation; respondents in both groups listed these factors as concerns. Another possible reason for these results is that many of our respondents found mobile health services unnecessary. Indeed, the benefits of staying at home might not outweigh negative aspects or concerns for fully mobile people who can readily access their healthcare providers. Individuals with disabilities or chronic conditions may perceive a greater benefit of staying at home and using mobile health apps.
Survey responses indicated more positive attitudes in the general population about the use of mobile health apps for the monitoring of chronic illnesses and conditions, general health assessment, check-ups, and post-hospitalisation follow-up. Fewer family physicians were interested in these services. Whereas about one-quarter of general-population respondents stated that they did not want to receive any form of care via mobile health services, the majority of physicians expressed a lack of interest in providing such services. Like those reported above, these results reflect a preference for an asynchronous mobile health model (i.e., monitoring, patient data collection).
Mobile health could be useful in preventive care (2-5), as addition to, rather than replacement for, existing care. For example, instead of replacing real-life consultation with teleconsultation, family physicians could add support systems to supplement the care already provided. Such models have been implemented in projects such as Flow (14), in which chronically ill patients are monitored via daily scheduled vital-sign assessments and symptom checkers to warn family physicians when any dangerous change may occur. This approach could be expanded further to detect significant weight gain in heart failure patients, or more rapid tracking of the effects of medication on conditions such as high blood pressure, enabling family physicians to faster adapt the treatment. In addition, caloric intake trackers could improve dietitians’ (or family physicians’) monitoring of patients’ eating habits in the context of weight loss programmes. This approach could be combined with the provision of daily scheduled reminders, tailored to individual patients, to avoid certain foods and to encourage better lifestyle choices (15). Participants in cigarette-smoking cessation programmes could benefit similarly from daily scheduled and tailored reminders, daily progression tracking, tracking of the amount of money saved by not buying cigarettes, encouragement messages, and daily tips (16). These proposals are in line with the sentiments of family physicians regarding the monitoring and tracking functions of mobile health apps. Most physicians in this study stated that timely interventions to address potentially harmful conditions, as achieved with mobile health services, could reduce patient care costs in the long term.
Time constraints and issues with information exchange are the main problems encountered by the general population sample and family physicians during and after consultation. Mobile health medication reminders may help to alleviate the problem of patients forgetting to take medication.
Information sources
The internet has clearly become the most important source of medical information, in terms of the acquisition and spreading of health-related messages. A majority of respondents, however, stated that they did ask their doctors for additional information after consulting medical/health information. Health information sources and health awareness programmes that are targeted to specific demographic groups could be used to take advantage of this problem.
Concerns
Quality control of mobile health services is a legitimate concern. The lack of proper regulation and quality control makes it extremely difficult for healthcare workers to recommend mobile health apps, which, in turn, do not exchange mobile health data with medical software. The simple collection of patient data is not sufficient. These data must also be stored easily and exchanged taking into account privacy regulations and accessible without the need to utilise specific software for each app.
Adapted regulations might improve attitudes of the general population and family physicians toward the implementation and use of the mobile health services. The construction of well-regulated platforms with emphasis on information exchange and preventative care could be a good way to further develop and implement mobile health. Standardisation of data storage and exchange could also enable more efficient use of patient data gathered from such platforms.
Another concern was the impersonal nature of care provided in mobile health context. However, in a study conducted in South Korea in 2013 (17), patients’ opinions about the impersonal nature of mobile health changed after they had used it. A way to reduce this concern could be to actively encourage the general population to try mobile health apps. They could be encouraged by a more personal approach of the apps and by a direct benefit of using the apps.
Study limitations
This study has several shortcomings. First, the sample was biased because it was small, and students were over-represented among general-population respondents. Both groups (physicians and non-physicians) are not representative of their respective population as they are younger than their respective population.
These problems might be addressed by extending the survey period and distributing it on more platforms, which might reach a broader section of the population.
Finally, we did not ask respondents whether they had conditions or disabilities that restricted their mobility; thus, we could not compare the responses of abled and less-abled individuals.
Conclusions
In this study, respondents from the general population and family physicians preferred to use mobile health for non-acute care functions, such as monitoring and data collection in chronic diseases. The type of mobile health that should be available in the near future should focus on prevention and early detection of illness, and less on patient assessment and treatment from a distance.
Supplement I
Questionnaire for the general population (English translation)
Mobile health applications can enable teleconsultations, which are doctor visits in your own home via video communication comparable to Skype conversations; mobile health enables the monitoring of chronic diseases (heart failure, COPD, asthma…) from your home; mobile health enables doctors to monitor your health after you leave the hospital.
