
Retrospective evaluation of a pilot eHealth/mHealth telewellness program for people with disabilities: Mindfulness, Exercise, and Nutrition To Optimize Resilience (MENTOR)
Introduction
In the United States, the current system for funding quality healthcare for people with disabilities is fundamentally broken (1,2). Working-age adults with disabilities visit their healthcare provider and the emergency department more frequently than people without disability (3), and individuals with mobility disability—both recently acquired and existing for many years—are seldom exposed to wellness programs that focus on improving their quality of life using adaptations where necessary to accommodate their level of health and function (4). To be clear, this does not incriminate healthcare providers as uninterested or apathetic about promoting wellness; on the contrary, many healthcare providers would welcome spending more time with patients were it not for the strong demands from health insurance providers to ensure that company profits are maintained or increased by seeing more versus less patients daily.
Another issue regarding wellness promotion is the challenge of implementation failure. While there are several health promotion/wellness interventions that have been found effective for promoting certain areas of health in people with disabilities (5-8), these interventions seldom, if ever, get translated into mainstreamed community-based health/wellness programs. Moreover, there are no scale-up community programs that have been endorsed by healthcare providers that support the needs of people with disabilities in lifelong wellness. Onsite facilities are often inaccessible due to several architectural and programmatic barriers (9). While the focus of this evaluation study pertains to people with disabilities in the U.S., these issues are not isolated to one country. In the World Report on Disability (10), the World Health Organization (WHO) noted that people with disabilities across the world experience multiple barriers to quality healthcare and health promotion, thus increasing their risk for multiple chronic health conditions (p.60–65).
Home-based telehealth programs provide a viable option for reaching people with disabilities who have difficulty getting to and from community-based wellness programs and venues. Compared to only a few years ago, millions of people now have internet access through cellular networks, and many choose them rather than subscribe to broadband access (11). Commercial video platforms like Zoom are also more ubiquitous post-pandemic, and ownership of smartphones has increased dramatically over the past 5 to 10 years (12). Additionally, a wide variety of assessment and treatment interventions can now be delivered to clients using remote monitoring systems (13).
Reviews of literature on health promotion/wellness call for more comprehensive lifestyle wellness programs that go beyond nutrition and exercise and involve a combination of interventions that enhance not only physical and metabolic health, but also address mental, emotional, and spiritual development, social relationships, sleep and other critical behaviors that can optimize one’s health (14,15). The published literature on telehealth interventions for people with disabilities continues to focus, to a large extent, on one or two health promotion strategies (i.e., exercise, diet) (16,17) typically delivered through one-on-one health coaching. This has created a substantial gap in understanding the potential benefits of more comprehensive lifestyle wellness programs that are group-based and address multiple areas of wellness. As the internet and smartphone become more available in geographically isolated areas across the globe, mobile health will continue to play a greater role in reaching underserved populations including people with disabilities (11). For this reason, we conducted a retrospective evaluation of a publicly available comprehensive wellness program called MENTOR (Mindfulness, Exercise, and Nutrition To Optimize Resilience) to explore the program’s usability and effectiveness in improving the health of adults with disabilities. This paper describes the program implementation elements and provides a brief quantitative and qualitative evaluation of MENTOR’s first pilot program. We present the following article in accordance with the STROBE reporting checklist (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-21-34/rc).
Methods
Design and purposes
This retrospective evaluation study had three purposes. The first purpose was to quantitatively evaluate the reach of MENTOR and its preliminary effects on physical activity level and wellness (physical, mental, and emotional health, and overall perceived wellness). A secondary quantitative purpose was to examine whether benefits differed among people who had low or high starting baseline values of physical activity and overall wellness. The third purpose was to qualitatively explore participants’ perceptions of issues or challenges with implementation processes that could be used to improve MENTOR on its next iteration, as well as explore further potential program benefits.
MENTOR overview
The MENTOR program (Figure 1) was designed for people with a physical disability living in the United States. MENTOR was an 8-week, 40-hour program (5 sessions/week, 1 hr/session) that was based on a set of evidenced wellness practices designed to support participants in improving their health (14,15,18). MENTOR included group classes Monday through Friday for mindfulness, exercise, nutrition, and health coaching. MENTOR targeted a total of 11 wellness domains. The three core wellness domains were Mindfulness, Exercise, and Nutrition (the MEN in MENTOR). The remaining eight wellness domains were self-care skills, core values, outdoor time in nature, rest/relaxation, contribution to others, arts and leisure, relationships, and spiritual practice. The program was funded by the U.S. Centers for Disease Control and Prevention.
Recruitment/eligibility
Participants were recruited from five rehabilitation centers across the U.S. in Birmingham, AL, Boston, MA, Chicago, IL, Denver, CO, and New York, NY. A formal memorandum of understanding (MOU) was signed by each participating center with the goal to recruit approximately 30 people into the MENTOR program and to assign two to three part-time staff who would be trained as MENTOR health coaches. People were eligible for the program if they met the following criteria: (I) between the ages of 18 to 70 years; (II) a self-reported physical/mobility disability; (III) internet access; and (IV) ability to access the program materials independently. Each participating center was responsible for developing their own recruitment materials. Participants were directed to a website where they could enroll in the program.
