mHealth and patient generated health data: stakeholder perspectives on opportunities and barriers for transforming healthcare
Introduction
Healthcare systems are charged with providing efficient, safe, high quality and patient-centered care while managing costs and resources. Innovations in care delivery, including effective strategies to engage with patients to improve care delivery, are one-way health systems seek to transform healthcare. Incorporating patient-generated health data (PGHD) in clinical care is one way to engage patients in clinical decision making. PGHD is defined as “data created, recorded, and gathered by and from patients” often through the use of technology such as smartphones and wearable devices (1,2). Wearable devices, mobile health apps, and geolocation technologies place the ability to track, monitor and report data in the individuals’ hands—or on their bodies. In this manner, individuals are able to document information about health and well-being, monitor activity levels, improve self-awareness of health, and leverage tools to better manage health conditions. The ability to create better “connected health,” where individuals collect data outside of the healthcare encounter and report it to their provider, has great potential to impact the delivery of healthcare through remote monitoring, and by allowing patients and healthcare teams to provide targeted and efficient care that aligns with the health status of individual patients (2,3). PGHD can also facilitate increased access to longitudinal data about an individual’s health, and improved engagement and communication with providers and healthcare teams (2,4).
While PGHD offers an opportunity to provide a more robust view of an individual’s health and wellness, healthcare systems have been slow to formally integrate PGHD into clinical workflows and care transformation. Integration of PGHD presents a host of challenges that health systems must consider, including data security and privacy, data standardization, workflow integration, and device interoperability (3). For example, in the context of clinical care, potential efficiencies created by PGHD collection could be outweighed by the added burden of PGHD review (5). Other concerns include the potential for PGHD to create or contribute to care inequities for individuals not able to track PGHD because of their disease make-up, level of engagement, access to technology, or the reimbursement capacities of their medical coverage (6). For both healthcare consumers and providers, questions remain about the content and frequency of data types that would be most helpful to support health monitoring and clinical decision-making (3). To support the scale and spread of PGHD use across healthcare systems, more needs to be understood about current PGHD utilization including the diversity of data collected, intentions for data use, impact on health information technology systems, and effect on healthcare delivery from diverse healthcare stakeholders.
Methods
We sought to engage a range of stakeholders involved in PGHD use to examine their perspective on the value of and challenges to PGHD integration in clinical care. Stakeholders included patients and care partners, healthcare providers, and healthcare administrators. Our goal was to understand stakeholder experience with PGHD, explore stakeholder perspectives on the opportunities and challenges presented by incorporating PGHD into clinical care, and identify the most pressing and impactful areas to advance the integration of PGHD. We conducted open-ended interviews with three stakeholder groups: healthcare consumers (patients and care partners), healthcare providers, and healthcare administrators. Interview guides were iteratively developed by the project team in collaboration with our research partners, including the University of Washington (UW) Medicine Committee for Digital and Connected Health (CDCH), external stakeholders with expertise in PGHD, and our patient partners. Interviews focused on stakeholder perceptions of value and barriers to PGHD use.
We used a combination of open recruitment and purposive sampling approaches to identify eligible participants that represented the breadth of PGHD use in research and clinical care. Healthcare consumers were identified through outreach to patient advisory and research networks, and potential participants were screened via survey, which allowed our purposive sample to include a wide range of PGHD use (e.g., health and well-being or symptom management) and a diverse group of patient and care partner interviewees. UW Medicine healthcare providers were identified through the study team’s previous work cataloging clinical use cases of PGHD, and through directed outreach (7). Finally, we identified healthcare administrators involved in health system-wide care transformation and invited them to participate in interviews.
All interviews were audio recorded, transcribed, and analyzed using a web-based qualitative data management program (8). A preliminary coding schema was developed by the project team using open coding methodology. This schema was further refined throughout the coding process, with additional sub-codes developed inductively as appropriate. A consensus coding strategy was employed, where select members of the study team with expertise in qualitative analysis co-coded and reconciled transcripts to increase validity of codes. Themes identified by the analysis team were reviewed and finalized by the full team for additional feedback and validation.
