
Facilitators and barriers to incorporating digital technologies into HIV care among cisgender female sex workers living with HIV in South Africa
Introduction
In 2019, there were 8.3 billion mobile phone subscriptions worldwide—greater than the global population (1). In low and middle income countries, the number of subscribers is growing exponentially, and increasingly accessible mobile technologies offer opportunities to easily connect with a large number of patients to provide individual-level support (2). Sending text messages as treatment reminders, calling patient mobile phones to promote behavior change, and using phone applications (apps) to track test results and appointment details can positively impact individual antiretroviral therapy (ART) adherence (3-14).
Marginalized populations face complex, multi-level barriers to accessing, adhering to, and remaining in HIV care (15,16). As a result, more intensive support and tailored interventions are needed to reach HIV viral suppression (17). Female sex workers (FSW) are one marginalized population who are often difficult to engage in care due to the stigma and criminalization of their work (18). Of the 121,000–167,000 women in South Africa estimated to be engaged in sex work, approximately 60% are living with HIV and an estimated 39% are currently on ART (19-23). Models suggest that approximately 20% of new infections among adults in South Africa are acquired by FSW or their clients (24).
To improve the health and quality of life for FSW and prevent HIV onward transmission, adherence to ART among FSW is needed. Documented determinants of ART non-adherence among FSW include alcohol and substance use, dissatisfaction with healthcare facilities and healthcare workers, depression, discrimination and stigmatization, and limited social support (25). The mediators of poor ART uptake, non-adherence, and retention in HIV treatment programs vary across individuals, highlighting the need for patient-responsive and adaptive intervention strategies (26). Individual-level interventions such as motivational messages, monitoring, and behavior change tools used in tailored face-to-face support can be modified for delivery via mobile devices (2). Furthermore, mobile technologies are accessible across time and space, permitting intervention delivery and interaction to capture attention when it is most relevant (2).
An abundance of literature demonstrates that mHealth interventions may improve ART adherence in adult, reproductive-aged populations (27-30). There are existing programs in South Africa and other sub-Saharan African countries utilizing mHealth strategies to engage FSW in HIV prevention treatment; most of whom use text message as the primary mode of delivering mHealth interventions (31-33). However, the appropriateness of delivering HIV-related interventions to FSW via mobile phone and other advanced digital technologies, has not been well studied to date. Thus, the objective of this qualitative study was to identify potential facilitators and barriers faced by cisgender FSW living with HIV in South Africa in using mobile phone and other advanced digital interventions for HIV care.
Methods
Study setting
This qualitative study was embedded in the Siyaphambili trial in Durban, South Africa (26). Recruitment of FSW participants was led by FSW peers employed at TB HIV Care, a non-governmental organization offering free HIV care and treatment to FSW in the eThekwini (Durban) metropolitan municipality. Participants were recruited at the TB HIV Care drop-in centers and sex work venues. For context, to-date we note that 63.5% (n=395/622) of the participants randomized into the trial reported phone ownership at enrollment.
Study participants
Women were eligible for the qualitative study if they had been randomized into and actively engaged in the Siyaphambili trial. To be eligible for randomization into the trial, cisgender women over 18 years of age had to be living with HIV, diagnosed at least six months prior, be ART-naive or on first line ART initiated at least two months prior, be non-virally suppressed as defined by South African standard of Care (≥50 copies/mL), selling sex as their main source of income, and not pregnant at enrollment (26). Sex work was defined as exchanging sex for money or goods as their main source of income, following TB HIV Care’s programmatic definition. We used maximum variation sampling to include FSW of varying age groups, educational levels, income levels, operating sites, and current relationship status, with aims to generate findings that are applicable to different FSW groups and individuals (34).
Data collection
Focus group discussions (FGDs) were conducted using a semi-structured interview guide developed in English, translated into isiZulu, and reviewed by FSW peers. The guide was focused on barriers and facilitators to receiving digital health interventions. The guides probed around mobile phone ownership and access as well as mobile phone use generally and for HIV care and treatment support. The guide also explored perceptions on the use of more advanced digital technologies, including biometrics as tools for identification, mobile phone apps, and chatbots. To ensure consistent understanding of chatbots for all participants, the iPhone Siri was demonstrated at each FGD as an example. A female research assistant with >15 years of qualitative experience led the FGDs. The first author (WX You), a behavioral scientist with content knowledge in technological innovations, supported the research assistant with logistics during the FGDs. FGDs occurred in a private space at the TB HIV Care drop-in center, were conducted in isiZulu and audio-recorded. Each FGD ranged from 60–90 minutes. FGDs continued until similar themes about facilitators and barriers around mobile phone use and advanced digital technologies emerged. Four FGDs were ultimately conducted.