MENTOR program
The MENTOR program consisted of a comprehensive set of wellness practices designed to support participants with disabilities improve their health (14,15). Participants signed up for an 8-week, synchronous wellness program (5 hr/wk.) using Zoom videoconferencing and directed by a trained health coach. The three Core wellness domains (mindfulness, exercise, nutrition) were taught by qualified instructors (mindfulness-certified instructor, exercise specialist, registered dietitian), and the eight other domains were taught by trained health coaches. Since people with disabilities have been reported to have higher rates of social isolation and loneliness compared to the general population (19), a group-based class format was used to provide participants with a social support structure that allowed them to interact with each other during class. Participants were provided with exercise equipment for the program, which included an exercise mat, leg/arm pedal bike, loop resistance bands, resistance bands with handles, wrist weights, wobble disc, small ball, yoga blocks, racquet ball, and sliders.
MENTOR’s core wellness domains
Exercise
Each class was taught in a group-based format. The exercise classes were offered two days a week for 1 hour each day (Tuesday/Thursday). During the first session participants were instructed on how to perform the exercise routines and were provided with a general overview of exercise safety for the first 30 minutes. This was followed by 30 minutes of exercise. The majority of the time in the second exercise session was spent performing the exercise routine, which included adaptations of fitness activities in strength, range of motion, balance and cardiorespiratory endurance based on participants’ functional level. For example, participants who were unable to stand (e.g., spinal cord injury) could perform an adapted version of the exercise routines in their wheelchair using their arms only.
Nutrition
The nutrition classes were taught once a week (Wednesday) and led by a registered dietitian. The classes focused on key areas of basic nutrition such as preparing meals; demonstrations of various recipes on how to increase fruit and vegetable consumption by making them more palatable; discussion of strategies for purchasing healthy foods on a limited budget including denoting certain products that can replace more costlier brands, reducing processed foods and replacing them with whole foods, and lowering sugar intake using natural alternatives. All the recommended foods were approved by the WIC (Women and Infants/Children) and SNAP (Supplemental Nutrition Assistance Program) U.S. federal assistance programs.
Mindfulness
The mindfulness classes were taught once a week (Monday) by a trained mindfulness instructor. Participants were taught the basic components of mindfulness including positioning (techniques for wheelchair users), proper respiratory control, and strategies to reduce unwanted thought patterns.
MENTOR’s wellness eight other domains
The eight additional wellness domains (self-care skills, core values, outdoor time in nature, rest/relaxation, contribution to others, arts & leisure, relationships, spiritual practice) were provided to participants by a trained health coach who met once a week (virtually) with their assigned group (Fridays). Given the brief amount of time allocated to each domain (1 hr/wk), the focus was to provide MENTOR participants with several high-level pointers. For example, under rest/relaxation (which included sleep quality), participants were provided with a set of recommendations that included going to bed at a consistent time of the evening, setting a cool room temperature (between 65 and 68 degrees), waking at the same time of day, reducing lighting in the room, avoiding blue lighting from computer screens and mobile phones, avoiding night eating, and sleeping seven to eight hours a night. Under self-care skills, participants were provided with a brief set of recommendations on good bladder/bowel/skin management, managing medications, and understanding how to advocate for higher quality healthcare. The emphasis of each of these sessions was to encourage participants to self-manage their health by practicing certain health behaviors that could improve one or more of these wellness domains. Upon request, participants were provided with additional resources in any of the eight wellness domains.
MENTOR procedures
Software
Coaching platform
Figure 2 illustrates the two commercial software platforms used in MENTOR. Rise commercial software (left screen) was used to train health coaches. Rise utilizes an intuitive e-learning platform and learning management system that allowed MENTOR’s graphic designer and developers to create interactive modules providing trainees with the ability to click buttons, drag and drop objects, and enter text. Modules included an overview of MENTOR, assessment and goal setting, how to use the coach-participant platform, and a section for each of the 11 wellness domains. Modules were broken into digestible trainings consisting of video, interactive games, knowledge checks, and attractive imagery. The platform also allowed MENTOR staff to track each trainees’ progress and to monitor how long it took to work through each training module. Time stamps were used to re-evaluate certain material when it was necessary to make the content clearer or more engaging to health coaches. Trainings were accessed by health coaches on a laptop computer or smartphone.
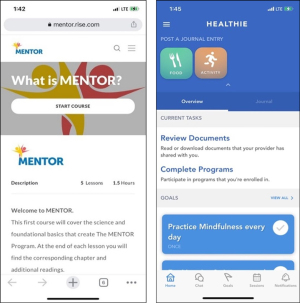
Coach-participant platform (HEALTHIE)
The right side of Figure 2 provides a screenshot of the HEALTHIE platform that was used by health coaches and participants as a ‘one-stop shop’ for accessing all assessment and intervention tools on any mobile device (phone, tablet, laptop, desktop). Coaches and participants were able to access their account from any iOS or Android device for convenient support. Participants received a password-protected ID and when they logged into the website, they were greeted with a dashboard that allowed them to track their own activities. The software also allowed the MENTOR health coach coordinator to create intake flows to collect baseline and follow-up health data as well track analytics (e.g., logins, page views). Participants were able to see their goals and upcoming intervention sessions and activities.
One of the unique features of the HEALTHIE platform was that it removed the constant back and forth of emailing to remind participants of sessions, check-ins, and when their next video training occurred. Since the platform could be accessed on a computer or via a smart phone app, coaches were able to email or text participants for various items (e.g., reminder about the next day’s class, what to read prior to the upcoming health coaching session). HEALTHIE integrations include HIPPA-compliant Zoom, a calendar for scheduling sessions, a resource library, and SMS messaging features.
Telelogistics support protocol
The telelogistics components of MENTOR included online enrollment, teleassessment, and implementation procedures. These procedures were managed by a telelogistics support team involving 10 personnel: 4 program staff and 6 health coaches. After enrollment, participants were placed on a waitlist and contacted by the MENTOR participant engagement coordinator. The coordinator explained the program logistics and referred participants to the HEALTHIE platform where they read and signed an electronic consent form and completed a set of health/wellness questionnaires.