The University of Washington Institutional Review Board reviewed this project and granted an exempt determination on 5/31/2017.
Results
We conducted interviews with healthcare consumers [21], healthcare providers [15], and healthcare administrators [5], a total of 41 interviews. Healthcare consumer interviewees represented a broad range of experience with healthcare utilization, as well as a breadth of interest in the use of PGHD for wellness, health management, and condition-specific treatment. Healthcare provider interviewees represented 12 specialties or areas of care, including psychiatry, rehabilitation, surgery, nephrology, oncology, and primary care. Additionally, the healthcare provider interviewees were from diverse medical specialty areas (e.g., medicine, nursing, physical therapy). Healthcare administrator interviewees held a variety of leadership positions within the health system, with responsibilities related to care transformation, strategic planning (e.g., fiscal, IT, etc.), and clinical operations management.
Themes identified across interviews related to tracking health behaviors, data sharing experiences, the value of PGHD, barriers to expanded use, and unintended consequences, as described in the following sections. Interviewees described diverse experiences with PGHD, from routine health and wellness tracking supporting the management of complex and progressive diseases. Across the stakeholder groups, consistent themes emerged around the value of PGHD for use cases where PGHD directly supports or enhances care decisions and the potential for PGHD to improve the communication and engagement between healthcare consumers and providers. The interviews highlighted the most promising use cases for the integration of PGHD into routine care, in particular through their inclusion in formal care pathways. The interviews also identified significant barriers to PGHD use in clinical care, including challenges around understanding data validity and actionability, and the added burden to integrate PGHD into care processes. Finally, the interviews highlighted the unanticipated consequences of collecting and reporting PGHD.
Theme 1: PGHD tracking supports many healthcare goals and behaviors
Interviewees discussed experiences with a range of PGHD collected and reported through various modalities. Table 1 presents the types of data and modalities for tracking PGHD reported by interviewees. In many cases, healthcare consumers reported tracking multiple types of data through different modalities simultaneously. A number of those interviewed also noted the use of diaries to collect narrative content or to allow for tailored tracking of information related to their condition. Care partners often referenced diaries as an important way for organizing and managing data both tracked by the individual as well as captured by the provider during office visits.
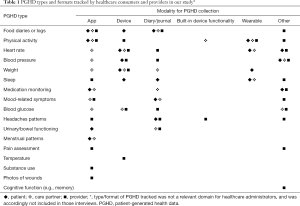
Full table
Healthcare providers we interviewed discussed PGHD primarily related to their clinical specialty. For example, behavioral health specialists focused on mental health and behavior data, whereas primary care providers focused on clinical measures, such as home monitoring of blood pressure. In addition to PGHD referenced in Table 1, healthcare providers discussed the use of validated assessments for patient-reported outcomes and standardized symptom ratings including function, depression, and pain. A few healthcare providers reported experience with app development to support tracking PGHD based on an identified need within their practice. The majority of providers reported experience conducting clinical research including PGHD captured via tracking devices, often with the aim to inform future use of PGHD in clinical practice.
Theme 2: people are intentional about when and what type of data they share with their providers.
Healthcare consumers reported diverse uses of PGHD including monitoring general health and well-being, advancing personal health goals, and managing clinical conditions. Individuals reported tracking data both for personal use and for sharing with healthcare providers. Individuals decided whether to share PGHD with their providers based on whether the individual believed sharing it would further their goals for the healthcare visit. PGHD tracked solely for the purpose of wellness or advancing personal health goals were typically not shared with providers. Goals expressed by healthcare consumers for sharing PGHD with providers included improving efficiency of communication about health experience, enhancing the ability to convey health status and concerns, and providing data to inform treatment decisions. Healthcare consumers recognize that time with providers is limited and they view sharing PGHD as an opportunity to maximize the time available by preparing for healthcare discussions ahead of time and presenting data about their health in an efficient way. PGHD may be presented to providers by individuals at the time of the appointment or sent in advance of appointments for providers to review (e.g., through the patient portal).