All participants provided written informed consent prior to participation. Precautions taken to address participants’ anonymity were included in the consent form and risks were communicated with participants during the consenting process. This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board and the University of the Western Cape Biomedical Research Ethics Committee. Reimbursement was provided to participants to account for their time and the cost of transportation (100ZAR=$7 USD).
Data analysis
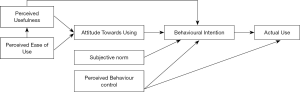
Our analysis is guided by a combination of the Technology Acceptance Model and Theory of Planned Behavior (C-TAM-TMB) (35). This model was chosen due to its flexibility in examining both old and new digital technologies and accommodating both experienced and inexperienced users. Factors that support and hinder the uptake and engagement in digital interventions are explored to shape HIV treatment and care intervention and program development. Further details on our application of this framework can be found in the supplementary materials.
Audio-recordings were transcribed verbatim and translated into English. Transcripts were inductively coded using thematic analysis. First, WXY identified emerging themes through iterative, open coding, and developed a codebook based on emergent themes. The codebook was reviewed and updated based on transcript reviews and consensus from WXY, CAC, and BAJ. Repeated reading, discussion, and coding was conducted by WXY and BAJ in Atlas.ti version 8 (36). After independently double-coding all transcripts, WXY and BAJ convened, resolved discrepancies, and agreed upon final coding. Themes presented were consistent across transcripts, and final selection of representative quotations was an iterative process by WXY, BAJ, CAC, and SS.
Results
Twenty-two black FSW participated in the FGDs and varied in their demographics, including age, education, income, ART status and relationship status (Table 1). The majority (82%, n=18) of participants owned a mobile phone.
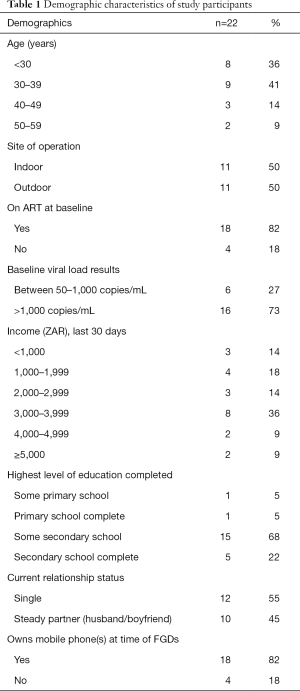
Full table
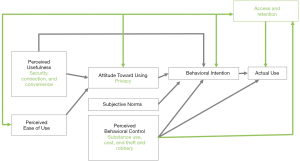
A modified C-TAM-TPB model, adapted to the findings, is presented in Figure 1. Primary themes included both facilitators and barriers to incorporating mobile phones into HIV care (Table 2), and facilitators and barriers to utilization of other advanced digital technologies within HIV care (Table 3). Sub-themes are described in detail below and outlined alongside additional supportive quotes in Tables 2 and 3.

Full table
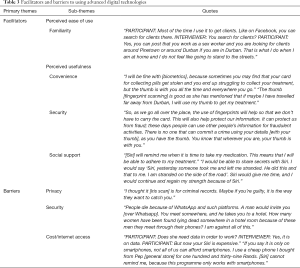
Full table
Mobile phones for HIV care: facilitators
FSW expressed positive attitudes and a willingness to use mobile phones to engage in HIV care. Patterns of ownership varied and were reflected in participant attitudes toward the utility of mobile phones, behavioral intentions for phone use and perceived ability to retain a mobile phone (Figure 1). Mobile phone ownership as well as the type of mobile phone owned (i.e., a smart or feature phone) depended first on participants’ individual stability and current life situation and then, preference, and utility. Though some participants indicated using one phone for her family and boyfriend and another phone for her clients, other participants owned a single phone for all uses.
Among participants who did not currently or consistently have a mobile phone, FSW reported sharing mobile phones with their peers, friends, boyfriends, and family members. Some participants indicated that they shared or borrowed a physical phone while others used the phone number of another person, who then passed on messages to the participant. FSW valued reliability as a key characteristic when considering with which person to share a phone.
“That’s why I give people the number of someone that I am certain will always be available to answer.”
