Chat-based hotlines for health promotion: a systematic review
Introduction
Traditional hotlines connect callers to service centers via phone call (1,2). Hotlines typically operate 24 hours a day and are commonly used for services such as crime tips, suicide crisis, and support for sexual assault and rape victims, bullying victims, runaway children, and human trafficking victims (1,2). Hotlines have been used for over half a century and were initially created to connect individuals in crisis to live, confidential and anonymous support services outside of normal business hours (2,3). The emergence of hotlines was a crucial step in connecting individuals to services in situations where getting access to in-person services was not possible due to distance, availability of providers, experiences of stigma and shame, the need for confidentiality or the timing of the crisis (1,2). Hotlines have now expanded into additional fields such as health promotion including support to quit smoking or curb other addictions and new modes of communication including instant messaging and app-based chatting (4).
Chat-based hotlines use online messaging services or popular chat applications such as WhatsApp, Facebook Messenger, and WeChat, to connect users to trained health providers or staff (5). Chat-based hotlines have unique features that make them more attractive for some users. Chatting does not require users to find a private, sound-proof space to discuss private topics; users can be on the bus or at a public library computer. When chatting, users can control the pace of the conversations and discuss things that they may be hesitant to say aloud (6). Today, chat-based hotlines are being used worldwide for such health topics as rape crisis response in the US (6), HIV treatment retention in Peru (7) and remote health services in Malawi (8).
Individual studies evaluating the effectiveness of chat-based hotlines for health promotion demonstrate the growing prevalence of this mode of support. In the Netherlands, children experiencing anxiety and depression who accessed a confidential one-on-one online chat service experienced a higher sense of well-being and a reduced severity of their problems (9). Data from an evaluation of the US National Sexual Assault Online Hotline found that the chat-based hotlines reached more survivors than their call-in line due to the increased anonymity (10). Other studies have found chat-based hotlines to be an effective way to provide sexual and reproductive health advice in the US (11), provide addiction support for alcohol misuse in Hong Kong (12) and provide emotional support for colostomy patients in China (13).
The evidence for chat-based hotlines for health promotion has not been reviewed systematically. This review will assess the existing global evidence on the efficacy of chat-based hotlines for health promotion.
We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/mhealth-2019-di-13).
Methods
The protocol of this review was registered with Prospero International Register for Systematic Reviews (ID: CRD42020156670).
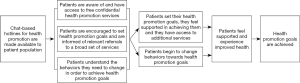
Theory of change
The theory of change guiding chat-based health promotion hotlines for a specific patient population is as follows. If patients have access to free confidential health promotion chat-based services offered during and outside of business hours, they will use those services to set health promotion goals (i.e., quit smoking, adhere to HIV medication, heal after sexual assault) and get support to start or stop the behaviors they need to change in order to achieve those goals. If they use the services, they will feel supported in achieving those goals and will be able to change their behavior. Then, patients will feel supported and experience improved health which will lead to their health promotion goals being achieved (see Figure 1).
Search terms
The following search terms were used in combination to search the literature: “chat-based”, “facebook messenger”, “WhatsApp”, “weChat”, “instant messenger”, “online hotline”, “real-time”, “mobile instant messaging (MIM)”, “online chat”, “Chat”, “health”.
For example, the PubMed search strategy was as follows: (("health"[MeSH Terms] OR "health"[All Fields]) OR "health s"[All Fields]) OR "healthful"[All Fields]) OR "healthfulness"[All Fields]) OR "healths"[All Fields]) AND "chat-based"[All Fields]) OR "facebook messenger"[All Fields]) OR "WhatsApp"[All Fields]) OR "weChat"[All Fields]) OR "instant messenger"[All Fields]) OR "online hotline"[All Fields]) OR "online chat"[All Fields]) OR "Chat"[All Fields].
The literature search occurred in two phases:
❖ Phase 1: we searched the following electronic databases: (I) PubMed; (II) Cochrane Database; (III) Google Scholar;
❖ Phase 2: researchers used the bibliographic back referencing technique. Two researchers reviewed reference lists of included studies and studies that had cited the included studies for additional studies.