I felt like it was more efficient to have the information all collected and then be able to relay that to my doctor…and then when I went in to see her, we could just talk immediately, like, “Okay, so here are the various options available to you. Now we have time for you to ask questions about these different options and discuss what would work best for you.”—Healthcare Consumer
PGHD is not always viewed by healthcare consumers as important for informing healthcare decisions or discussions in the context of formal healthcare settings. This is reinforced through the lack of inquiry about PGHD from providers noted by healthcare consumers. Importantly, the extent to which people believe providers find tracking data useful influences the extent to which people share PGHD in the healthcare setting. Healthcare consumers report that lack of buy-in or dismissive attitudes toward PGHD by health care providers or systems can result in selecting not to continue sharing data with their providers. In some instances, providers not valuing PGHD leads individuals to find new providers who support engaged discussions of PGHD.
Theme 3: the value of PGHD increases with alignment to measurement-based care
Across stakeholder groups, PGHD that provides actionable information for the end-user is most valued. Healthcare consumers and providers recognize that as data aligns with measurement-based care, in which data is systematically collected to monitor patient progress and inform care decisions (9), the value of PGHD increases.
My clinician had the data, I had the data, we could see where we needed to focus in the coming year on what was not responding or hadn’t responded enough, and also adjust medications to hopefully improve what we were aiming for.—Healthcare Consumer
This holds true both outside of, and within, the formal healthcare setting. Healthcare consumers who track PGHD solely for self-management find it an effective tool for tracking goals and goal attainment when captured in a manner that can inform and guide behavior. PGHD also offers an effective strategy for managing multiple dimensions of health, such as medication management, monitoring symptoms, and documenting biometric data. Tracking PGHD provides healthcare consumers with an increased awareness of their health, and the ability to better engage in care with their healthcare providers.
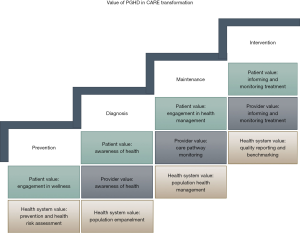
Healthcare providers report that when the type of data tracked by patients aligns with clinical treatment pathways, PGHD improves patient engagement and increases the value of PGHD in clinical care (Figure 1). Healthcare providers who incorporate PGHD into patient care strategies also recognize the opportunity PGHD provides to better understand an individual’s health outside of the healthcare encounter. This information supports efforts to understand common health behaviors and habits, identify trends in symptoms experienced as well as quantify responses to treatment regimens.
One person in particular who…decided on her own that she was so eager about her activity change that she was going to buy [an activity tracker] …and then brought it into one of the next sessions. So then we really started talking about using it and doing some goal-setting…and it just gave us this very nice concrete thing to look at together, and it kind of anchored our treatment.—Healthcare provider
Healthcare providers and administrators note the value of PGHD in supporting remote monitoring. PGHD is viewed as a way to expand care for individuals who have limited access to healthcare and to improve care for those with acute or chronic conditions that can benefit from additional monitoring between healthcare encounters. Healthcare administrators see the use of PGHD as a way to better engage patients in their use of the patient portal and electronic health records. As clinical measures are increasingly tied to performance and payment metrics, system leaders are motivated to ensure clinical data accurately reflects the health status of their patient populations. Understanding behaviors and health risk present opportunities to better support population health and promote patient wellness activities.
Theme 4: data provides a common framework that facilitates patient engagement
Healthcare consumers tracking PGHD report increased awareness of health, providing a sense of confidence in their ability to accurately recall past events and communicate with providers about health trends and decisions around treatment regimens. PGHD can also inform the decision to seek out care when trends in data become concerning. Healthcare consumers also note that data provides tangible evidence of health experiences that they perceive as being taken more seriously by providers than verbal or descriptions of symptoms.