MENTOR was rolled out in waves (i.e., groups of participants who were ready to begin the program). Two weeks prior to the start of each wave, the participant engagement coordinator recontacted participants via phone to confirm that they were still interested in the program and to provide them with a final list of program details including their start date, class schedule and the list of exercise equipment that they would receive via UPS. MENTOR staff (program coordinator and two assistants) packaged and shipped the program equipment directly to participants’ homes (2-day shipping). Equipment packaging was performed in a teledistribution room that was located at the site where the MENTOR staff and telehealth facilities were located.
One week prior to the start of the program, participants were contacted through the HEALTHIE platform for final preparations. They were provided with an automatic reminder for the date and time of class sessions via email and SMS. If a participant did not attend a class within the first two weeks of the program, the participant engagement coordinator contacted the participant via phone to assist with any issues. The classes were run by trained health coaches through the HEALTHIE platform, which included a goal setting feature where participants recorded their goals, a Zoom videoconferencing link for the online classes and coaching sessions, and a section where health coaches could share materials with participants. After completing the program, participants were automatically sent the post-evaluation questionnaires through HEALTHIE.
Sample and measures
The pilot MENTOR program included a quantitative and qualitative evaluation of a subset of participants who completed the MENTOR program. Participants who went through the program were asked to complete the same set of baseline measures after the 8-week program. However, no participant was required to complete the post-test measures since the program was already being offered to participants through a federally funded center (CDC) and the focus of this evaluation study was on quality improvement. The data analyzed involved participants who had a set of pre/post measures.
Quantitative data included geographic distribution (reported through enrollment data), a self-report measure of physical activity (Godin Leisure-Time Exercise Questionnaire, GLTEQ), and a brief self-report wellness assessment [UAB/Lakeshore Wellness Assessment (LWA)]. The GLTEQ is a 7-day recall questionnaire that contains three questions pertaining to light, moderate, and vigorous intensity activity. There are two ways to score the GLTEQ. The Total Activity score is the sum of all three types of intensities including, light, moderate, and vigorous, after being multiplied by 9, 5, and 3, respectively. The Health Contribution score is the sum of only the moderate and vigorous activity, and this score has been linked with health enhancing volumes of exercise (20). A score of <24 indicates a person is insufficiently active, whereas a score of ≥24 indicates a person is physically active.
The UAB/LWA (see Appendix 1) is a 16-item questionnaire that provides a brief self-report assessment of a person’s overall wellness in the three dimensions of health: physical, mental and emotional. There are five questions in each health dimension and one overall summary question. The questionnaire was analyzed for reading level and met the standards of readability at the 9th grade reading level. Scoring is on a 1–5 Likert scale (1 very unsatisfied to 5 very satisfied). LWA scores of 1–5 were multiplied by a value of 10 to provide a calculation score between 10 and 50 for each item. The tool has face validity, as it was created through several collaborative iterations between disability fitness experts and stakeholders from an adapted fitness facility (Lakeshore Foundation, Homewood, AL) and serves as a criterion-referenced tool to monitor changes in participant wellness at the beginning and end of the program.
Measurement procedures
To assess the MENTOR program, quantitative pre to post evaluation and post-intervention qualitative interviews were utilized. Since the program was offered to participants as a community program and not a research study, completion of the study questionnaires, interviews, and surveys was encouraged but not mandatory. This study analyzed data from as many people as possible who had no missing pre and post data. All data were entered directly into an online database and analyzed by a project statistician who was not involved with the intervention.
Qualitative data in the form of participant post-intervention interviews and surveys were used to explore participants’ perceptions about their experience with the MENTOR program, in relation to potential benefits of MENTOR and issues or challenges with implementation processes. Participants who completed the program had the option of providing their feedback through a one-on-one video conference interview or via an online survey. Interviews lasted no longer than 45 minutes and contained 10 general questions pertaining to: overall perceptions of the program, likes and dislikes regarding implementation processes, and potential physical, mental, or behavioral benefits. Interviews were conducted via video conference by a trained qualitative research assistant that was not involved with the intervention. The interviews were audio-recorded and transcribed for analysis. An email was sent by the participants’ health coach reminding them to complete the posttests. Interview and survey responses were optional for participants, and they were not compensated for participation.
Statistical analysis
To address the first study purpose, we recorded and presented descriptive enrollment data for reach and conducted two sets of analyses for potential benefits to GLTEQ and LWA scores: analyses for all participants, and analyses for participants with low baseline scores. Intervention reach data included the number of people enrolled, completed, and dropped out of the program, as well as sex and state location. Other descriptive data included means, standard deviations, and effect size (Cohen’s D) estimates were reported for the GLTEQ and LWA. Effect size estimates were interpreted as follows: 0.2, small; 0.5, medium; 0.8 large (21).
GLTEQ scores were not normally distributed and therefore, Wilcoxon matched pair signed rank tests were used to examine pre-post changes in both GLTEQ Total Activity and Health Contribution scores. LWA scores included normal and non-normal data and included paired t-tests and Wilcoxon signed rank tests as appropriate. Participants with missing or incomplete data (e.g., have not completed the program or did not complete all posttests) were excluded from the analysis. These procedures were done for all participants, as well as participants with low baseline scores. All statistical analyses were conducted using IBM SPSS statistical software (version 27).