Most participants reported moving frequently between cities and locations within cities (i.e., sex work venues) and highlighted the importance of having a phone to stay connected with friends, family, and clients. Mobile phone ownership and use among FSW also emerged as a desired security measure. When necessary and in reference to troublesome clients or law enforcement, mobile phones provide a tool for FSW to account and look out for one another’s safety.
Mobile phones for HIV care: barriers
Lack of continuous mobile phone or phone number retention due to financial instability, substance use, and theft emerged as key barriers to using mobile phones for HIV care among FSW. Collectively, these barriers negatively impacted FSW’s perceived behavioral control surrounding mobile phone use (Figure 1).
In addition to frequent cycling of a single physical phone, FSW expressed failing to retain the same subscriber identity module (SIM) card over time and hence, phone number.
“I will not lie, most of us [keep our phones for] one week or two weeks.”
Inconsistent ownership or access was often a product of immediate needs, substance use and theft. FSW reported frequent selling or pawning mobile phones for cash to meet their basic needs. FSW also reported personally selling or trading mobile phones for substances, including alcohol and drugs. Moreover, conducting sex work under the influence emerged as increasing the risk that FSW would lose their phones or have them stolen. FSW also reported having clients or FSW peers steal their phone, even when not under the influence of drugs or alcohol. Participants’ perceived risk of losing their mobile phones both influenced FSWs’ intentions to own specific types of mobile phones and overall mobile phone use.
Advanced technologies for HIV care: facilitators
Facilitators of using advanced technologies for HIV care included familiarity with the technologies and perceptions that these advanced technologies would offer convenience, security, and social support.
Participant familiarity with advanced technologies (e.g., biometrics, social media, messaging apps and chatbots) varied among participants and influenced their perceived ease of using advanced technologies. Participants most commonly expressed knowledge of social media apps and search engines. A few reported utilizing apps like Facebook and WhatsApp tools to support their sex work and expressed greater perceived ease of use (Figure 1). No participant had previously used biometrics for identification prior to study participation nor had interacted with a chatbot.
Participants perceived biometric identification tools useful for their convenience and ability to offer security. Specifically, participants imagined a use case where biometric identification was introduced alongside a national electronic medical record system, hence eliminating the need for clinics to ask FSW for clinic cards or other means of identification before dispensing ART. Participants noted that while clinic or identification cards can be lost, inaccessible, manufactured or falsified, biometric identification is more specific and difficult to forge. Participants felt that biometric identification would ensure ART could only be received by the participant herself, preventing fraudulent ART pick-ups.
Preferences and concerns around the types of biometric tools varied. Some participants did not prefer fingerprint scanning due to their long nails. Others worried voice recognition would not consistently work with a voice deepened after drinking.
Social media tools were also cited as back up measures to stay connected within their network, especially if mobile phones are lost, stolen, or sold. After seeing the various capabilities of Siri, participants also imagined scenarios where chatbots might act as a tool to protect themselves in case of an emergency, like kidnapping.
“WXY: “[Siri] is a voice communication system. Siri, where am I right now?”
Siri: “You are at [address].”
PARTICIPANT: “Wow, I am lost for words.”
INTERVIEWER: “How would Siri be of assistance to you?”
PARTICIPANT: “[Siri] could help if a client kidnapped me, blindfolded me, and I am in an unknown area. If I manage to free myself and do not know where I am, I would check my location [with Siri] and let them know where to find me.”
Participants also imagined that chatbots like Siri could provide various types of social support. For instance, participants imagined chatbots providing informational social support and improving ART adherence by providing reminders about clinic appointments and daily medication reminders. Additionally, participants imagined Siri as being useful as an emotional social support tool, highlighting the possibility of Siri listening and offering a feeling of being understood.
“When I leave the clinic and I am told that my next visit will be on a certain day, I could easily just ask Siri to remind me. We want Siri. If that’s how this program works, then it is really good.”
Advanced technologies for HIV care: barriers
Initial concerns about privacy emerged regarding fingerprint and iris scanning, because these are also used by the police to track people who commit crimes. However, after explaining the system linkages needed to connect the medical and criminal justice databases, participants expressed less apprehension. Other privacy concerns emerged based on participants’ personal experiences, the experiences of other FSW, and fearing potentially negative outcomes. One participant specifically expressed that a Google Maps location image included her standing outside of the sex work venue.
