
Home blood pressure measurement self-reporting in real-life practices using the Hy-Result app: self-monitoring and digital pathway
Highlight box
Key findings
• Hy-Result web app database [510,983 systolic blood pressure (BP) and diastolic BP readings collected in real life circumstances] shows that 90% of the home BP measurement (HBPM) reports include the required minimum number of BP readings to allow the calculation of a reliable BP average.
• From 17,289 HBPM sequences of more 15 consecutive BP readings, 40% have uncontrolled BP levels.
What is known and what is new?
• Digital tools improve self-management
• The Hy-Result web app reinforces the patient’s engagement to independently monitor and self-reported their BP. The Hy-Result database may serve as a public health tool.
What is the implication, and what should change now?
• When the mean BP is not within the recommended range, the users are automatically prompted by automatic text messages to seek medical advice by the software. Further studies are needed to demonstrate the benefice of this information in lowering BP.
Introduction
There is growing evidence that the information and communication technologies (ICTs) and home blood pressure measurement (HBPM) can improve health care access, patient education, compliance to treatment and outcomes, particularly in chronic diseases such as arterial hypertension (1-3). However, little real-life information is available on the clinical characteristics of ICT users, particularly in the context of hypertension and HBPM. In this e-Health context, our group validated previously, a software system named Hy-Result®, to help patients and professionals in the management of HBPM (4-6). The patients’ reported data collected by the system give an original look on real life practices in the use of eHealth tools and HBPM. The aim of this study is to describe user’s HBPM practices in real-life circumstances through data collected by the Hy-Result® system.
Methods
Software
Hy-Result is a validated system. A first study evaluated whether the algorithm classification of the blood pressure (BP) status was in accordance with the physician’s classification (blinded to the software’s results) following a consultation (n=195 patients) and shows that classification by Hy-Result is similar to that of a specialist in current practice (4). A second, study assessed the experience of patients with the functionalities and medical content of Hy-Result, their feelings and expectations, and the impact of Hy-Result on the physician-patient relationship. It concluded that most of the users (n=512) described Hy-Result as an easy-to-use and useful tool (5). Additional study shows that the majority (88%) of pregnant women (n=107) performed HBPM and successfully used the Hy-Result software for self-interpretation of the BP readings (6).
Hy-Result is designed to help patients to: (I) perform HBPM according to a standardized protocol; (II) understand their results; and (III) share his/her BP readings with their doctor or nurse in a PDF format report (4-6). The data is generated through the Hy-Result web interface using a home conventional oscillometric monitor (with an upper-arm or a wrist cuff) and following an eHealth self-management protocol in accordance with the European Society of Hypertension (ESH) guidelines (2,7).
After measuring their BP according to the Hy-Result protocol (sitting position, three measurements 1 or 2 minutes apart, morning and evening for 3 to 7 consecutive days), the patient connects to “hy-result.com” enters their systolic BP (SBP) and diastolic BP (DBP) in the web interface and provides their medical profile (characteristics taken into account by the Hy-Result algorithm, Table 1). After clicking the “calculate” button, the software automatically generates a PDF analysis report using the Hy-Result® algorithm. This PDF report reconstructs the data in the form of graphs (Figure 1) and text messages written in user-friendly language (Appendix 1) and color-coded. Table 2 summarizes the classification of color codes. When the mean BP is not within the recommended range, the users were automatically prompted by text messages to seek medical advice by the software. The data (medical profile + BP measurements) are recorded anonymously in a secure database.
Table 1
| Question | Response |
|---|---|
| Gender | Male/female |
| Age (years) | 18 to 90 |
| Height (cm) | 60 to 210 |
| Weight (kg) | 30 to 140 |
| Undertaking antihypertensive treatment | Yes/no |
| Current smoker | Yes/no |
| Number of alcohol drinks per day (glass) | 0 to 5 or more |
| Past medical history of stroke | Yes/no/I don’t know |
| Diabetes | Yes/no/I don’t know |
| Chronic kidney disease | Yes/no/I don’t know |
| Use of contraceptive pills | Yes/no |
| Pregnancy | Yes/no |
Table 2
| Hy-Result® color code | Classification |
|---|---|
| Gray | Without treatment: SBP ≤100 mmHg |
| Treated hypertension: SBP ≤115 mmHg or DBP ≤65 mmHg | |
| Green | SBP 101–135 mmHg and DBP 66–85 mmHg |
| Orange | SBP 136–150 mmHg and/or DBP 86–100 mmHg |
| Red | SBP ≥151 mmHg and/or DBP ≥101 mmHg |
SBP, systolic blood pressure; DBP, diastolic blood pressure.