1.Please state your year of birth in numbers (for example, 1989): …
2.Please select your sex (choose one option)
- Male
- Female
3.Select your current occupation (choose one option)
- Student
- Employee
- Labourer
- Pensioner
- Other: …
4.What is the highest level of education you finished successfully? (choose one option)
- Primary school
- Secondary school
- College
- University
- None
- Other: …
5.Select the number of children you have:
- 0
- 1
- 2 or more
6.What is your current marital status? (choose one option)
- Married
- Cohabiting
- Single
- Other: …
7.Have you heard of the term mHealth or mobile health? (choose one answer)
- Yes
- No
8.Which health parameters would you personally prefer to have monitored from your home instead of having them measured at your doctor’s practice or hospital? (multiple answers are possible)
- Weight
- Blood sugar level
- Blood pressure
- Temperature
- Blood oxygen level
- Exercise/physical activity
- Calorie/fat intake
- Pain level
- Sleep pattern
- Heart rhythm
- Mental health status
- Other: …
9.What are the main reasons you would choose to utilise mobile health instead of visiting your doctor? (multiple answers are possible)
- Time saving (waiting times, transportation)
- Ease, you can stay at home
- Cost saving (transport costs, etc.)
- I would never use mobile health applications
- Other: …
10.What kind of healthcare would you prefer to receive via mobile health instead of having to visit your doctor’s practice or hospital? (choose one option)
- General health/check-up
- Teleconsultation
- Monitoring of previous (chronic) condition
- Monitoring after leaving hospital
- Palliative care
- None, I would always rather go to my doctor or hospital
- Other: …
11.What are the biggest problems you encounter during your doctor’s visits? (choose one option)
- Accessing your medical information quickly (medicines, investigations)
- Too little face-to-face time with your doctor
- Other: …
12.What are the biggest problems you encounter outside your doctor’s visits? (choose one option)
- Forgetting to take my medication
- Taking medication at wrong times
- Difficulty contacting my doctor
- Other: …
13.What are your biggest concerns regarding mobile health? (choose one option)
- Impersonal nature of the care
- Security: having your medical data stolen/lost
- Quality of the care you would receive
- Cost: having to pay additional costs for the devices needed
- Other: …
14.Would you be willing to pay an additional fee for e-health services? (choose one option)
- Yes
- No
15.Which source do you consult for information concerning health? (choose one option)
- Friends and acquaintances
- Family
- Posters at my doctor’s office
- Posters outside of my doctor’s office
- Fliers at my doctor’s office
- Fliers outside of my doctor’s office
- Internet
- TV
- Radio
- Newspaper
- Other:
16.Have you ever asked your doctor for additional information after consulting one of the above sources? (choose one option)
- Yes
- No
Questionnaire for family physicians (English translation)
Mobile health applications can enable teleconsultations, which are doctor visits in patients’ own homes via video communication comparable to Skype conversations; mobile health enables the monitoring of chronic diseases (heart failure, COPD, asthma…) from patients’ homes; mobile health enables you to monitor your patients’ health after they leave the hospital.
1.Have you heard of the term mHealth or mobile health? (choose one answer)
- Yes
- No
2.Which health parameters would you personally prefer to monitor from your office? (multiple answers are possible)
- Weight
- Blood sugar level
- Blood pressure
- Temperature
- Blood oxygen level
- Exercise/physical activity
- Calorie/fat intake
- Pain level
- Sleep pattern
- Heart rhythm
- Mental health status
- Other: …
3.What kind of healthcare would you prefer to offer via mobile health instead of having your patients come to you? (choose one option)
- General health/check-up
- Teleconsultation
- Monitoring of previous (chronic) condition
- Monitoring after leaving hospital
- Palliative care
- None, I would always rather have my patients come to me
- Other: …
4.What are the biggest problems you encounter during a consultation? (choose one option)
- Exchangeability of data
- Reliability of investigations
- Reliability of sources
- Difficulties inputting relevant data in patient files
- Too little time
- Other:
5.What are the biggest problems you encounter outside of your consultation? (choose one option)
- Assessing patient compliance
- Answering patient questions about medication/dosage/side effects
- Other: …
6.What are you biggest concerns regarding mobile health? (choose one option)
- Impersonal nature of the care
- Security: having medical data stolen/lost
- Quality of the care patients would receive
- Cost
- Other: …
7.What impact do you believe the use of mobile health could have on your way of working? (choose one option)
- I would be able to make quicker medical decisions
- I would spend less time on administrative tasks
- I would be able to communicate with other doctors more easily
- I would have more time for my patients
- None
- Other: …
8.Select a number from 1 to 10 for the following statements, where 1 stands for “I would never use this” and 10 stands for “I would use this for all of my patients”
- I would utilise teleconsultation
- I would utilise data gathered via mobile health applications
9.Do you believe that you would benefit financially by implementing mobile health applications? (choose one option)
- Yes, I would spend less time on each patient
- Yes, I would have fewer interruptions
- Yes, pre-emptive interventions for certain potentially dangerous conditions could save costs in the long run
- No, I would conduct fewer interventions
- No, it would cost me more time
- No, software and hardware costs would outweigh potential cost savings
- Other: …
10.Which other methods would you use to conduct health awareness programmes? (choose one option)
- Letter correspondence
- My website
- Social media
- Via SMS messaging
- Via mobile apps
- Other: …
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: At the start of the study in March 2016 a permission from an ethics commission was not required, as no patient data or personal health information was obtained.
