
The use of telemedicine in the preoperative management of pheochromocytoma saves resources
Introduction
Pheochromocytomas are rare tumors of neuroectodermal origin. They most frequently arise from the adrenal medulla as functional tumors secreting catecholamines (norepinephrine, epinephrine, and dopamine) (1). Signs and symptoms are related to the effect of circulating catecholamines and include headaches, tachycardia, hypertension, palpitations and anxiety (2). Chronic alpha-adrenergic stimulation results in vasoconstriction and diminished plasma volume leading to cardiovascular sequelae including myocardial infarction, cardiomyopathy, cardiac dysrhythmias, and stroke (3).
Surgical resection is the appropriate treatment of pheochromocytoma but requires preoperative alpha-adrenergic blockade to minimize the risk of perioperative cardiovascular complications (4). While some studies question the required use of preoperative pharmacological preparation, especially in normotensive pheochromocytomas, it is widely-accepted that pre-operative alpha blockade is necessary (5). Alpha blockade prevents unopposed alpha-adrenergic stimulation resulting in vasodilation and associated intravascular volume depletion (3). Volume expansion is recommended through preoperative hydration and the adherence to a high sodium diet (6).
Historically, patients required preoperative hospitalization with aggressive titration of alpha-antagonists and saline infusion for several weeks (7). Due to multiple orally-available alpha-antagonists, outpatient preoperative alpha-blockade is the current standard of care (8). Although a great improvement, this plan requires frequent dose titration and multiple preoperative visits to assess for orthostatic hypotension, measuring blood pressure (BP) and heart rate (HR) as well as monitoring pharmacologic side effects.
Here, we hypothesize that pre-operative telecommunication between patients and physicians for the preparation of resection of pheochromocytomas is a safe and effective method of significantly reducing preoperative clinic visits and time to surgical resection while conserving limited medical resources.
In surgical care, telemedicine has been more commonly used for postoperative purposes, such as monitoring surgical drain output for breast surgery via text messaging (9). Even more, newer technology devices like smartphone apps have been used in order to improve treatment adherence and BP monitoring in post transplanted kidney patients (10). Video conferences have been used to evaluate urologic postoperative outcomes in children (11), or ileostomy outputs after discharge (12), through this channel physicians may immediately suggest therapeutic actions to improve patient´s conditions.
Other information that may be exchanged by telemedicine resources are videos or photos, so surgeons have been able to evaluate patient´s abdominal wounds after appendectomy (13) or neck wounds after parathyroidectomy (9) without face-to-face consultation.
Telemedicine in surgical preoperative assessment or diagnosis has already been described, although it has been more widely applied for post-operative follow up. For preoperative management, a group of pediatric surgeons (14), used a telephone-based videoconference, preoperative assessment occurred in 32.8% of their patients which included any required preoperative teaching of the family.
For preoperative diagnosis and assessment, telemedicine has proven to be safe and effective in different types of surgery; for maxillofacial surgery (15), surgical trauma (11) for plastic surgeon evaluation in a military facility (9), neonatal surgical consultation for diagnosis and operative plan if needed (16), preoperative bariatric surgery consultations (17) prescreening of possible surgical patients of remote areas (18).
Methods
A retrospective review of surgically managed pheochromocytomas by a single surgeon at our institution was performed, 14 patients who were treated preoperatively with frequent clinic appointments for orthostatic evaluation and alpha-blockade dose titration were considered as the “control group”.
Usually, the patients in preoperative alpha blockade are who asks them to sit down for at least five minutes, then their BP and HR are evaluated while seated and in standing position. Their BP and HR are registered at their medical records, the targeted BP is <130/80 mmHg while seated and a systolic BP greater than 90 mmHg while standing, with a target HR of 60–70 bpm seated and 70–80 bpm standing (3). Afterwards the surgeon checks the medical files and asks for data of orthostatic hypotension, such as lightheadedness or dizziness when standing up, if treatment titration is needed the physician makes the appropriate changes. As soon as they reach the targeted measures, surgery is scheduled.