Study design and data collection
This is a retrospective observational study conducted using Hy-Result® database between November 2021 and October 2022. We collected, in our secure database, 21,158 reports compiled in an Excel file format. Each report corresponds to a set of self-measurement sequences (1 to 7 consecutive days), recorded by one user.
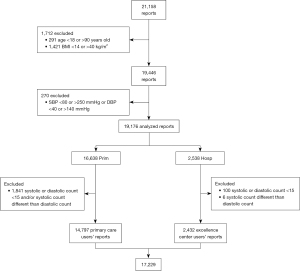
For analysis, we included patients aged between 18 and 90 years. Because the usual practice of HBPM is accompanied by aberrant values due to malfunctions of BP monitoring and/or users input errors, we excluded 270 reports (1.4%) with aberrant values defined as follows: DBP <40 or >140 mmHg; SBP <80 or >250 mmHg. (These thresholds are arbitrary but mainly based on the technical limitations of some devices. Above these ranges of readings, automatic analysis by the software is questionable without verification of monitor reliability, measurement procedure quality, and clinical information. Since such verification is impossible, we prefer to exclude such extreme values, which constitute a tiny minority of the data, to avoid any hazardous interpretations). The software cannot differentiate between an aberrant value which is due to a tensiometer’s technical problem or a manual input mistake (misreporting). We also excluded patients with a body mass index lower than 14 kg/m2 or higher than >40 kg/m2 because of the risk of error measurements due to unadapted cuff size. Overall, we analyzed 19,176 HBPM reports collected in real life circumstances from French users (see flow chart, Figure 2). The Hy-Result database totaled 510,983 SBP and DBP readings.
The characteristics and medical history are self-declared by users: age; gender; the use or not of antihypertensive treatment; history of diabetes, stroke, chronic kidney disease; the use of oral contraception; current pregnancy; current tobacco use; number of alcohol drinks per day (Table 1). A user is considered hypertensive if he declares taking an antihypertensive drug. Two groups of users are differentiated according to the source of recruitment, primary care (Prim), or hypertension center (Hosp) of an ESH excellence center:
- Prim users: this group is composed of health consumers who find the website by themselves on the Internet (hy-result.com) or patients following the recommendation of their physician (e.g., general practitioner or cardiologist). For this group, we are not aware of the existence of any self-measurement education input. However, we do know, that they followed the instructions given by the system because otherwise they could not complete the web interface and fill in their BP measurements.
- Hosp users: this group corresponds to those who use the web application as per the recommendation of a physician who works in an ESH excellence center (Georges Pompidou European Hospital, Paris, France). In this center, patients are instructed on how to correctly measure their home BP by a nurse and they receive a 4-page leaflet that explains how to use the Hy-Result® web interface which is designed for self-management use. (The leaflet is also available online in PDF format). To use the software, these patients did not receive any subsequent help from a health professional.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics Version 26.0 and conducted between January and April 2023. Categorical variables were summarized as frequency and percentage. Continuous variables were presented as mean, standard deviation (SD), median, minimum, and maximum. Shapiro test was used to test the normality of continuous variables. This test is used to determine if two categorical variables are independent or if they are related to one another. In this study, we used the t-test to assess the significance of differences in mean values between two independent groups, while the Pearson correlation coefficient was employed to evaluate the strength and direction of relationships between two continuous variables. An aberrant value is defined by having either a SBP <80 or >250 mmHg or a DBP <40 or >140 mmHg. A manual input error is defined if any of the following occurs: (I) error count: the SBP count is different than the DBP.
Both international hypertension and HBPM guidelines recommend performing a minimum number of BP measurements over a few days to obtain an accurate and a reproducible estimate of the average BP values. A minimum of 12 SBP and 12 DBP readings, taken on 3 (consecutive) days, are needed for the reproducibility of HBPM to be superior to that of conventional measurements (8,9). In our study, BP levels are analyzed in the subgroup of reports having a minimum of 15 SBP and 15 DBP in accordance with the French guidelines recommending three measurements morning and evening.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Before using the app, users agreed to the use of their data for research purposes (app’ user agreement). According to French law, IRB approval was waived for the study of a completely anonymous database. Data collection, storage and processing complied with European General Data Protection Regulations (GDPR).