Instead of me just going, “No, really, guys”, it’s like, “Look. I can show you this date to this date and this happened.” So, it shows that I’m being serious about managing it and being on top of it.—Healthcare consumer
Providers value the ability to better understand patient health outside of clinical encounters. The ability to see trends captured through PGHD supports discussions about health status and decisions about changes to treatment regimens. This ability to engage with patients promotes the sense of providing patient-centered care. Related is the perception reported by providers that tracking PGHD demonstrates patient engagement in and accountability for health management, which further supports improved communication. Providers also believe that PGHD helps circumvent the potential for patients to be influenced by social desirability bias in reporting what they believe the provider wants to hear and decreases the influence of stigma in addressing sensitive health concerns.
Theme 5: the promise of PGHD is tempered by lack of standards
Despite the value PGHD offers, barriers exist that temper scaled integration within healthcare delivery (Table 2). Capturing and utilizing PGHD requires effort, time, and resources on behalf of both the healthcare consumer and, when shared, healthcare teams. While diverse modes of tracking data allow healthcare consumers to test and select methods that work best for their needs, the diversity of data types and modes presents a challenge when managing data across multiple platforms. Interoperability between devices and platforms, or single platforms that support tracking across multiple dimensions of health, would reduce this complexity and facilitate sustained use.

Full table
Providers and patients also face dilemmas in how much to tailor PGHD tracking and reporting tools to patient needs and preferences. Greater personalization may reduce the burden of collecting this data for patients, but then providers must respond to more types of data from different tracking modalities presented in different formats (or using different measurement standards), thus increasing provider burden. The lack of standards around how data is tracked using different technologies, interoperability across devices and platforms, and a lack of evidence-based interpretation of data further limits the clinical utility of PGHD.
The risk, if it’s not made easy, is that it gets ignored. Again, you can have as much PGHD as you want, but if people aren’t able to read it, interpret it, and act upon it, it’s kind of worthless.—Healthcare provider
Healthcare administrators identify several key barriers to system-level integration of PGHD, citing the potential burden on providers and healthcare teams, including the impact on resources and workflow within the clinic, and the intensive need for training on data interpretation and use. Administrators emphasized the importance of carefully selecting clinical contexts for PGHD use and alignment with existing health system structures and standards, such as leveraging the electronic medical record to standardize how data is received and reviewed by providers. Administrators also noted that current payment models do not support PGHD. The lack of reimbursement mechanisms and healthcare policy supporting PGHD use hinders the advancement of PGHD within the health system.
Theme 6: unintended consequences of PGHD need further exploration
Indirect and unexpected outcomes of tracking PGHD emerged from interview discussions. Most notable is the potential for increased anxiety or emotional stress for healthcare consumers who track PGHD. This may be caused by increased awareness of declining health, hyper-focus on data, the burden associated with tracking data, and feelings of failure or inadequacy if unable to track data. Healthcare consumers also expressed that tracking PGHD can alter relationships with family members, friends, and healthcare providers. Individuals serving as care partners noted that both the process of tracking as well as discussions about PGHD could negatively impact relationships with family members or friends through perceived changes to the power balance and by creating a heightened focus on health.
It’s really become a parent-child-esque relationship and we both wish things could go back to the way things were. I mean of course she’s thankful for the stability now…It’s strained our relationship for sure.—Care partner
Positive unintended consequences of PGHD tracking included triggering the decision to pursue medical care to address changing symptoms, better access to social support through communities created through app-based technology, enhanced motivation through gamification-enabled applications, and improved self-awareness and confidence in health management for other aspects of health.
Discussion
With the growing prevalence of chronic conditions requiring changes in lifestyle and at-home self-management, there is increased interest in and need for integrating data from beyond the clinic visit to successfully diagnose and manage health and achieve optimal health outcomes. These changes, coupled with a burgeoning consumer market for products that allow individuals to more readily track personal health data, underlie health system level efforts to leverage PGHD in healthcare transformation. Translating advances in technology and data tracking into successful clinical implementation requires a robust understanding of how stakeholders conceptualize and make use of PGHD, the potential value that PGHD can add to care, and the challenges that may limit PGHD’s promise. The interview results reported here provide rich context and understanding of the experiences and needs of the healthcare consumers, healthcare providers, and healthcare administrators who interface with PGHD.