“Yes. When you browse [street name] on Google Maps, it shows you the car parked there. I would appear standing there as well. The lounge [sex work venue] as it is, and it will even reveal you sitting there on the side of the road with your legs wide open. [Google Maps] will show you in whatever clothes you are wearing.”
Security and cost emerged as other salient concerns around advanced technology use. For example, using messaging apps like WhatsApp to find clients was perceived as potentially dangerous. Furthermore, many advanced technologies require smartphones and internet access, which have associated costs and access issues that were identified as a barrier.
Discussion
This study explored the perceived usefulness, perceived ease of use, attitudes towards and control over digital health technologies for engagement in HIV treatment support. While most FSW are motivated to own or have access to a mobile phone, nearly all FSW expressed difficulty retaining phones and phone numbers as a result of financial instability, substance use, and theft. When discussing advanced technologies such as biometrics, apps, and chatbots, FSW showed interest because of their potential to provide convenience, security, and social support. However, FSW also expressed that privacy and cost would be barriers to use. Given that preferences and opinions of technology varied by individual, integrating technology into HIV care will require more patient-centered, tailored approaches for FSW.
FSW described currently using mobile phones frequently to remain safe and connected; future interventions should leverage perceived utility of the technology to offer social and clinical support to FSW via phone. Given the highly stigmatized nature of sex work and that digital interactions can be anonymous, immediate, and tailored, mHealth interventions may effectively supplement in-person healthcare venues for FSW (37-40). Previous research demonstrates that people may even be more willing to disclose personal information via phone than in-person (41). mHealth tools have also made it possible for researchers to engage previously unreachable members of marginalized populations by easing the burden of participating, as in the LITE study with the transgender community (42). Providing data via a mobile phone may also be more acceptable than clinician-led, in-person interviews, since some key populations living with HIV often face discrimination from physicians and nurses in South Africa (40).
Despite these opportunities, FSW described difficulties consistently retaining their mobile phone and phone number, which will require creative solutions for FSW to benefit from digital HIV care. FSW know how to perform SIM swaps to maintain their phone number while changing phones, but were unmotivated to do so. Given that SIM cards are relatively inexpensive, FSW could be provided multiple SIM cards or new SIM cards, as needed, at in-person clinical or research visits. Alternately, phone numbers could be collected anew from engaged FSW at each in-person visit. FSW stated that they notified certain people when getting a new phone number; researchers and clinicians could also request and provide incentives to be notified whenever FSW change their contact information. However, this would need to be balanced against motivating FSW to provide false change in contacts to acquire incentives such as airtime credit. Additionally, many FSW described at least one key peer who was “reliable” and consistently maintained a single phone number over time. In lieu of delivering tailored messaging to each FSW, future mHealth interventions could deliver generic health information to key, consenting FSW peer champions who could then share that information with her peers (43). Future research should explore whether social media or other accounts (e.g., Facebook, WhatsApp) independent of a phone number would be an acceptable way to maintain contact with FSW as their phone numbers change.
Participants described other FSW-specific HIV care use cases for advanced technologies like biometric identification, social media, and chatbots. To aid in addressing FSW mobility and the impact on treatment interruptions (44,45), replacing clinic cards with biometric identification at least within sex work-supported services would better accommodate FSW, who may have their cards stolen and are highly mobile while traveling between clients. It should be noted, however, that a national electronic medical record system would be necessary for biometric identification tools to work across clinics. Beyond biometrics, FSW described how social media connected them with other FSW and clients beyond text messaging. In one study with FSWs in Zimbabwe, a messaging app successfully supplemented in-person group therapy (46). Finally, FSW described how chatbots may offer adherence support and emotional support by “listening” to FSW. Chatbots are increasingly being used to address adherence and mental health issues (47), including preliminary research around the use of chatbots for HIV and mental health in low and middle income countries (29,48). Chatbots are particularly promising for FSW and other stigmatized populations because of their focus on users, nonjudgment, and ability to help users cognitively reappraise negative experiences (49).
FSW heavily emphasized potential risks about privacy when receiving digital interventions. FSW are criminalized globally, and thus, privacy in many ways equals safety (50-53). Many FSW in this and other studies compartmentalize their work from their personal lives by using separate phones for each; others only share their phones with trusted friends and family members (54). To avoid undesired disclosures about their work or HIV status, future interventions via mobile phone, social media, or chatbots may need to use coded language or have password protection to access certain apps or sections of apps, in line with other successfully implemented HIV strategies (55-57). There may also be unintended consequences such as inadvertent disclosure or poor intervention uptake among those sharing a phone. Clear messaging around the purpose of the technology will be necessary before engaging FSW in digital interventions.