Since MENTOR is a CDC-funded Quality Improvement (QI) program versus a prospective, hypothesis-driven study, the program was open to anyone with a physical disability. Therefore, we did not control for participants who had high starting baseline wellness scores (i.e., ceiling effect) in the outcomes of interest. As a pilot project, we conducted a set of analyses that included all people and a set of analyses for a subset of participants who had low baseline values. The rationale for the subset analyses is that research projects typically exclude people who may have high baseline values (e.g., exclude people at baseline who have high levels of physical activity). For the GLTEQ, a high baseline value was a Health Contribution Score ≥24, which classifies a person as participating in sufficient volumes of physical activity to achieve health benefits (20). A UAB-LWA response for item 16 (overall wellness) of 4 (satisfied) or 5 (very satisfied) (transformed to a score of 40 to 50) was considered a high baseline value.
Philosophical assumptions that underpinned all aspects of the qualitative evaluation component were ontological subjectivism (multiple realities) and epistemological interpretivism (knowledge is created by the interaction of all parties). The qualitative researchers noted that participants could experience different perspectives of the program, and recollections of the program and the presentation of the findings were constructed by the interaction between the participants, interviewer, and analysts.
Inductive thematic analysis (22) was used to analyze qualitative data (both the interviews and surveys). First, the research team transcribed and crosschecked the data for accuracy while reading the transcriptions. Next, two analysts generated initial codes that were written in the text to resemble their interpretations of short data segments. Codes were generated iteratively across each transcription. After initial coding, analysts independently searched their codes for patterns and, from these patterns, generated overarching themes based upon internal and external homogeneity (23). Last, the analysts then met to articulate their viewpoint of the overall data and compare their themes. In consideration of the small sample of interview participants (n=6), the coders aimed to generate a small number of rich themes and only two coding levels (codes and themes) to enhance the likelihood that the themes would be saturated (i.e., themes that appropriately and adequately related to quality improvement) (24).
Regarding rigor, member reflection was performed as necessary to “generate additional data and insight” (25), whereby the interviewer contacted participants post-interview to resolve gaps and ambiguous data (26). Additionally, during interpretation of the qualitative data, the analysts engaged in an in-depth process of critical dialogue referred to as ‘critical friends’(25). Specifically, they gave voice to their interpretations of the data and offered each other critical feedback based upon their epistemological beliefs. The goal of this dialogue was not to merely agree or disagree on their interpretations of the data, but instead encourage reflexivity to support and defend their viewpoints. The analysts used this strategy to increase the likelihood that the most plausible interpretations of the data were recognized. Finally, the analysts kept an audit trail so that themes could be traced back to the segments of text they were generated from. One researcher was a person with a spinal cord injury and had a background in delivering health promotion programs to people with physical disabilities. The other researcher was a resident in physical medicine and rehabilitation with a background in treating patients with neurological (e.g., spinal cord injury, stroke) and musculoskeletal conditions.
Ethical statement
The local IRB granted a research exemption for this study designating it as a quality improvement evaluation study of an existing program. Data were aggregated across centers using identifiers to prevent loss of confidentiality. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was waived due to the retrospective nature of the study.
Results
Reach
To date, MENTOR has enrolled a total of 154 people with disabilities across the U.S (mean age 49±15 years; range, 21–71 years). One-hundred and thirty-five participants (96 females/39 males) completed the program. Nineteen participants (12%) did not complete the program. Participants had the following physical/mobility disabilities: multiple sclerosis (n=35), spinal cord injury (n=33), stroke (n=16), cerebral palsy (n=12), traumatic brain injury (n=9), spina bifida (n=6), Parkinson’s (n=3), amputee (n=1), and 20 reported ‘Other’ condition. They resided in 15 different states.
UAB/LWA
Fifty-three participants who completed the program (mean age 52±16 years) had complete data for the LWA. Table 1 shows the results for two sets of participants, all participants and a subset of participants who reported low baseline scores. For all participants, LWA results demonstrated statistically significant improvements in exercise behavior (P=0.006; effect size =0.39) and contribution to society/community (P=0.013; effect size =0.37). Secondary analyses for 25 participants with low UAB-LWA baseline scores demonstrated statistically significant improvements in exercise behavior (P=0.0001; effect size =1.05), nutrition (P=0.004; effect size =0.71), sleep (P=0.012; effect size =0.56), core values (P=0.01; effect size =0.57), self-care (P=0.023; effect size =0.50), hobbies (P=0.027; effect size =0.54), contribution to society/community (P=0.003; effect size =0.75), relationships (P=0.006; effect size =0.63), and overall wellness (P=0.0001; effect size =1.07), with a trend for outdoor time in nature (P=0.063; effect size =0.43).