We also conducted a supplemental keyword search in google.com based on leads generated by the search described above. For example, if a search identified an article mentioning (but not evaluating) a chat-based hotlines for smoking cessation for key populations through an NGO called iQuit, a search of google.com and google.scholar using the term “iQuit” and several related keywords such as “health” or “chat-based hotline” was conducted to determine whether there was any additional information on the program that might have included evaluation information relevant to the analysis.
Titles and abstracts of search hits were read and excluded when obviously irrelevant. Duplicate references were also excluded. Disagreements about inclusion at this stage were resolved through discussion. If no agreement could be reached, a third independent member of the team was brought in to resolve the disagreement.
Any study identify during this phase were determined to be eligible for full-text review and were then read by two researchers and evaluated based on the below inclusion and exclusion criteria. Researchers who were blinded to each other’s decisions and discrepancies were decided through discussion mediated by a third party. The first time inter-rate reliability rate between the two blinded researchers was 85%.
Inclusion criteria
Participants
We included studies of chat-based hotlines where users engaged in one-on-one interactions with healthcare providers, trained staff or trained volunteers.
Type of chat-based hotline
we included studies of chat-based hotline where clients or patients have access to live/real-time chatting during extended hours outside of business hours up to 24 h. We included studies of chat-based hotlines that use text messages, a mobile instant message application (Facebook messenger, weChat and WhatsApp) or a live chatting feature through a website.
Study types
We included all trial protocols, pilot studies, observational, quasi-experimental and experimental quantitative evaluations as long as there is a documented and pre-determined methodology guiding the evaluation.
Outcomes
We included any outcomes that measured the reach of the chat-based hotline such as characteristics of users, utilization data, utilization of referral services and satisfaction by participants as well as effectiveness of the chat-based hotline through measures such as participants’ knowledge, attitude, behavior or health outcomes. We also looked for cost-effectiveness outcomes such as the incremental cost-effectiveness ratio.
Time period
We included articles published since 2009 when WhatsApp was initially released (Facebook messenger and weChat were released in 2011 and 2010 respectively).
Exclusion criteria
Participants
We excluded studies about chat-based hotlines that connected two or more staff member such as between supervisors and staff. We also excluded studies about group chat-based hotlines (i.e., a chat room or group chats).
Type of intervention
We excluded studies of chat-based hotlines that required clients or patients to make appointment for chatting or could only chat during certain time periods. We excluded those that examined one-way chat-based hotlines that only provided health education messages or reminders; and we excluded those that used artificial intelligence or chatbots. We excluded chat-based hotlines that used text messages or emails that did not have a live person ready to provide an immediate response.
Study design
We excluded case studies, qualitative studies and modeling analyses.
Outcomes
We excluded outcomes on staff experiences running the chat-based hotline.
Time period
We excluded articles published before 2009.
Data collection process
Those studies included at this stage underwent a data extract process guided by an electronic data extraction form created using the Google form application. Data was entered into the form which then populated a table with all study details including: author, year of publication, health promotion activity, chat-based hotline details, study population, study location, study type, outcome categories, outcome measures and effects. From this master database, individual tables were then created for study characteristics and the four outcome categories (user characteristics, modes of support, health outcome and user).
Data synthesis
The researchers performed a narrative synthesis that describes the nature, scope and evidence base for chat-based hotlines. Multiple tables are presented in the results section that provide details on the health promotion activity, the type of chat-based hotlines, the population groups, the outcome categories and the effects. If chat-based hotlines were being compared to other types of hotline formats, this was noted and described in the table. The direction of main effect was coded as either positive, negative, or no effect and as either significant or non-significant.
Analysis of outcome categories
We examined four outcomes categories: user characteristics, modes of support, health outcome and user satisfaction based on the data trends from included studies. Summary measures included difference in proportions and means, risk ratios, and odds ratios.
Risk of bias assessment
Two researchers worked independently to assess the rigor of each study using the National Institute of Health Study Quality Assessment Tools specific to the study design (available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). Using these tools, reviewers assigned a quality rating of good, fair or poor to each study. If there was a disagreement between reviewers, it was resolved through discussion. The results of the risk of bias assessment is included in the results section.