Interviewees enumerated a range of benefits for using PGHD, indicating broad agreement that PGHD is a valuable addition to clinical care. In particular, healthcare consumers and providers both report a high value for bringing PGHD into the healthcare encounter when it can directly support clinical decision making and measurement-based care. This finding highlights the opportunity to align PGHD integration with care pathways that can benefit from the type of granular, ongoing availability of data that PGHD enables. However, healthcare consumers may elect not to share PGHD with providers when they believe the data is not relevant to the goals of the healthcare encounter. Further, perceptions of provider attitudes toward PGHD can act to dissuade patients from sharing data that would be relevant to care. Open conversations between providers and healthcare consumers about the role of PGHD in healthcare help set the stage for incorporating PGHD in ways that can improve patient engagement, enable patient-provider communication, and support attainment of health goals. For example, Chung et al demonstrated the value of PGHD in GI disorders and healthy eating, stressing the importance of goal alignment, articulating how tracking supports the goal, and a shared understanding of when and by whom data will be reviewed (10). Our results build on these findings, further demonstrating the potential for PGHD to inform and support goal attainment and patient-provider communication across health conditions.
We undertook this study to understand what is needed to support health systems implementation of PGHD. Directly engaging people with experience using PGHD provides important insight on the opportunities and challenges presented by incorporating PGHD to advance clinical care. Our interviews also found that while there is momentum to integrate PGHD meaningfully into clinical care, additional demonstration of its benefits may be required. This includes not only identifying the most pressing and impactful areas to advance the integration of PGHD within the health system, but also examination of which health conditions, types of PGHD, or methods of tracking demonstrate clear potential to improve outcomes.
While those interviewed reflect individuals who believe that PGHD offers an important dimension to healthcare, interviewees also recognize that utility of PGHD is currently limited due to barriers that hinder the ability to scale integration within healthcare settings. Stakeholders recognize the potential for PGHD to enhance care delivery and health outcomes, while simultaneously acknowledging substantial organizational and technical barriers to more widespread adoption. The barriers identified by stakeholders align with and further elaborate on those found in other work, including West et al, who identified barriers related to data quality and utility, the alignment of patient and provider goals, and ensuring data is clinically useful and interpretable (11). Barriers to PGHD integration point to significant gaps in current knowledge about how PGHD can best be employed in the service of healthcare delivery. Evidence gaps and areas where future research is warranted to better understand how PGHD advances care transformation for healthcare systems include advancing methodology for interpreting and managing PGHD, assessing how PGHD advances care coordination, evaluating the impact of PGHD integration on workflow and provider efficiency, assessing how PGHD impacts healthcare utilization, and examining the role PGHD plays in supporting patient engagement and patient-centered care. Table 3 enumerates five critical areas for future research, and presents research questions that can guide investigators in expanding the evidence base to support the role of PGHD in healthcare transformation. In addition, continued adoption and growth in the use of PGHD could result in additional unintended consequences, such as changes to how patients seek and access care. Future work is needed to more fully understand the unintended consequences PGHD may present for patient outcomes and healthcare delivery.
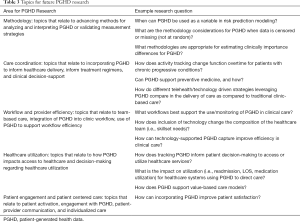
Full table
Conclusions
The results of this study illustrate the value and challenges associated with health systems implementation of PGHD. Increasingly, technology permeates all facets of life including health and wellness. The marketplace for tracking PGHD reflects consumer demand to gain access to tools to better support self-care and engage in care coordination. While not a one-size fits all approach, for some, PGHD may provide an effective way to monitor and manage health outside the healthcare encounter, and is an added tool for communicating health needs with providers. For healthcare providers, PGHD represents the opportunity to better engage patients in care and align data with measurement-based care to inform treatment decisions. For healthcare systems, the promise of PGHD lies in the potential to improve healthcare outcomes at both the individual and population level through better understanding of day-to-day activities, behaviors, and health, leading to more targeted care. Yet more evidence is needed. The ability to incorporate PGHD seamlessly into care remains limited due to lack of standards for integrating disparate forms of data, lack of evidence on effective use of PGHD, and lack of clarity about where PGHD offers the greatest impact in healthcare delivery. Yet the vision of how healthcare is delivered is evolving. The growing recognition of how patients track their health data outside the healthcare encounter creates an imperative for health systems to address the opportunities and challenges presented by PGHD as a tool for improving healthcare delivery. Efforts to increase the scale and spread of PGHD in healthcare transformation will benefit from an implementation approach that addresses both the value, as well at the attendant challenges, PGHD brings to clinical care.