The patients known as the “study group” were another 14 patients with diagnosed pheochromocytoma who were not available for weekly clinic visits, so at their first clinical appointment they were educated by a nurse on the use of a sphygmomanometer, HR measurement and the accurate detection of orthostatic hypotension (19), they were given a prescription for alpha-blockade agent and written instructions that specified the e-mail address, the information they must provide in each e-mail and the days of the week they should be writing (Monday and Friday until 8 pm). Subsequently, the surgeon, on a biweekly basis, revised and replied the e-mails and if needed, dose escalation was appointed. When the patients reached the targeted BP and HR, they were asked to come by the clinic to schedule for surgery.
Afterwards the comparison between groups were performed using a t-test or a chi-square test as appropriate, using the SPSS software version 19.0, and the statistical significance was defined at the level of P<0.05.
Ethics approval was not required as data in this study was collected prior to the need for IRB approval for retrospective studies at our institution.
Results
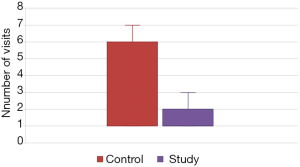
Twenty-eight patients were included, the two groups were similar in terms of age, sex, race, and tumor size (Table 1). Perioperative characteristics (Table 2) such as estimated blood loss, type of surgery (laparoscopic or open) and complications were also similar, active patient participation in pre-operative alpha blockade therapy resulted in significantly fewer preoperative visits (mean 1.52 vs. 3.20 visits; P=0.02) (Figure 1) as well as in a significantly shorter time from initiation of blockade to resection (33 vs. 82 days; P=0.03). Two patients had their surgeries postponed due to inadequate control upon arrival to the hospital the day of surgery (one in each group) so they were not considered in the analysis.

Full table
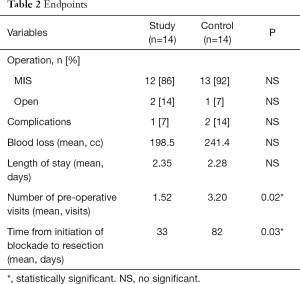
Full table
Discussion
Telemedicine in surgery has become a useful tool for patient care delivery although it is not accessible to all the patients or health providers (20).
In this example, titration of alpha blockade therapy through patient and surgeon e-mail correspondence is efficacious as well as safe and it saves limited resources and time. It also allows patients to prepare for surgery in a non-hospital environment and less working days lost. Because pheochromocytomas are frequently treated at distant tertiary referral centers, this process eliminates unnecessary travel time and expenses for the patient, preserving its quality of life. Furthermore, it has already been identified that the total in-hospital cost for patients with pheochromocytoma is approximately $50,000 compared with $41,000 for other adrenal masses (21).
Assessment of BP and HR as an outpatient was described by Witteles et al. (7), before 1987, patients with pheochromocytoma were hospitalized for preoperative treatment. The authors compared the costs of preoperative treatment of patients as outpatients vs. hospitalized. In this scenario the outpatients made a phone call to their anesthesiologist who would adjust their medication as needed, no information about preoperative clinic visits is given but preoperative hospital stay in this group was significantly shorter than in inpatients (3.27 vs. 12.82 days, P=0.002). No other reference in the literature was found about this kind of action.
The costs of telemedicine have not been widely analyzed, though it is known that it saves patients’ and hospitals’ resources. It also provides a mean of communication between physicians to exchange knowledge, information and advice in real time scenarios. Telemedicine has even been used to mentor surgical procedures. We should try to widen the field of preoperative management, some of the future perspectives should focus on photographic assessment of a wound bed for skin grafting, follow up of a kidney stone with serial X-rays sent to the doctor, if it fails to be expulsed, schedule a procedure. Anesthesiologist may also benefit from telemedicine to follow-up comorbid conditions that should be controlled before a surgical procedure such as tobacco use, glycemic control, anemia, obesity.
Conclusions
Due to these benefits, compared with usual care, this e-mail based pre-operative management should be implemented in the routine surgical care of pheochromocytomas, as it diminished preoperative visits and the mean time since initiation of management to surgery. Technology is nowadays an important tool for our society, doctors need to be encouraged to use telemedicine as part of its daily practice as long as it is safe and satisfying for the patient.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethics approval was not required as data in this study was collected prior to the need for IRB approval for retrospective studies at our institution.