Results
A total of 4,406 records were identified in the initial screening process; 151 duplicates were removed and 4,142 records were excluded based on the inclusion and exclusion criteria listed above. The remaining 113 full-text articles were read and assessed for eligibility; 102 articles were removed based on a closer examination of their fit with the inclusion and exclusion criteria and 11 studies were included in the final analysis. Five additional articles were identified through bibliographic back referencing; 4 were excluded and 1 was included in the final analysis. A total of 12 studies were included in the final narrative synthesis for this review. Figure 2 provides the screening and inclusion process for this review.
Study type, health promotion activity, location, chat-based hotline details, program additions, and primary study population per each study are listed in Table 1. Study types included 6 cross-sectional (10,14-18), 4 pre-post with no control group (9,11,19,20), one study protocol (2), and one randomized control study (13).

Full table
Seven studies focused on emotional support (9,10,13-16,19); two studies focused on sexual and reproductive health information (11,20); two studies focused on addiction support (12,17); and one study focused on enhancing service accessibility (18). Studies emphasized on problem gambling (14,17); sexual assault (10); mental health and suicide (15,16,19); lesbian, gay, bisexual, transgender and questioning (LGBTQ) youth (16); alcohol and other substances (12,18); and colostomy patients (13). Additionally, some studies served specific age groups, such as children (9), adolescents and youth (16,19,20), teens and young adults (11), and adults (12,13). Studies were only located in high income countries: Australia (14,17,18); United States of America (10,11,16,20); Netherlands (9,15), Canada (19), China (13), and Hong Kong (12).
Nine programs had 24-hour or continuous methods for the chat-based hotline (9,10,12,13,15-18,20) and three programs had extended times for chat-based services (11,14,19). Of the three chat-based hotlines with extended times, two were available during and after business hours (11,14), one was available on weekends (11), and one was supplemented with a 24-hour voice line (19). Chat-based hotline respondents included trained counselors (14,16-19), volunteers (9,10,15), and other professionals (11,13,20).
One study utilized WhatsApp as the communication platform (12); one study utilized WeChat and QQ (13); and ten studies utilized helplines or other web-based platforms (9-11,14-20). Nine studies had additional interventions to the chat-based hotline program (9,11-13,15-17,19,20). Chat-based hotline additions included voice call and telephone support (9,13,15,16,19); text messaging (11,20); email support (17); and educational/informational resources (12,13,15,16).
User characteristics
Ten studies measured characteristics of the chat-based applications and its users (9,11,13-20). All ten studies contributed information on the gender of users and user age (9,11,13-20); five studies included user ethnicity (11,14,16,19,20); and three included information regarding first time users (9,14,17).
Seven studies compared user characteristics between chat-based hotlines and other hotlines (9,11,13,17-20). Most studies found that chat users were more likely to be female (9,11,14-16,18-20) with the exception of one who found that males were more likely to be chat users (17). Among studies that reported on race/ethnicity, the majority of participants were white/Caucasian (11,14,16,19,20). Of studies that reported on age, a majority found that younger participants were the primary users: under 40 years old (14,17); average of 13.8 years (9); 18–24 years (11); 14–17 years (19); 15–19 years (20); 18–34 years (15); average of 17.6 years (16); and under 24 years (18) (Table 2).

Full table
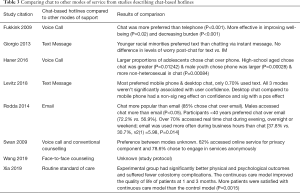
Mode of support comparisons
Eight studies compared chat-based programs with other modes of support (9,11-13,17-20). Of those eight, two studies compared chat to voice call (9,19), two studies compared chat to text messages (11,20), one study compared chat to email (17), two studies compared chat to standard care (12,13), and one study compared chat to voice call and standard care (18). Chat was a preferred method of intervention among 5 of the studies (9,13,17,19,20); 1 study yielded mixed results (11); 1 study did not specify user preference (18); and there were no results for the study protocol (12). Between the two studies that compared chat to voice call, chat was preferred (9,19). Between the two studies that compared chat to text message, one study showed preferences to text message among racial minorities (11), whereas the other study preferred mobile phone and desktop chat over text message (20). For the study comparing chat to email, users preferred chat (17). For the two studies comparing chat to standard care, only one had results: one study yielded significant results in utilizing chat (13), whereas we were unable to determine the results for the study protocol (12). Lastly, the study comparing chat to voice call and standard care resulted in chat being utilized more however user preference was not specified (18) (Table 3).