Despite the promise of digital interventions, these data suggest that, at this stage, digital support for HIV care alone will be insufficient for many FSW, and multi-component interventions including in-person strategies are likely to be the most effective. Until phones and other technologies are affordable and retainable for most FSW, HIV programmatic and research activities implemented digitally are likely to underrepresent those most vulnerable.
Technology should complement but not replace personalized, in-person care. For FSW specifically, formative research from the Siyaphambili trial demonstrated that knowing and visiting FSW at their place of work were perceived as critical for long-term engagement (58). FSW also reported that clinic and research staff should know their technology usage preferences (e.g., text vs. call, timing, type of staff member) to best leverage phones as part of HIV care (58).
Several limitations should be considered when evaluating the results of this study. This qualitative study was conducted prior to the holiday seasons, where large numbers of people migrate within the country. This movement of populations may have potentially affected the overall diversity of participants and reduced the overall numbers of women who engaged in the FGDs. Moreover, although the findings apply to FSW in Durban, they are not expected to be generalizable across settings. Generalizability is, however, rarely the intention of qualitative data collection. Participants benefited from being familiar with iris scanning biometrics through the Siyaphambili trial, but discussion around other biometric data collection tools, social media platforms or artificial intelligence technologies would likely have been hypothetical for some participants as not all participants had experience engaging with each of these digital technologies.
Conclusions
FSWs were receptive to digital technologies for HIV care and beyond, but they also described many barriers. Future work must strongly consider digital privacy and ensure that the most vulnerable are not systematically excluded from programming and research requiring technology. There is an inherent tension between the benefits of anonymous, general messages that enhance privacy should phones be shared or seen by clients or family, and personalized efforts to foster greater social support. At this point, digital tools such as mobile phones, biometric identification, mobile apps, and chatbots should only supplement but not replace in-person HIV research and care for FSW in South Africa. While there is extraordinary potential for healthcare interventions leveraging technology among FSW, substantial barriers remain and the views, opinions, and participation of FSW must be primary throughout the design and implementation.
Supplementary
Conceptual model combined technology acceptance model and theory of planned behavior model (C-TAM-TPB)
One aim of the Siyaphambili study is to explore opportunities in using digital health technologies to improve HIV treatment adherence and retention in care for FSW. To scale up utilization of digital health interventions, there is need for user-centered evaluation to understand the usage behaviors. Specific to this study, what makes FSW use or not use digital health technologies.
Theory of reasoned action (TRA), proposed by Fishbein and Ajzen, posits attitudes toward behavior and subjective norms affect one’s behavioral intention (59). It gained widespread acceptance in technology acceptance research; many studies have demonstrated this theory to be useful in predicting and explaining behaviors of technology use (60,61). Theory of planned behavior (TPB) (Figure S1), as an extension of TRA, introduced perceived behavior control as the third construct that affects one’s behavioral intention (62). Perceived behavior control is determined by the availability of skills, resources, and opportunities, as well as the perceived importance of those skills, resources, and opportunities (63). When the barriers to using digital health seem too high, the user’s intention to use it may reduce, hence decreasing the chance of actually using digital health.
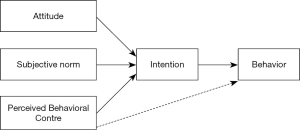
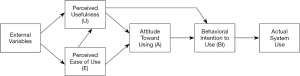
The technology acceptance model (TAM) (Figure S2) is a model researchers have been using to predict acceptance and use of a new system. TAM suggests that perceived usefulness and perceived ease of use are the determinants of users’ behavioral intention to use technology, with the intention to use serving as a mediator of actual usage (61). Similar approaches can be used to evaluate acceptance and use of novel digital health in low-resource settings (64).
This qualitative sub-study drew heavily from the C-TAM-TPB model (Figure S3), shown below, which is a combined model of the Technology Acceptance Model and Theory of Planned Behavior (35). While some FSW may have more experience with digital health technologies and familiar with their functionalities and usefulness, others may have little exposure to digital health. This model was chosen due to its flexibility in examining both old and new digital health technologies, and also because it accommodates both experienced and inexperienced users. The C-TAM-TPB was used to inform the analysis and interpretation of the results.