Acknowledgments
The content provided is solely the responsibility of the authors and does not necessarily represent the official views of PCORI, or HHS or any of its agencies.
Funding: The work was supported by a Patient-Centered Outcomes Research Institute (PCORI) Program Award (4322-UOW); and by Funding Opportunity Number CMS-331-44-501 from the U.S. Department of Health & Human Services, Centers for Medicare & Medicaid Services.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The University of Washington Institutional Review Board reviewed this project and granted an exempt determination on 5/31/2017.
References
- US Department of Health & Human Services. Consumer eHealth: Patient-Generated Health Data 2015. Available online: https://www.healthit.gov/policy-researchers-implementers/patient-generated-health-data
- Cohen DJ, Keller SR, Hayes GR, et al. Integrating Patient-Generated Health Data Into Clinical Care Settings or Clinical Decision-Making: Lessons Learned From Project HealthDesign. JMIR Hum Factors 2016;3:e26. [Crossref] [PubMed]
- Chung AE, Basch EM. Potential and challenges of patient-generated health data for high-quality cancer care. J Oncol Pract 2015;11:195-7. [Crossref] [PubMed]
- Watson AJ, Kvedar JC, Rahman B, et al. Diabetes connected health: a pilot study of a patient- and provider-shared glucose monitoring web application. J Diabetes Sci Technol 2009;3:345-52. [Crossref] [PubMed]
- Shapiro M, Johnston D, Wald J, et al. Patient-generated health data: White Paper prepared for the Office of the National Coordinator for Health Information Technology. 2012. Available online: https://www.rti.org/sites/default/files/resources/patientgeneratedhealthdata.pdf
- Chung CF, Cook J, Bales E, et al. More Than Telemonitoring: Health Provider Use and Nonuse of Life-Log Data in Irritable Bowel Syndrome and Weight Management. J Med Internet Res 2015;17:e203. [Crossref] [PubMed]
- Using Patient-Generated Health Data to Transform Healthcare: Milestone B000061603 Evaluation Report. July 2017. Available online: https://www.pcori.org/research-results/2017/using-patient-generated-health-data-transform-healthcare
- Dedoose Version 7.0.23, web application for managing, analyzing, and presenting qualitative and mixed method research data 2016. Los Angeles, CA: SocioCultural Research Consultants, LLC. Available online: www.dedoose.com
- Scott K, Lewis CC. Using Measurement-Based Care to Enhance Any Treatment. Cogn Behav Pract 2015;22:49-59. [Crossref] [PubMed]
- Chung CF, Dew K, Cole A, et al. Boundary Negotiating Artifacts in Personal Informatics: Patient-Provider Collaboration with Patient-Generated Data. CSCW Conf Comput Support Coop Work 2016;2016:770-86.
- Petersen C, DeMuro P. Legal and regulatory considerations associated with use of patient-generated health data from social media and mobile health (mHealth) devices. Appl Clin Inform 2015;6:16-26. [Crossref] [PubMed]
Cite this article as: Lavallee DC, Lee JR, Austin E, Bloch R, Lawrence SO, McCall D, Munson SA, Nery-Hurwit MB, Amtmann D. mHealth and patient generated health data: stakeholder perspectives on opportunities and barriers for transforming healthcare. mHealth 2020;6:8.