Full table
Health outcomes
Six studies contributed data on health outcomes. Six articles yielded health outcomes (9,11,13-16). Each of the studies used different scales to measure health effect. One study uses the Problem Gambling Significant Other Impact Scale (PG-SOIS) to measure emotional impact on concerned significant others and found a positive non-significant correlation between problem gambling and emotional impact (14). Another study uses the Cantrill Scale to measure well-being and Strengths and Difficulties Questionnaire (SDQ) to measure quality of life of children, which resulted in a positive non-significant correlation for well-being and positive significant correlation for quality of life (9). One study uses pre-post surveys to measure levels of worry, which resulted in a positive non-significant correlation in feeling less worried post-chat (11). Additionally, one study uses the Crisis Call Outcome Rating Scores (CCORS) to measure emotional states and suicidality of callers, which resulted in most callers (86.1%) were in a suicidal crisis and a positive significant correlation between CCORS and improvements in emotional state and suicidal ambivalence (15).
Another study uses Beck Hopelessness Scale Short Form to measure hopelessness, Abbreviated posttraumatic stress disorder (PTSD) Civilian Checklist to measure PTSD, Center for Epidemiologic Studies Depression Scale Short Form (CES-D-4) to measure depression, Interpersonal Needs Questionnaire (INQ) to measure belonging and burdensome, and Columbia-Suicide Severity Rating Scale (C-SSRS) and Suicide Behaviors Questionnaire-Revised (SBQ-R) to measure suicidality in LGTBTQ youths, which resulted in a positive significant correlation in feeling hopelessness, PTSD, depression, suicidal ratings and behaviors, and a positive nonsignificant correlation in feelings of belonging and burdensome (16). The last study uses the State-Trait Anxiety Inventory (STAI) to measure anxiety, Stoma Care Self-Efficacy Scale to measure self-efficacy, and Stoma-QOL to measure quality of life for colostomy patients, which resulted in a positive significant correlation for anxiety after three months, self-efficacy after one and three months, quality of life after one and three months (13) (Table 4).

Full table
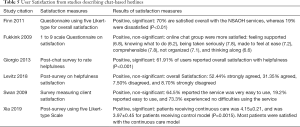
User satisfaction
Table 5 describes the user satisfaction measures and results. Six studies used questionnaires to measure perceived helpfulness and satisfaction of the service (9-11,13,18,20). From the six studies, participants reported high levels of satisfaction with the services provided (9-11,13,18,20).
Full table
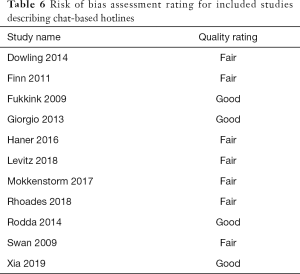
Risk of bias assessment results
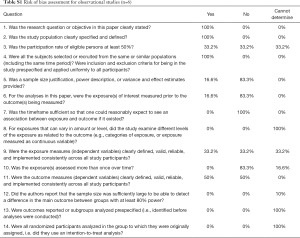
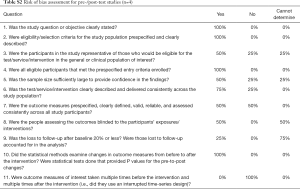
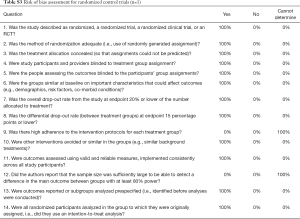
Table 6 shows the risk of bias assessment results for all studies included in the review. Risk of bias was measured for 11 of the studies. Risk of bias was not measured for the study protocol. Each article was assessed using the appropriate guidelines using the Study Quality Assessment Tools. Six studies were assessed using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies (Table S1), 4 studies were assessed using the Quality Assessment Tool for Pre- and Post-Interventions (Table S2), and the remaining study was assessed using the Quality Assessment of Controlled Intervention Studies tool for randomized control trials (Table S3).