Acknowledgments
We are grateful to the Centers for Disease Control and Prevention for their support of the TB HIV Care sex work program. Finally, we express appreciation to all the participants who took part in the study.
Funding: This work was supported by the National Institute of Nursing Research of the National Institutes of Health (Award Number R01NR016650), as well as through support from the Johns Hopkins University Center for AIDS Research through the National Institutes of Health (Award Number P30AI094189). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Johns Hopkins CFAR. The study sponsor was not involved in the design of the study; the collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures were approved by the University of the Western Cape Biomedical Research Ethics Committee and the JHSPH institutional review board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Union IT. ITU Statistics. 2018.
- Free C, Phillips G, Galli L, et al. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Med 2013;10:e1001362. [Crossref] [PubMed]
- Moore DJ, Poquette A, Casaletto KB, et al. Individualized texting for adherence building (iTAB): improving antiretroviral dose timing among HIV-infected persons with co-occurring bipolar disorder. AIDS Behav 2015;19:459-71. [Crossref] [PubMed]
- Sabin LL, DeSilva MB, Gill CJ, et al. Improving adherence to antiretroviral therapy with triggered real time text message reminders: the China through technology study (CATS). J Acquired Immune Deficiency Syndromes (1999) 2015;69:551.
- Dowshen N, Kuhns LM, Johnson A, et al. Improving adherence to antiretroviral therapy for youth living with HIV/AIDS: a pilot study using personalized, interactive, daily text message reminders. J Med Internet Res 2012;14:e51. [Crossref] [PubMed]
- Hailey JH, Arscott J. Using technology to effectively engage adolescents and young adults into care: STAR TRACK Adherence Program. J Assoc Nurses AIDS Care 2013;24:582-6. [Crossref] [PubMed]
- Lewis MA, Uhrig JD, Bann CM, et al. Tailored text messaging intervention for HIV adherence: A proof-of-concept study. Health Psychol 2013;32:248. [Crossref] [PubMed]
- Perera AI, Thomas MG, Moore JO, et al. Effect of a smartphone application incorporating personalized health-related imagery on adherence to antiretroviral therapy: a randomized clinical trial. AIDS Patient Care STDs 2014;28:579-86. [Crossref] [PubMed]
- Swendeman D, Jana S, Ray P, et al. Development and pilot testing of daily interactive voice response (IVR) calls to support antiretroviral adherence in India: a mixed-methods pilot study. AIDS Behav 2015;19:142-55. [Crossref] [PubMed]
- da Costa TM, Barbosa BJP, Costa DAG, et al. Results of a randomized controlled trial to assess the effects of a mobile SMS-based intervention on treatment adherence in HIV/AIDS-infected Brazilian women and impressions and satisfaction with respect to incoming messages. Int J Med Inform 2012;81:257-69. [Crossref] [PubMed]
- Huang D, Sangthong R, McNeil E, et al. Effects of a phone call intervention to promote adherence to antiretroviral therapy and quality of life of HIV/AIDS patients in Baoshan, China: a randomized controlled trial. AIDS Res Treat 2013;2013:580974. [Crossref] [PubMed]
- Vidrine DJ, Marks RM, Arduino RC, et al. Efficacy of cell phone–delivered smoking cessation counseling for persons living with HIV/AIDS: 3-month outcomes. Nicotine Tob Res 2012;14:106-10. [Crossref] [PubMed]
- Luque AE, Corales R, Fowler RJ, et al. Bridging the digital divide in HIV care: a pilot study of an iPod personal health record. J Int Association Providers AIDS Care 2013;12:117-21. (JIAPAC). [Crossref] [PubMed]
- Swendeman D, Ramanathan N, Baetscher L, et al. Smartphone self-monitoring to support self-management among people living with HIV: Perceived benefits and theory of change from a mixed-methods, randomized pilot study. J Acquired Immune Deficiency Syndromes (1999) 2015;69:S80.
- Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS 2012;26:2059-67. [Crossref] [PubMed]
- Deblonde J, De Koker P, Hamers FF, et al. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health 2010;20:422-32. [Crossref] [PubMed]
- Mishra S, Mountain E, Pickles M, et al. Exploring the population-level impact of antiretroviral treatment: the influence of baseline intervention context. AIDS 2014;28:S61-72. [Crossref] [PubMed]
- Ma PH, Chan ZC, Loke AY. The socio-ecological model approach to understanding barriers and facilitators to the accessing of health services by sex workers: a systematic review. AIDS Behav 2017;21:2412-38. [Crossref] [PubMed]
- Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 2012;12:538-49. [Crossref] [PubMed]
- Mishra S, Pickles M, Blanchard JF, et al. Distinguishing sources of HIV transmission from the distribution of newly acquired HIV infections: why is it important for HIV prevention planning? Sex Transm Infect 2014;90:19-25. [Crossref] [PubMed]
- Shannon K, Strathdee SA, Goldenberg SM, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet 2015;385:55-71. [Crossref] [PubMed]
- Education SW, Taskforce A. Sex workers in South Africa: a rapid population size estimation study. 2013.