References
- Lenders JW, Eisenhofer G, Mannelli M, et al. Phaeochromocytoma. Lancet 2005;366:665-75. [Crossref] [PubMed]
- Salinas FV. Contemporary Perioperative and Anesthetic Management of Pheochromocytoma and Paraganglioma. Adv Anesth 2016;34:181-96. [Crossref]
- Lenders JW, Duh QY, Eisenhofer G, et al. Pheochromocytoma and paraganglioma: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 2014;99:1915-42. [Crossref] [PubMed]
- Scholten A, Cisco RM, Vriens MR, et al. Pheochromocytoma crisis is not a surgical emergency. J Clin Endocrinol Metab 2013;98:581-91. [Crossref] [PubMed]
- Lafont M, Fagour C, Haissaguerre M, et al. Per-operative hemodynamic instability in normotensive patients with incidentally discovered pheochromocytomas. J Clin Endocrinol Metab 2015;100:417-21. [Crossref] [PubMed]
- Pacak K. Approach to the patient: Preoperative management of the pheochromocytoma patient. J Clin Endocrinol Metab 2007;92:4069-79. [Crossref] [PubMed]
- Witteles RM, Kaplan EL, Roizen MF. Safe and cost-effective preoperative preparation of patients with pheochromocytoma. Anesth Analg 2000;91:302-4. [PubMed]
- Naranjo J, Dodd S, Martin YN. Perioperative Management of Pheochromocytoma. J Cardiothorac Vasc Anesth 2017;31:1427-39. [Crossref] [PubMed]
- Scerri GV, Vassallo DJ. Initial plastic surgery experience with the first telemedicine links for the British Forces. Br J Plast Surg 1999;52:294-8. [Crossref] [PubMed]
- Jasim S, Suman VJ, Jimenez C, et al. Phase II trial of pazopanib in advanced/progressive malignant pheochromocytoma and paraganglioma. Endocrine 2017;57:220-5. [Crossref] [PubMed]
- Wallace DL, Jones SM, Milroy C, et al. Telemedicine in acute plastic surgical trauma and burns. J Plast Reconstr Aesthet Surg 2008;61:31-6. [Crossref] [PubMed]
- Bednarski BK, Slack RS, Katz M, et al. Assessment of Ileostomy Output Using Telemedicine: A Feasibility Trial. Dis Colon Rectum 2018;61:77-83. [Crossref] [PubMed]
- Segura-Sampedro JJ, Rivero-Belenchón I, Pino-Díaz V, et al. Feasibility and safety of surgical wound remote follow-up by smart phone in appendectomy: A pilot study. Ann Med Surg (Lond) 2017;21:58-62. [Crossref] [PubMed]
- Postuma R, Loewen L. Telepediatric surgery: capturing clinical outcomes. J Pediatr Surg 2005;40:813-8. [Crossref] [PubMed]
- Wood EW, Strauss RA, Janus C, et al. Telemedicine Consultations in Oral and Maxillofacial Surgery: A Follow-Up Study. J Oral Maxillofac Surg 2016;74:262-8. [Crossref] [PubMed]
- Robie DK, Naulty CM, Parry RL, et al. Early experience using telemedicine for neonatal surgical consultations. J Pediatr Surg 1998;33:1172-6; discussion 1177. [Crossref] [PubMed]
- Sudan R, Salter M, Lynch T, et al. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg 2011;202:71-6. [Crossref] [PubMed]
- Lee S, Broderick TJ, Haynes J, et al. The role of low-bandwidth telemedicine in surgical prescreening. J Pediatr Surg 2003;38:1281-3. [Crossref] [PubMed]
- Freeman R, Wieling W, Axelrod FB, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 2011;21:69-72. [Crossref] [PubMed]
- Asiri A, AlBishi S, AlMadani W, et al. The Use of Telemedicine in Surgical Care: a Systematic Review. Acta Inform Med 2018;26:201-6. [Crossref] [PubMed]
- Parikh PP, Rubio GA, Farra JC, et al. Nationwide review of hormonally active adrenal tumors highlights high morbidity in pheochromocytoma. J Surg Res 2017;215:204-10. [Crossref] [PubMed]
Cite this article as: Heslin MJ, Liles JS, Moctezuma-Velázquez P. The use of telemedicine in the preoperative management of pheochromocytoma saves resources. mHealth 2019;5:27.