Results
A total of 19,176 reports are analyzed (Figure 2). The database provides medical information on the users (age, gender, cardiovascular risk factors, and cardiovascular events), BP levels, compliance—or not—with the measurement protocol and the types of sphygmomanometers used (arm or wrist). For BP level reliable analysis, we then excluded patients with systolic or diastolic count <15 and users with a systolic count different from the diastolic count. We ended up with 17,229 reports (14,797 reports of Prim users and 2,432 reports for patients followed-up in an ESH excellence center).
Population
Of the 19,176 reports, 63.2% declare receiving antihypertensive medication (n=12,117). In this group, the mean ± SD age is 64±12 years of whom 60.7% are male (n=7,350). Diabetes, chronic kidney disease, and stroke are declared in 15.2%, 9.7%, and 7.6%, respectively (n=1,843, 1,171, and 918, respectively) (Table 3). Untreated group is younger with a mean ± SD age of 58±14 years and with a lower prevalence of comorbidities (Table 3). When comparing reports from treated patients in the Prim vs. Hosp group, we find that the first group is older with a mean ± SD age of 65±11 vs. 58±14 years. Fewer have chronic kidney disease and stroke [8.2% (n=829) and 7.2% (n=723) vs. 16.6% (n=342) and 9.5% (n=195), respectively]. The prevalence of diabetes is slightly higher in the prim group [15.5% (n=1,556) vs. 13.9%] (Table 4).
Table 3
| Characteristics | Treated group | Untreated group | P value |
|---|---|---|---|
| Total | 12,117 (63.2) | 7,059 (36.8) | NA |
| Age (years) | 64±12 | 58±14 | <0.001 |
| Gender | <0.001 | ||
| Male | 7,350 (60.7) | 3,801 (53.8) | |
| Female | 4,767 (39.3) | 3,258 (46.2) | |
| BMI (kg/m2) | 27.2±4.3 | 26.5±4.2 | 0.02 |
| Current smoking | 774 (6.4) | 688 (9.7) | <0.001 |
| Alcohol | 0.12 | ||
| 0 glass/day | 7,451 (61.5) | 4,458 (63.2) | |
| >5 glasses/day | 43 (0.4) | 23 (0.3) | |
| Diabetes | 1,843 (15.2) | 561 (7.9) | <0.001 |
| Chronic kidney disease | 1,171 (9.7) | 240 (3.4) | <0.001 |
| Stroke | 918 (7.6) | 347 (4.9) | <0.001 |
Data are presented as n (%) or mean ± SD. NA, not available; BMI, body mass index; SD, standard deviation.
Table 4
| Factors | Hosp (ESH excellence center; n=2,538, 13.2%) | Prim (n=16,638, 86.8%) | |||||
|---|---|---|---|---|---|---|---|
| Treated | Untreated | P value | Treated | Untreated | P value | ||
| Total | 2,058 (81.1) | 480 (18.9) | NA | 10,059 (60.5) | 6,579 (39.5) | NA | |
| Age (years) | 58±14 | 55±16 | <0.001 | 65±11 | 59±14 | <0.001 | |
| Gender | <0.001 | <0.001 | |||||
| Male | 1,265 (61.5) | 247 (51.5) | 6,085 (60.5) | 3,554 (54.0) | |||
| Female | 793 (38.5) | 233 (48.5) | 3,974 (39.5) | 3,025 (46.0) | |||
| BMI (kg/m2) | 26.9±4.4 | 25.5±4.2 | <0.001 | 27.2±4.3 | 26.6±4.2 | 0.09 | |
| Tobacco | 155 (7.5) | 49 (10.2) | 0.05 | 619 (6.2) | 639 (9.7) | <0.001 | |
| Alcohol | 0.008 | 0.004 | |||||
| 0 glass/day | 1,426 (69.3) | 328 (68.3) | 6,025 (59.9) | 4,130 (62.8) | |||
| >5 glass/day | 6 (0.3) | 0 (0.0) | 33 (0.3) | 15 (0.2) | |||
| Diabetes | 287 (13.9) | 33 (6.9) | <0.001 | 1,556 (15.5) | 528 (8.0) | <0.001 | |
| Chronic kidney disease | 342 (16.6) | 68 (14.2) | 0.18 | 829 (8.2) | 172 (2.6) | <0.001 | |
| Stroke | 195 (9.5) | 34 (7.1) | 0.10 | 723 (7.2) | 313 (4.8) | <0.001 | |
Data are presented as n (%) or mean ± SD. Hosp, hypertension center; Prim, primary care; ESH, European Society of Hypertension; NA, not available; BMI, body mass index; SD, standard deviation.