Full table
Full table
Full table
Full table
Each study was given an overall quality rating as shown in Figure 2. Quality ratings were evaluated on a scale of Good, Fair, or Poor. Four studies were given an overall rating of Good (9,11,13,17) and seven studies were rated as Fair (10,14-16,18-20). No studies were rated as poor.
Discussion
The findings of this review show that chat-based hotlines have been used for health promotion mostly in the area of emotional support especially for younger (12–24 years old) and female user and have only been evaluated and published in high-income countries. Chat-based hotlines using instant messenger applications were generally preferred by users over other modes of services such as email, text messaging, voice calls, and face-to-face counselling. Evaluations, although limited in rigor due to mostly observational study designs, indicate mostly positive significant effects on mental health outcomes such as anxiety, depression, well-being and suicidality. None of the studies reviewed had a negative effect or no effect. Additionally, we found that user's satisfaction with the services to be moderately high.
The majority of individuals who accessed chat-based hotlines were seeking urgent emotional support services, demonstrating that chat-based services can be instrumental in crisis settings. Additionally, chat-based hotlines included in this study were used for other health promotion activities such as sexual reproductive health advice, addiction support, and a range of other health advice. From the broader literature, we know that telephone hotlines in the US have been used for a much broader range of health promotion services such as the safety for runaways, domestic violence, poison control, eating disorders, HIV treatment, addiction and shoplifting (21). There may be potential for the expansion of chat-based hotline applications to a wider range of health services.
We found that chat-based hotlines have only been evaluated in high-income countries and that evaluation designs lacked rigor. Systematic reviews of telephone-based hotlines or helplines in specific health areas have been conducted including hotlines for cancer caregiver support (22), cancer patient support (23) tobacco smoking cessation (24,25) and alcohol use (24). Results from these hotline reviews also found that published evaluations mostly come from high income countries. These reviews also found that there was limited ability to claim efficacy of the hotlines due to lack of rigor in evaluation designs. The handful of randomized trials that were included in these reviews demonstrated positive findings (22,23).
We did not find any information on cost or cost effectiveness of chat-lines in the included studies in this review but other studies have found telephone hotlines to be cost-effective such as in Belgium where a suicide hotline was found to be cost-saving for the national health insurance plan (26), in New Zealand where a national smoking quitline service was found to be cost saving for the national health system (27) and in Denmark where a national smoking quitline was found to be cost-effective in comparison to other smoking cessation interventions (28). Assessing the cost effectiveness of chat-based hotlines as compared to telephone hotlines is an important research area for funding and scaling this type of intervention.
There are some limitations of this review. First, our systematic review only included studies available in English. Although a majority of the studies found were in English, there were two studies which were excluded due to language limitations. Second, this review only included studies where full text articles or study protocols were available. Although a majority of the articles requested were available, one study was excluded due to the researchers’ inability to obtain a copy of the full text of the article. Third, as with any review, there is potential for publication bias; only peer-reviewed articles published in accessible sources were considered. Organization reports and news articles that discuss chat-based hotlines were not included. Finally, as with most systematic reviews, there is also potential for research bias when applying inclusion criteria and risk of bias assessment criteria. We attempted to minimize this bias by having two researchers work independently and a third researcher to decide in the case of discrepancies.
While the evidence base for the effectiveness of chat-based hotlines in the peer-reviewed literature is limited, they are becoming more popular in the US and in other high-income countries. Large US-based crisis support hotlines such as the National Suicide Prevention Lifeline, RAINN and the National Domestic Violence Hotline have developed chat-based options in response to user preferences. In 2014, many police stations across the US started offering a texting option for 911 callers (29). Expansion of chat-based hotlines to low- and middle-income countries has potential given that mobile phone and mobile application use have grown exponentially over the last fifteen years (30).