Table 1
| Variables | All 53 participants (pre and post) | 25 participants who reported a baseline wellness score <30 (pre and post) | |||
|---|---|---|---|---|---|
| Mean ± SD | P value | Mean ± SD | P value | ||
| Physical health | |||||
| Exercise | Pre: 23.49±14, post: 30.47±12 | 0.006* | Pre: 17.6±11, post: 34.8±12 | 0.0001* | |
| Nutrition | Pre: 29.62±14, post: 33.49±12 | 0.155 | Pre: 23±13, post: 50±11 | 0.004* | |
| Self-care | Pre: 44.06±7.8, post: 40.19±11 | 0.081 | Pre: 43±9, post: 42±11 | 0.878 | |
| Sleep | Pre: 29.91±13, post: 32.74±13 | 0.239 | Pre: 24.2±12, post: 33.6±13 | 0.012* | |
| Pain management | Pre: 23.3±15, post: 24.34±13 | 0.673 | Pre: 26.6±15, post: 23.4±13 | 0.401 | |
| Mental health | |||||
| Managing negative thoughts | Pre: 21.23±15, post: 20.28±13 | 0.785 | Pre: 26.4±16, post: 21±14 | 0.188 | |
| Core values | Pre: 30.47±14, post: 32.08±13 | 0.607 | Pre: 24.6±11, post: 34.4±14 | 0.01* | |
| Self-care | Pre: 35.75±11, post: 34.53±12 | 0.72 | Pre: 29.8±11, post: 37±11 | 0.023* | |
| Depression & loneliness | Pre: 16.32±14, post: 18.77±12 | 0.355 | Pre: 22±14, post: 18.2±13 | 0.387 | |
| Hobbies | Pre: 24.91±16, post: 29.43±14 | 0.135 | Pre: 19.8±15, post: 32±14 | 0.027* | |
| Emotional health | |||||
| Inner peace | Pre: 15.47±13, post: 17.83±13 | 0.265 | Pre: 18.6±14, post: 18.6±13 | 0.913 | |
| Contribution to society/community | Pre: 22.1±14, post: 29.6±12 | 0.013* | Pre: 17.6±12, post: 30.8±12 | 0.003* | |
| Spiritual practice | Pre: 30.09±13, post: 30.47±12 | 0.856 | Pre: 26.6±13, post: 30.2±13 | 0.362 | |
| Relationships | Pre: 34.55±13.2, post: 36.8±11 | 0.356 | Pre: 27.6±12, post: 37.2±11 | 0.006* | |
| Outdoor time in nature | Pre: 25.66±16, post: 30.94±13 | 0.102 | Pre: 21.8±16, post: 32.4±14 | 0.063 | |
| Overall score | Pre: 27.74±11, post 31.04±11 | 0.099 | Pre: 18.6±6, post: 31.8±12 | 0.0001* | |
Data source: MENTOR program. *, statistical significance. UAB, The University of Alabama at Birmingham; LWA, Lakeshore Wellness Assessment; MENTOR, Mindfulness, Exercise, and Nutrition To Optimize Resilience.
Physical activity
GLTEQ data from 12 participants were excluded due to missing data or incompleteness, leaving a total of 41 participants included in the analyses. GLTEQ results for all 41 participants demonstrated no statistically significant improvement from pre to post intervention in either Total Activity or Health Contribution score. However, secondary analysis including 32 people who were physically inactive at baseline (i.e., GLTEQ Health Contribution Score <24) resulted in statistically significant improvements in both Total Activity score (pre mean =15.4±13, post mean 25.8±19.6; P=0.002; effect size =0.56) and Health Contribution score (pre mean 6.2±8, post mean 25.8±20; P=0.005; effect size =0.53).
Qualitative findings
A convenience sample of 35 participants with disabilities who participated in the MENTOR program provided feedback on what they liked about the program and what they would like to see improved. Nine participants completed semi-structured interviews, which were recorded and transcribed, and an additional 26 completed a survey with the same open-ended questions as used in the interviews. The resultant qualitative themes were: (I) lifestyle transformation, and (II) engagement through accessible online bonding. Table 2 presents the themes with codes and their supportive quotes.
Table 2
| Themes | Codes | Supporting quotes |
|---|---|---|
| Lifestyle transformation | The program provided new and positive experiences for participants | “You learn so much and you have so much hands-on experience and working out, and nutrition and meditation and mindfulness. It’s a life changing program really.” (P1) |
| Participants experienced improvements to physical and mental health | “I’ve gotten my, how would I say, my stamina back and I’ve maintained it and everything and energy’s doing great. I’ve actually lost a little over five pounds in the last few weeks, which has had to do with eating healthier.” (P1) | |
| Participants adopted healthy habits | “I was able to quit smoking, thanks to the inspiration and support from MENTOR. It was already one of my goals to be more mindful of my cigarettes, but I didn’t expect, I didn’t expect me to be able to quit completely and I did.” (P1) | |
| Engagement through accessible online bonding | The classes promoted experiential learning and social connectedness | “The thing that I liked most about them is that she came up with creative ways to teach us the lessons. Some of it was animated stuff. Then some of it was just regular videos, and then just learning some adaptive equipment that I could use, actually use my kitchen.” (P4) |
| “I think it (the program) is a wonderful thing because we had one little girl in our group, and she’s young, very young and fairly newly, you know, diagnosed I thought, to see her go from the beginning, I mean just the short of course eight weeks is a short time, but to see her smiling and laughing and we all were. I think that is a huge benefit that I saw, not only for myself, but for all of us in the group.” (P2) | ||
| Coaches were perceived as professional and personable | “……very good teacher. She was a very pleasant teacher, and she had her stuff together, I would say. She had all the information for us that we needed.” (P6) | |
| “I really liked my health coach. Whenever we talked it was just the bright spot of my day.” (P8) | ||
| Accessibility and accountability enhanced participation | “It was so convenient having the products delivered and being able to just have it all right there. We were very spoiled. They made it very easy to just prepare it.” (P5) | |
| “I thank God that I did have access to the Zoom on my phone so that I didn’t miss anything.” (P7) | ||
| Post-program support can promote sustainable behavior | “Maybe just make the program longer because I didn’t want it to end.” (P2) | |
| “I understand that mentor was an eight-week program, but maybe there needs to be an after program.” (P7) | ||
| “It felt like it was just beginning to get started when it was coming to an end like everyone’s just beginning to understand and it was coming to an end.” (P1) |
Data source: MENTOR program. MENTOR, Mindfulness, Exercise, and Nutrition To Optimize Resilience.