- Schwartz S, Lambert A, Phaswana-Mafuya N, et al. Engagement in the HIV care cascade and barriers to antiretroviral therapy uptake among female sex workers in Port Elizabeth, South Africa: findings from a respondent-driven sampling study. Sex Transm Infect 2017;93:290-6. [Crossref] [PubMed]
- Council SANA. National Strategic Plan on HIV, STIs and TB, 2012-2016. South African National AIDS Council; 2012.
- Heestermans T, Browne JL, Aitken SC, et al. Determinants of adherence to antiretroviral therapy among HIV-positive adults in sub-Saharan Africa: a systematic review. BMJ Global Health 2016;1:e000125. [Crossref] [PubMed]
- Comins CA, Schwartz SR, Phetlhu DR, et al. Siyaphambili protocol: An evaluation of randomized, nurse-led adaptive HIV treatment interventions for cisgender female sex workers living with HIV in Durban, South Africa. Res Nurs Health 2019;42:107-18. [Crossref] [PubMed]
- Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S. Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 2014;14:188. [Crossref] [PubMed]
- Marcolino MS, Oliveira JAQ, D'Agostino M, et al. The impact of mHealth interventions: systematic review of systematic reviews. JMIR mHealth uHealth 2018;6:e23. [Crossref] [PubMed]
- Green EP, Pearson N, Rajasekharan S, et al. Expanding Access to Depression Treatment in Kenya Through Automated Psychological Support: Protocol for a Single-Case Experimental Design Pilot Study. JMIR Res Protoc 2019;8:e11800. [Crossref] [PubMed]
- Nachega JB, Skinner D, Jennings L, et al. Acceptability and feasibility of mHealth and community-based directly observed antiretroviral therapy to prevent mother-to-child HIV transmission in South African pregnant women under Option B+: an exploratory study. Patient Preference Adherence 2016;10:683. [Crossref] [PubMed]
- Laar A, Sutherland E, Ankomah A, et al. A Performance Evaluation of the National HIV Prevention Program for FSW and MSM in Ghana.
- Forrest JI, Wiens M, Kanters S, et al. Mobile health applications for HIV prevention and care in Africa. Curr Opin HIV AIDS 2015;10:464-71. [Crossref] [PubMed]
- Prata N, Morris N, Agbovi KK, et al. Does time matter? Cross–sectional evaluation of mhealth program enrollment duration on healthy behaviors among key populations in Lomé. MOJ Public Health 2019;8:172-80.
- Patton MQ. Qualitative evaluation and research methods. SAGE Publications, Inc.; 1990.
- Taylor S, Todd PA. Understanding information technology usage: A test of competing models. Information Systems Res 1995;6:144-76. [Crossref]
- DevelopmentGmbH AtSS. Atlas.ti. 8.3.2 ed. Berlin, Germany2019.
- Free C, Whittaker R, Knight R, et al. Txt2stop: a pilot randomised controlled trial of mobile phone-based smoking cessation support. Tobacco Control 2009;18:88-91. [Crossref] [PubMed]
- Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tobacco Control 2005;14:255-61. [Crossref] [PubMed]
- Walther JB, Boyd S. Attraction to computer-mediated social support. Communication technology and society: Audience Adoption Uses 2002;153188.
- Duby Z, Nkosi B, Scheibe A, et al. ‘Scared of going to the clinic’: Contextualising healthcare access for men who have sex with men, female sex workers and people who use drugs in two South African cities. Southern African J HIV Med 2018.19.
- Sundar SS, Kim J, editors. Machine Heuristic: When We Trust Computers More than Humans with Our Personal Information. Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems; 2019: ACM.