Health promotion organizations, particularly those providing crisis support services through telephone hotlines, may also want to consider how chat-based hotlines can expand the reach of their services and user types. In addition, providing an alternative to voice-based hotlines may increase user satisfaction. For researchers monitoring and evaluating chat-based hotline user health outcomes, using standardized metrics such as the CCORS (31) will improve our ability to determine the efficacy of chat-based hotlines among different health outcome categories and modalities. Determining the cost-effectiveness of chat-based hotlines compared to existing interventions is also recommended.
Program planners and funders should consider evaluating whether or not this scalable and potentially cost-effective services may improve health in other contexts and for other types of health promotion activities especially in low- and middle-income countries.
Acknowledgments
We would like to thank the Touro University California librarians for their assistance in obtaining full text articles for this review.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Carinne Brody and Sarah Sullivan) for the series “Digital Interventions for Hard-to-reach Populations” published in mHealth. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/mhealth-2019-di-13
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/mhealth-2019-di-13). The series “Digital Interventions for Hard-to-reach Populations” was commissioned by the editorial office without any funding or sponsorship. CB served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of mHealth from Mar 2019 to Feb 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rosenbaum A, Calhoun JF. The use of the telephone hotline in crisis intervention: a review. J Community Psychol 1977;5:325-39. [Crossref] [PubMed]
- World Health Organization. Preventing suicide: a resource for establishing a crisis line. Geneva 2018; License: CC BY-NC-SA 3 IGO. Available online: https://apps.who.int/iris/bitstream/handle/10665/311295/WHO-MSD-MER-18.4-eng.pdf?ua=1
- Mishara BL, Chagnon F, Daigle M, et al. Comparing models of helper behavior to actual practice in telephone crisis intervention: a Silent Monitoring Study of Calls to the U.S. 1-800-SUICIDE Network. Suicide Life Threat Behav 2007;37:291-307. [Crossref] [PubMed]
- Gerdts C, Hudaya I. Quality of Care in a Safe-Abortion Hotline in Indonesia: Beyond Harm Reduction. Am J Public Health 2016;106:2071-5. [Crossref] [PubMed]
- Statista. Social Media & User-Generated Content: Statistics and Market Data on Social Media & User-Generated Content 2019 Available online: https://www.statista.com/markets/424/topic/540/social-media-user-generated-content/
- Grant R. Why aren’t more crisis hotlines offering chat-based help? The Atlantic 2015;13.
- Bayona E, Menacho L, Segura ER, et al. The Experiences of Newly Diagnosed Men Who Have Sex with Men Entering the HIV Care Cascade in Lima, Peru, 2015-2016: A Qualitative Analysis of Counselor-Participant Text Message Exchanges. Cyberpsychol Behav Soc Netw 2017;20:389-96. [Crossref] [PubMed]
- Pimmer C, Mhango S, Mzumara A, et al. Mobile instant messaging for rural community health workers: a case from Malawi. Glob Health Action 2017;10:1368236. [Crossref] [PubMed]
- Fukkink RG, Hermanns JM. Children's experiences with chat support and telephone support. J Child Psychol Psychiatry 2009;50:759-66. [Crossref] [PubMed]
- Finn J, Garner MD, Wilson J. Volunteer and user evaluation of the National Sexual Assault Online Hotline. Eval Program Plann 2011;34:266-72. [Crossref] [PubMed]
- Giorgio MM, Kantor LM, Levine DS, et al. Using chat and text technologies to answer sexual and reproductive health questions: Planned Parenthood pilot study. J Med Internet Res 2013;15:e203. [Crossref] [PubMed]
- Wang MP. Alcohol brief intervention plus personalized mobile chat-based intervention to reduce alcohol misuse in an emergency department. ClinicalTrials.gov Identifier: NCT03823599, 2019.