Lifestyle transformation
Participants reported that the program led to the adoption of a variety of healthy habits including positive changes in nutrition, meditation, physical activity, and smoking behavior. These habits became part of their daily routine and led to several benefits, such as increased physical activity, energy, mental alertness, self-esteem, improved sleep quality, and weight loss. Every participant mentioned at least one way in which the MENTOR program influenced their lifestyle.
Engagement through accessible online bonding
Enjoyment was consistently reported as a positive aspect of the program, which was related to the social connectedness that participants felt through their online experiential learning. They reported that the classes promoted interactive learning activities, such as cooking, exercising, and breathing and meditation exercises, which they enjoyed performing with other participants. They also reported feeling socially connected through the class activities because of visual and social communication with other people with similar disabilities. Moreover, participants noted that the interactions with their health coach were a key element of program enjoyment and success.
Participants perceived health coaches as professional, knowledgeable, and well-prepared for each session. They noted that they really enjoyed their coaching sessions because they felt comfortable discussing their personal wellness goals with their coach. They also felt that the coaching sessions helped them adhere to the program and be accountable for practicing the skills in their daily lives. Of note, participants expressed a strong desire to increase the duration of program support. Specifically, they recommended that there should be further support after the program to increase the likelihood that they would sustain their behaviors because the program content was ‘rich,’ and the adoption of behaviors required time.
Regarding accessibility, participants noted that they enjoyed the online format and classes offered through videoconferencing technology, which helped them maintain strong adherence to the program. Participants also noted that they felt a strong connection with other participants in their group and appreciated the program being tailored to meet their unique needs and interests. They also appreciated being able to access the program through their mobile phone or tablet so that they did not have to be anchored to one location in their home (i.e., behind their desktop). The benefit of using these mobile devices versus a desktop computer was that they could move around the house to multiple locations to participate in the classes (e.g., kitchen when learning and/or preparing new recipes, large room for performing exercise, quiet space for health coaching calls).
Discussion
Wellness programs need to go beyond exercise and diet interventions and take a broader approach to optimizing health using a combination of interventions that enhance physical, intellectual, emotional, spiritual, and social well-being (15,27). The MENTOR program was designed based on this growing volume of literature and the need to address a constellation of health behaviors that can improve and sustain physical, mental and emotional/spiritual health in people with disabilities. The findings from this retrospective evaluation study of a novel telewellness program designed for people with disabilities demonstrated good usability of the software (HEALTHIE) and videoconferencing technology (Zoom), allowing participants to socially interact with other participants in their group, the mindfulness, exercise and nutrition instructors, and their health coach.
Quantitative findings demonstrated that a comprehensive telewellness wellness program designed for people with disabilities was effective in improving certain areas of wellness. For all participants, including those with good baseline scores in wellness (satisfied or very satisfied with their overall wellness), two wellness domains improved: exercise and contribution to society/community. It is not surprising that the other wellness domains did not improve given the issue of ceiling effects limiting their ability to make large enough gains to reach statistical significance. Since the MENTOR program included about 90 minutes a week of group-based exercise classes, it’s plausible that active participants may have achieved an increase in physical activity by maintaining their regular exercise routine while adding these two additional classes. Regarding contribution to society/community, health coaches noted that there was a great deal of bonding among participants that may have led to feeling that they were ‘giving back’ to the participants in their group. Health coaches heard several anecdotal comments about participants exchanging email addresses or phone numbers and staying in contact with each other after the program ended. Being supportive of other individuals is an important finding that needs to be explored further as the research on ‘giving’ back to others is associated with significant improvements in health including a lower risk of mortality (28).
Participants who reported low overall wellness scores at baseline demonstrated significant gains in eight of the 11 wellness domains. This included exercise, nutrition, sleep, core values, self-care, hobbies, contribution to society/community, and relationships. Participants also achieved a large, statistically significant effect in overall wellness. This finding demonstrated that improvements in multiple areas of wellness can be achieved in a relatively short period of time (8 weeks) through a mobile health platform that significantly reduced the time (getting to and from a facility) and costs (transportation, paying for a membership at a local fitness facility) associated with most onsite wellness programs, two of the most challenging barriers to overcome for people with disabilities (9,29).
The qualitative findings supported the quantitative findings in explaining program benefits and successful usability elements. Participants reported improvements to physical and mental health as a consequence of the adoption of new healthy habits and behaviors (Table 2). Successful implementation processes led to the adoption of health behaviors, which can be replicated in future telewellness programs. Professional and personable coaches, accessible web-utilities, and group-based learning were key elements of facilitating engagement. Moreover, telewellness programs should place a strong emphasize on post-program support. Participants perceived MENTOR to be short in duration and desired support to enhance the likelihood that behaviors they adopted would be sustained over time. Future research is needed to examine the sustainability of benefits obtained from a telewellness intervention and identify optimal strategies for increasing sustainability.
The MENTOR pilot program had a primary focus on empowering participants to take control of their health by enabling greater personalized choice and control. The program placed a strong emphasis on obtaining input from participants to continuously improve the program. For instance, the mindfulness classes were originally offered later in the week, but several participants recommended that they be offered at the beginning of the week so that they could start off with a better mindset. Participants also suggested that the classes be recorded so that they could watch the video if they were unable to attend a certain class and be prepared for Friday’s coaching call. It’s plausible that some participants may have watched certain videos more than one time. We also recognized that participants did not want to spend an inordinate amount of time completing the assessments. In future offerings of MENTOR, we plan to limit baseline and post-assessments to a maximum 45 minutes.