Numbers of readings and compliance with the HBPM schedule
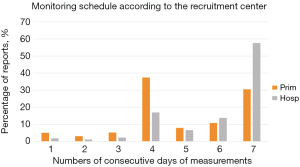
Web app instructions are: “Measure your BP for 3 to 7 days in a row and fill the table”. Table 5 shows the total numbers of readings per report. The large majority of reports (90.2%, n=17,289) totaled 15 BP readings or more, among which 96.1% were Hosp users (n=2,438) and 89.3% were Prim users (n=14,851) with a significant difference between the groups (P<0.001). Figure 3 compares compliance with the HBPM schedule regarding the number of consecutive days of measurements between the centers of recruitment: 5% of Prim users (n=830) vs. 1.8% of Hosp users (n=46) did less than six measurements. We collected 17,229 reports with at least 15 measurements. In this subgroup, the compliance rate for 7 measurements days was higher in the Hosp group with 57.6% (n=1,463) vs. 30.5% (n=5,081).
Table 5
| Subgroups | BP readings per report | P value | |
|---|---|---|---|
| ≤14 | ≥15 | ||
| Hosp (n=2,538) | 100 (3.9) | 2,438 (96.1) | <0.001 |
| Prim (n=16,638) | 1,787 (10.7) | 14,851 (89.3) | |
Data are presented as n (%). BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure; Hosp, hypertension center; Prim, primary care.
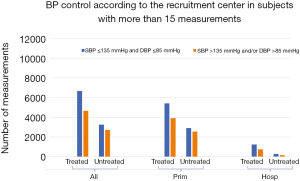
BP levels
Figure 4 presents the achievement of BP control (threshold of 135/85 mmHg, as defined by ESH guidelines), according to patients’ groups (Prim or Hosp) among treated and untreated users. To ensure reliability in our analysis, we focused on examining a subgroup consisting of 17,289 reports that included at least 15 BP measurements. In this subgroup, 42.7% (n=7,378) had an average SBP and/or DBP above the recommended thresholds (below 135 and/or 85 mmHg), among whom, 36.8% were untreated subjects (n=2,716). Users that are followed in the ESH excellence Hosp had better BP control than those in a Prim setting (P<0.001).
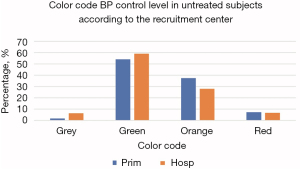
To facilitate patient understanding, the Hy-Result algorithm classifies SBP and/or DBP averages into four color codes (gray corresponds to low pressures, normal to green, and orange or red to pressures above thresholds). Figure 5 and Figure S1 show the repartition of color code according to the BP levels. Patients’ cardiovascular risk factors of normal or low BP (gray color code) are summarized in Table 4. In this group, 93.5% are treated patients (n=1,606).
HBPM oscillometric devices
Upper arm cuff devices were used in 80.7% of Prim users (n=13,628) and in 93.1% of Hosp users (n=2,318), with a significant difference (P<0.001). In both groups, treated patients used the recommended arm cuff more frequently than the untreated users (Table S1).
Discussion
Strengths and limitations
The analyzed data relates to 19,176 reports totaling 510,983 SBP and DBP readings. It offers a large-scale quantitative observation on HBPM practices in a real-life setting. This retrospective examination of the Hy-Result database provides a unique insight into the behavior of two groups as they self-measure their BP at home using their personal devices and engage with ICT through a web interface, all without the supervision of healthcare professionals. The methodology employed here does not introduce any clinical trial bias. Clinical trials based on HBPM typically differ from real-life scenarios due to differences in inclusion criteria, the requirement for consent, and the presence of instructions, which can vary from providing information or education to occasionally supplying study-specific monitors. Therefore, this retrospective analysis without intervention is a good way of observing real-life behaviors. We acknowledge limitations stem from the technical characteristics of the software: because it is anonymous, the data does not distinguish between the number of reports and the number of users; each user does not have a single ID to log in; therefore, if a user enters multiple sets of HBPM, we will collect multiple reports in our database that cannot be identified as belonging to the same user. In other words, the 19,446 reports do not correspond exactly to 19,446 users. The data do not provide information how patients interact with the program, particularly BP submissions at repeated intervals over time. This information will be available in a new version of the software.