- Xia L. The Effects of Continuous Care Model of Information-Based Hospital-Family Integration on Colostomy Patients: a Randomized Controlled Trial. J Cancer Educ 2020;35:301-11. [Crossref] [PubMed]
- Dowling NA, Rodda SN, Lubman DI, et al. The impacts of problem gambling on concerned significant others accessing web-based counselling. Addict Behav 2014;39:1253-7. [Crossref] [PubMed]
- Mokkenstorm JK, Eikelenboom M, Huisman A, et al. Evaluation of the 113Online Suicide Prevention Crisis Chat Service: Outcomes, Helper Behaviors and Comparison to Telephone Hotlines. Suicide Life Threat Behav 2017;47:282-96. [Crossref] [PubMed]
- Rhoades H, Rusow JA, Bond D, et al. Homelessness, Mental Health and Suicidality Among LGBTQ Youth Accessing Crisis Services. Child Psychiatry Hum Dev 2018;49:643-51. [Crossref] [PubMed]
- Rodda S, Lubman DI. Characteristics of gamblers using a national online counselling service for problem gambling. J Gambl Stud 2014;30:277-89. [Crossref] [PubMed]
- Swan AJ, Tyssen EG. Enhancing treatment access: evaluation of an Australian Web-based alcohol and drug counselling initiative. Drug Alcohol Rev 2009;28:48-53. [Crossref] [PubMed]
- Haner D, Pepler D. Live Chat Clients at Kids Help Phone: Individual Characteristics and Problem Topics. J Can Acad Child Adolesc Psychiatry 2016;25:138-44. [PubMed]
- Levitz N, Wood E, Kantor L. The Influence of Technology Delivery Mode on Intervention Outcomes: Analysis of a Theory-Based Sexual Health Program. J Med Internet Res 2018;20:e10398. [Crossref] [PubMed]
- . . Available online: https://psychcentral.com/lib/common-hotline-phone-numbers/Central Psych, Common Hotline Phone Numbers. 2020.
- Heckel L, Heynsbergh NL, Livingston PM. Are cancer helplines effective in supporting caregivers? A systematic review. Support Care Cancer 2019;27:3219-31. [Crossref] [PubMed]
- Clinton-McHarg T, Paul C, Boyes A, et al. Do cancer helplines deliver benefits to people affected by cancer? A systematic review. Patient Educ Couns 2014;97:302-9. [Crossref] [PubMed]
- Danielsson AK, Eriksson AK, Allebeck P. Technology-based support via telephone or web: a systematic review of the effects on smoking, alcohol use and gambling. Addict Behav 2014;39:1846-68. [Crossref] [PubMed]
- Stead LF, Hartmann-Boyce J, Perera R, et al. Telephone counselling for smoking cessation. Cochrane Database Syst Rev 2013.CD002850. [PubMed]
- Pil L, Pauwels K, Muijzers E, et al. Cost-effectiveness of a helpline for suicide prevention. Journal of Telemedicine and Telecare 2013;19:273-81. [Crossref] [PubMed]
- Nghiem N, Cleghorn CL, Leung W, et al. A national quitline service and its promotion in the mass media: modelling the health gain, health equity and cost-utility. Tob Control 2018;27:434-41. [Crossref] [PubMed]
- Rasmussen SR. The cost effectiveness of telephone counselling to aid smoking cessation in Denmark: a modelling study. Scand J Public Health 2013;41:4-10. [Crossref] [PubMed]
- Federal Communications Commission. Text to 911:00:00 What You Need To Know. Consumer Guides. 2020 Available online: https://www.fcc.gov/consumers/guides/what-you-need-know-about-text-911
- The World Bank. Mobile cellular subscriptions (per 100 people) - Low income. World Telecommunication/ICT Development Report and database. 2019 Available online: https://data.worldbank.org/indicator/IT.CEL.SETS.P2?locations=XM
- Bonneson ME, Hartsough DM. Development of the Crisis Call Outcome Rating Scale. J Consult Clin Psychol 1987;55:612-4. [Crossref] [PubMed]
Cite this article as: Brody C, Star A, Tran J. Chat-based hotlines for health promotion: a systematic review. mHealth 2020;6:36.