A recent study found that one out of three people living in rural areas in the U.S. has a disability, a significantly higher rate than in urban and suburban settings, which is typically reported as one in five people with disability (30). In order to reach this underserved segment of the population, there must be multiple delivery systems that allow people to participate in wellness at home and/or in their community. While the emphasis in the health promotion literature leans toward encouraging people to use indoor (e.g., fitness centers) and outdoor facilities (e.g., parks) to promote their own wellness, we believe that both a home-based program and access to community services are both necessary to achieve optimum health in people with disabilities. Community-based programs allow for greater social interaction by taking advantage of the health benefits gained from being outdoors in parks and other green environments, meeting up with friends at coffee shops or local organizations (e.g., churches, community centers), and visiting local farmers markets to purchase fresh fruits and vegetables. Supplementing an onsite program with a telewellness option may accommodate people who experience certain community-based barriers (e.g., lack of transportation, limited programs in rural areas) that prevent them from participating in these programs on a regular basis.
Since the MENTOR pilot program was designed as a quality improvement program, there were limitations. First, we had to offer the program to any participant with a disability, including those who already had high wellness scores, increasing the likelihood of a ceiling effect for several participants. Second, a subset of participants did not complete the post-assessment. We learned from several post-assessment interviews that the baseline surveys took over 2 hours to complete and that they didn’t want to spend the time completing the same assessments. The MENTOR team is now exploring ways to reduce the burden of the assessments. Third, it’s unclear how many people with disabilities were interested in participating in the program but did not have a smartphone or internet access. In the future, we plan to collect information on the number of people with disabilities who do not have internet access or a smartphone and identify ways that we can increase their access to the program through hotspots or providing a small number of participants with tablets. Fourth, the inclusion criteria did not target people with intellectual disability. While we feel that most or all of the program elements (with the appropriate adaptations and offering additional caregiver or health coaching training/support) are relevant to adults with intellectual disability, further efforts are needed to test the program’s utility and effectiveness with people with intellectual disability. Fifth, while we use the term Resilience in the title of MENTOR, we did not have a resilience measure. We plan to add a measure of resilience in future iterations of the program. Sixth, being a nationally funded study, the program was implemented only within the U.S. Seventh, given that the HEALTHIE platform was designed for MENTOR with a focus on quality improvement, as opposed to a research-oriented program, data were not available regarding participant engagement (e.g., adherence to the classes or coaching sessions). However, we aim to incorporate attendance monitoring in the next iteration of the program. Lastly, since the program is entirely remote, we’re unable to ascertain what physiological effects may have occurred had we had the opportunity to conduct onsite testing of certain health parameters (e.g., blood pressure, blood glucose, fitness). The program was originally designed with an onsite testing protocol but when COVID-19 began, the entire program was moved online.
Conclusions
The growing field of lifestyle medicine is a reflection of the emergence of holistic wellness as a set of tools that address a broader constellation of health promoting behaviors that target psychological, emotional, intellectual and spiritual development, social relationships and cultural well-being (15,31,32). MENTOR is one of a very small number of comprehensive wellness programs that have been designed for people with physical/mobility disabilities and accessible through multiple portable devices (33). It also is available on a versatile mobile health platform that allows it to grow and expand (rinse and repeat) over the next several years. We envision that MENTOR will also need to become more ‘precision-based’ targeting secondary health conditions that affect a growing number of people with disabilities (e.g., obesity, pain, depression, social isolation).
As mobile technology becomes more affordable and ubiquitous, a greater number of people with disabilities will be able to access programs like MENTOR through their cell phone service (34). We anticipate that over the next several years MENTOR’s reach will be equivalent to the industry’s growth in mobile health. We also recommend that MENTOR be offered to people with disabilities across the world if appropriate resources (e.g., staffing) can be identified to assist with the health coaching components of the program. The future of mobile health for people with disabilities holds great promise for transforming when, where, and how wellness support can be provided to ensure that important social, behavioral, and environmental determinants are used to understand what each individual needs to achieve optimal health.
Acknowledgments
Special thanks to our MENTOR participants who volunteered their time and effort to assist with the implementation of this online quality improvement program.
Funding: Funding for this study was provided by the Centers for Disease Control and Prevention (CDC), Division of Birth Defects and Developmental Disabilities (NCBDDD), Grant #NU27DD000022.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Donna J. Slovensky and Donna M. Malvey) for the series “mHealth: Innovations on the Periphery” published in mHealth. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-21-34/rc
Data Sharing Statement: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-21-34/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-21-34/coif). The series “mHealth: Innovations on the Periphery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The local IRB granted a research exemption for this study designating it as a quality improvement evaluation study of an existing program. Informed consent was waived due to the retrospective nature of the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Turk MA, McDermott S. How to address continued health care differences and disparities among people with disability. Disabil Health J 2017;10:163-4. [Crossref] [PubMed]
- The Lancet. Prioritising disability in universal health coverage. Lancet 2019;394:187. [Crossref] [PubMed]
- Kennedy J, Wood EG. Disability-based disparities in social determinants of health among working-age adults: Evidence from the 2018 National Health Interview Surveys. Collaborative on Health Reform and Independent Living, 2020.