Population
The distribution of the age, gender ratio and BMI of the Hy-Result® system users is consistent with the epidemiological knowledge observed in France where the prevalence of hypertension is higher in men than in women (34% vs. 28%) and increases with age (10). The same is true for the population attending an ESH excellence center, which is younger than that of a Prim setting. It is consistent to note that the patients under antihypertensive medication are older and suffer from a higher rate of comorbidities (diabetes, chronic kidney disease, and/or stroke) than those untreated. It is important to note that patients who perform HBPM and use a digital tool are not representative of the general population. In France, only 20.9% of the Esteban study adult population possess a HBPM device (10).
BP levels
On the one hand, our study finds that approximately half (43%) of the reports of treated patients do not have BP levels under control; this is consistent with other studies that show that the control rate among the hypertensive population is estimated between 40% to 50% in Europe (11). In France, a national study shows that among those treated, 45% had uncontrolled BP (55% in men and 33.5% in women) (12,13). On the other hand, a significant proportion (41%) of the reports are generated by untreated subjects. This is original data for which we lack comparison in the literature.
Uncontrolled BP levels
In our population, 45.4% of untreated patients have uncontrolled BP levels. However, our data do not allow us to know whether self-measurement is carried out as part of a self-screening process or at the request of a health professional to diagnose hypertension. In the Hosp group, the proportion of hypertension without treatment is 35.9%. These are patients in whom the healthcare professional was looking for white coat hypertension (WC-HTN) or patients whose treatment had been temporarily stopped to allow exploration (such as hormonal dosage of renin and aldosterone levels for example). Assuming that people consulting a tertiary center have had previously observed high BP at some time in the past, the percentage of 35.1% could correspond to that of the white coat effect. Although our hypothesis is fragile, this rate is plausible since data from the literature suggest that 20% to 40% of patients initially diagnosed as hypertension may have WC-HTN even if it is impossible to posit a precise number due to variation in different populations (as Prim vs. Hosp center) (14). In a Prim setting, a study found a prevalence of 39% of WC-HTN (15).
Low BP level
The Hy-Result algorithm cut-off for the gray color code is 115/65 mmHg which corresponds to the lower BP target as per the ESH 2023 guidelines (7). These guidelines indicate that an office SBP <120 mmHg and DBP <70 mmHg cannot be recommended in several situations such as diabetes mellitus or chronic kidney disease). In our study, 8.3% of the treated population have a low BP level. Are these patients (Figure S1) over treated? To answer we should consider the patients’ tolerance and orthostatic hypotension. To answer this question, we need to consider patient tolerance and orthostatic hypotension. Unfortunately, these data are not available with a sitting measurement. In these cases (gray zone classification), text messages invite users to check their BP with their doctor.
HBPM oscillometric devices
Hy-Result’ users web app declare that they mostly use brachial rather than radial cuff devices (80% in the Prim group and 93% in the Hosp group). This is probably because patients followed up in an ESH excellence center are trained in the proper protocol for HBPM. These proportions are higher than those found in the FLAHS survey, which estimates that half of treated hypertensive patients are equipped with brachial cuff-type BP monitors, whereas in subjects without treated hypertension, wrist monitors are used in the majority of cases (16). In France, the distribution of arm or wrist BP monitors sold in pharmacies was identical (17). The instructions provided through the Hy-Result app advise patients against using wrist devices. This is a necessary information since BP monitors can be bought without the guidance of a health provider (i.e., supermarkets or Internet).
HBPM schedule
Having a reliable HBPM is crucial because correct BP measurement is a prerequisite for appropriate medical decision-making (diagnosis and/or drug titration). Healthcare providers are concerned about the low adherence to self-measured BP monitoring schedules by patients (18,19). The monitoring schedule and protocol might be poorly explained by health professionals. According to a French study, only 17% of general practitioners teach their patients how to perform standardized HBPM (20). The Hy-Result app is designed to help patients to respect the recommended schedule. Overall, the vast majority (90%; n=17,289) of Hy-Result reports include the minimum number of measurement days required by the ESH guidelines (2,7). This rate reaches 96% for Hosp group which has received specific training from a nurse.