- Wirtz AL, Cooney EE, Chaudhry A, et al. Computer-Mediated Communication to Facilitate Synchronous Online Focus Group Discussions: Feasibility Study for Qualitative HIV Research Among Transgender Women Across the United States. J Med Internet Res 2019;21:e12569. [PubMed]
- Simoni JM, Nelson KM, Franks JC, et al. Are peer interventions for HIV efficacious? A systematic review. AIDS Behav 2011;15:1589-95. [Crossref] [PubMed]
- Richter M, Chersich MF, Vearey J, et al. Migration status, work conditions and health utilization of female sex workers in three South African cities. J Immigr Minor Health 2014;16:7-17. [Crossref] [PubMed]
- Davey C, Cowan F, Hargreaves J. The effect of mobility on HIV-related healthcare access and use for female sex workers: A systematic review. Social Science Medicine 2018;211:261-73. [Crossref] [PubMed]
- Mutevedzi F, Takawira D, Jani C, et al. Empowering female sex workers (FSW) through self help groups (SHG) - A pilot programme in Harare Zimbabwe. AIDSImpact; London 2019.
- Laranjo L, Dunn AG, Tong HL, et al. Conversational agents in healthcare: a systematic review. J Am Med Inform Assoc 2018;25:1248-58. [Crossref] [PubMed]
- van Heerden A, Ntinga X, Vilakazi K, editors. The potential of conversational agents to provide a rapid HIV counseling and testing services. 2017 international conference on the frontiers and advances in data science (FADS); 2017: IEEE.
- Caplan SE, Turner JS. Bringing theory to research on computer-mediated comforting communication. Computers Human Behavior 2007;23:985-98. [Crossref]
- Shannon K, Crago AL, Baral SD, et al. The global response and unmet actions for HIV and sex workers. Lancet 2018;392:698-710. [Crossref] [PubMed]
- Reid MJ, Dhar SI, Cary M, et al. Opinions and attitudes of participants in a randomized controlled trial examining the efficacy of SMS reminders to enhance antiretroviral adherence: a cross-sectional survey. J Acquir Immune Defic Syndr 2014;65:e86-8. [Crossref] [PubMed]
- Hasin DS, Aharonovich E, Greenstein E. HealthCall for the smartphone: technology enhancement of brief intervention in HIV alcohol dependent patients. Addict Sci Clin Pract 2014;9:5. [Crossref] [PubMed]
- Sidney K, Antony J, Rodrigues R, et al. Supporting patient adherence to antiretrovirals using mobile phone reminders: patient responses from South India. AIDS Care 2012;24:612-7. [Crossref] [PubMed]
- Sambasivan N, Weber J, Cutrell E, editors. Designing a phone broadcasting system for urban sex workers in India. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; 2011: ACM.
- Maraba N, Hoffmann CJ, Chihota VN, et al. Using mHealth to improve tuberculosis case identification and treatment initiation in South Africa: Results from a pilot study. PLoS One 2018;13:e0199687. [Crossref] [PubMed]
- Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet 2010;376:1838-45. [Crossref] [PubMed]
- Jarrett B, DiAndreth L, Elf J, et al. The effects of securely sending HIV-related and tuberculosis laboratory results to patient cell phones: a pilot comparative study. Union World Conference on Lung Health; Hyderabad, India 2019.
- Comins C, Parmley L, Schwartz S, et al. Multi-level barriers to antiretroviral therapy initiation, retention, and adherence for female sex workers living with HIV in South Africa. Journal of the International AIDS Society 2018.
- Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. MA: Addison-Wesley, 1975.
- Davis FD. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly 1989;13:319-40. [Crossref]
- Davis FD, Bagozzi RP, Warshaw PR. User acceptance of computer technology: a comparison of two theoretical models. Management Science 1989;35:982-1003. [Crossref]
- Ajzen I. Attitudes, Personality, and Behavior. Milton Keynes: Open University Press. 1988.
- Kripanont N. Examining a Technology Acceptance Model of Internet Usage by Academics within Thai Business Schools. Victoria University (Accessed 6 Jan 2008). 2007.
- Mburu S, Oboko R. A model for predicting utilization of mHealth interventions in lowresource settings: case of maternal and newborn care in Kenya. BMC Medical Informatics and Decision Making 2018;18:67. [Crossref] [PubMed]
Cite this article as: You WX, Comins CA, Jarrett BA, Young K, Guddera V, Phetlhu DR, Mulumba N, Mcingana M, Hausler H, Baral S, Schwartz S. Facilitators and barriers to incorporating digital technologies into HIV care among cisgender female sex workers living with HIV in South Africa. mHealth 2020;6:15.