References
- World Health Organization. Global diffusion of eHealth: Making universal health coverage achievable. Report of the third global survey on eHealth. Available online: (2016, accessed 10 January 2018).http://apps.who.int/iris/bitstream/10665/252529/1/9789241511780-eng.pdf?ua=1
- mHealth als sleutel tot kwaliteit en betaalbare zorg. Whitepaper Voka Health Community mobile Health. Available online: (2015, accessed 10 January 2018).https://www.voka.be/sites/voka.prod.wunderkraut.be/files/files/Vlaanderen/Overige%20pdf%20documenten/Whitepaper%20Health%20Community%20%27mHealth%27_lowres.pdf
- Dendale P, De Keulenaer G, Troisfontaines P, et al. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail 2012;14:333-40. [Crossref] [PubMed]
- Inglis SC, Clark RA, McAlister FA, et al. Structured telephone support or telemonitoring programmes for patients with chronic heart failure. Cochrane Database Syst Rev 2010. [PubMed]
- Kvedar J, Coye MJ, Everett W. Connected health: a review of technologies and strategies to improve patient care with telemedicine and telehealth. Health Aff (Millwood) 2014;33:194-9. [Crossref] [PubMed]
- Burke LE, Ma J, Azar KM, et al. Current Science on Consumer Use of Mobile Health for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation 2015;132:1157-213. [Crossref] [PubMed]
- Rossi MC, Nicolucci A, Di Bartolo P, et al. Diabetes Interactive Diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life: an open-label, international, multicenter, randomized study. Diabetes Care 2010;33:109-15. [Crossref] [PubMed]
- World Health Organization. mHealth: New horizons for health through mobile technologies, WHO Press, Switzerland. Available online: (2016, accessed 10 January 2018).http://www.who.int/goe/publications/goe_mhealth_web.pdf
- Adibi S. editors. mHealth Multidisciplinary Verticals. 1 edition. CRC Press (Taylor & Francis Group), 2014, USA.
- Center For Connected Health Policy. what is telehealth? Available online: (2010, accessed 10 January 2018).http://cchpca.org/what-is-telehealth
- E-health, over het e-health platform. Available online: (2016, accessed 10 January 2018).https://www.ehealth.fgov.be/ehealthplatform/nl
- Digital health. The opportunity for patients, businesses and healthcare providers (Pinsent Masons), 2013, England. Available online: (2013, accessed on 10 January 2018).https://www.pinsentmasons.com/PDF/Digital-Health-Winter-2013.pdf
- Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: A comparison of two theoretical models. Management Science 1989;35:982-1003. [Crossref]
- Florence, the concept. Available online: (2016, accessed 10 January 2018).https://www.getflorence.co.uk/
- Lyzwinski LN. A systematic review and meta-analysis of mobile devices and weight loss with an intervention content analysis. J Pers Med 2014;4:311-85. [Crossref] [PubMed]
- Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control 2005;14:255-61. [Crossref] [PubMed]
- Lee J, Rho MJ. Perception of Influencing Factors on Acceptance of Mobile Health Monitoring Service: A Comparison between Users and Non-users. Healthc Inform Res 2013;19:167-76. [Crossref] [PubMed]
Cite this article as: Mutebi I, Devroey D. Perceptions on mobile health in the primary healthcare setting in Belgium. mHealth 2018;4:44.