- Carroll NW, Hall AG, Feldman S, et al. Enhancing transitions from rehabilita-tion patient to wellness participant for people with disabilities: an opportunity for hospital community benefit. Front Public Health 2020;8:105. [Crossref] [PubMed]
- Rimmer JH. Health promotion for individuals with disabilities: The need for a transitional model in service delivery. Disease Management and Health Outcomes 2002;10:337-43. [Crossref]
- Block P, Vanner EA, Keys CB, et al. Project Shake-It-Up: using health promotion, capacity building and a disability studies framework to increase self efficacy. Disabil Rehabil 2010;32:741-54. [Crossref] [PubMed]
- Ravesloot C, Seekins T, Young Q, et al. Health promotion for people with chronic illness and physical disabilities: The connection between health psychology and disability prevention. Clin Psychol Pscyhot 1998;5:75-85. [Crossref]
- Castro O, Ng K, Novoradovskaya E, et al. A scoping review on interventions to promote physical activity among adults with disabilities. Disabil Health J 2018;11:174-83. [Crossref] [PubMed]
- Martin Ginis KA, Ma JK, Latimer-Cheung AE, et al. A systematic review of re-view articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev 2016;10:478-94. [Crossref] [PubMed]
- World Health Organization. World report on disability. Available online: https://www.who.int/disabilities/world_report/2011/report.pdf. Accessed 11/18/2021.
- Serrano KJ, Thai CL, Greenberg AJ, et al. Progress on Broadband Access to the Internet and Use of Mobile Devices in the United States. Public Health Rep 2017;132:27-31. [Crossref] [PubMed]
- Pew Research Center. Internet/Broadband fact sheet. Available online: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/#home-broadband-use-over-time. Accessed 8/10/2021.
- Rimmer JH, Lai B, Young HJ. Bending the arc of exercise and recreation technology toward people with disabilities. Arch Phys Med Rehabil 2016;97:S247-51. [Crossref] [PubMed]
- Walsh R. Lifestyle and mental health. Am Psychol 2011;66:579-92. [Crossref] [PubMed]
- Bertozzi B, Tosti V, Fontana L. Beyond calories: an integrated approach to promote health, longevity, and well-being. Gerontology 2017;63:13-9. [Crossref] [PubMed]
- Lai B, Young HJ, Bickel CS, et al. Current trends in exercise intervention research, technology, and behavioral change strategies for people with disabilities: a scoping review. Am J Phys Med Rehabil 2017;96:748-61. [Crossref] [PubMed]
- Motl RW, Sandroff BM. Current perspectives on exercise training in the management of multiple sclerosis. Expert Rev Neurother 2020;20:855-65. [Crossref] [PubMed]
- Strout KA, Howard EP. The six dimensions of wellness and cognition in aging adults. J Holist Nurs 2012;30:195-204. [Crossref] [PubMed]
- Emerson E, Fortune N, Llewellyn G, et al. Loneliness, social support, social isolation and wellbeing among working age adults with and without disability: Cross-sectional study. Disabil Health J 2021;14:100965. [Crossref] [PubMed]
- Amireault S, Godin G. The Godin-Shephard leisure-time physical activity questionnaire: validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept Mot Skills 2015;120:604-22. [Crossref] [PubMed]
- Cohen J. Statistical power analysis for the behavioral sciences. Academic press 2013. Available online: http://www.utstat.toronto.edu/~brunner/oldclass/378f16/readings/CohenPower.pdf
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res in Psychol 2006;3:77-101. [Crossref]
- Patton MQ. Qualitative evaluation and research methods. 2nd ed. Newbury Park, CA: Sage Publications, 1990.
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18:59-82. [Crossref]
- Smith B, McGannon KR. Developing rigor in qualitative research: problems and opportunities within sport and exercise psychology. Int Rev Sport Exerc Psychol 2017;11:101-21. [Crossref]
- Tracy SJ. Qualitative quality: Eight “big-tent” criteria for excellent qualitative research. Qual Inq 2010;16:837-51. [Crossref]
- Schuette SAP, Cordero E, Slosburg K, et al. A scoping review of positive lifestyle and wellness interventions to inform the development of a comprehensive health promotion program: “HealthPro Am J Lifestyle Med 2017;13:336-46. [Crossref] [PubMed]
- Qu H, Konrath S, Poulin M. Which types of giving are associated with reduced mortality risk among older adults? Pers Individ Dif 2020;154:109668. [Crossref]
- Becker H, Stuifbergen A. What makes it so hard? Barriers to health promotion experienced by people with multiple sclerosis and polio. Fam Community Health 2004;27:75-85. [Crossref] [PubMed]
- Zhao G, Okoro CA, Hsia J, et al. Prevalence of disability and disability types by urban-rural county classification-U.S., 2016. Am J Prev Med 2019;57:749-56. [Crossref] [PubMed]
- Bodai BI, Nakata TE, Wong WT, et al. Lifestyle medicine: a brief review of its dramatic impact on health and survival. Perm J 2018;22:17-025. [PubMed]
- Bredesen DE. Reversal of cognitive decline: a novel therapeutic program. Aging (Albany NY) 2014;6:707-17. [Crossref] [PubMed]
- Jones M, Morris J, Deruyter F. Mobile healthcare and people with disabilities: current state and future needs. Int J Environ Res Public Health 2018;15:515. [Crossref] [PubMed]
- Zhou L, Parmanto B. Reaching people with disabilities in underserved areas through digital interventions: systematic review. J Med Internet Res 2019;21:e12981. [Crossref] [PubMed]
Cite this article as: Rimmer JH, Wilroy J, Galea P, Jeter A, Lai BW. Retrospective evaluation of a pilot eHealth/mHealth telewellness program for people with disabilities: Mindfulness, Exercise, and Nutrition To Optimize Resilience (MENTOR). mHealth 2022;8:15.