The value of 90% derives from a select, motivated and willing subset of individuals. Website traffic statistics show that of all visitors to the home page, roughly two-thirds enter their BP readings to calculate their average BP (first step). Half of them proceed to the second and final step (by completing their medical profile, entering their BP results, and clicking the “calculate” button). In a previous pilot study, we observed that 54% (n=304) of the new patients who booked via the Internet an appointment at our Hosp were able to prepare for their visit by going through a digital pathway and following the application’s instructions for use (21).
HBPM and provider-perceived barriers
Healthcare providers highlight that the increased use of HBPM monitoring, along with education and communication, will affect their daily practice (staff workload, telephone calls, email messages, etc.). They are also concerned about the extra time needed for interpreting self-measured BP readings (19). For these reasons, the Hy-Result app was designed for a self-management approach, as distinct from a telemonitoring approach (22).
Electronic oscillometric devices require little to no training and are generally not affected by an observer bias; if used correctly (23). The app automatically calculates SBP and DBP averages and classifies them into four color zones in accordance with the ESH guidelines. Manual input of readings may be sometimes wrong (misreporting), but on average, possible errors in notation had almost no influence on the mean BP, as shown in a study with a memory-equipped electronic device (24). Database shows that 90% of the HBPM reports include the required minimum number of BP measurements to allow the calculation of a reliable average. According to a pilot study in our tertiary center, approximately half of the patients (54%) were able to successfully negotiate the Digital Path with either Hy-Quest and/or Hy-Result completed (5 days self-measurement minimum) (21).
Conclusions
In conclusion, our real-life study shows that 90% of the HBPM reports include the required minimum number of BP readings to allow the calculation of a reliable average among whom 40% have uncontrolled BP levels. The self-management Hy-Result web app demonstrates significant potential for inclusion in the patient care process and reinforces the patient’s engagement to independently monitor and self-reported their BP.
Acknowledgments
We express our great gratitude to Association Robert Debré Pour la Recherche Médicale (ARDRM), Fondation de l’Avenir, University Faculté de Médecine Paris V, French Society of Hypertension (SFHTA).
Funding: None.
Footnote
Data Sharing Statement: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-66/dss
Peer Review File: Available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-66/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://mhealth.amegroups.com/article/view/10.21037/mhealth-23-66/coif). N.P.V. serves as an unpaid editorial board member of mHealth from December 2022 to November 2024. N.P.V. reports that the Hy-Result application is certified by the French Society of Hypertension (SFHTA). Its development is supported by two non-profit organizations (Association Robert Debré Pour la Recherche Médicale, Fondation de l’Avenir) and university (Faculté de Médecine Paris V); it is free of charge and generates no revenue. N.P.V., as one of the academic authors, does not receive any remuneration. A.L. receives payments from Bayer for speaker bureau and lectures and Astrazeneca for presentations. R.A. receives payments for grants from Omron (Japan) and Servier (France), payments for consulting from Axelife (France), payments for lectures from Omron, Recordati, Boehringer, payments for meetings from Recordati, Omron, and payments for equipment from Omron. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Before using the app, users agreed to the use of their data for research purposes (app’ user agreement). According to French law, IRB approval was waived for the study of a completely anonymous database. Data collection, storage and processing complied with European General Data Protection Regulations (GDPR).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Postel-Vinay N, Bobrie G, Savard S, et al. Home blood pressure measurement and digital health: communication technologies create a new context. J Hypertens 2018;36:2125-31. [Crossref] [PubMed]
- Parati G, Stergiou GS, Bilo G, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the Working Group on Blood Pressure Monitoring and Cardiovascular Variability of the European Society of Hypertension. J Hypertens 2021;39:1742-67. [Crossref] [PubMed]
- McManus RJ, Mant J, Franssen M, et al. Efficacy of self-monitored blood pressure, with or without telemonitoring, for titration of antihypertensive medication (TASMINH4): an unmasked randomised controlled trial. Lancet 2018;391:949-59. [Crossref] [PubMed]
- Postel-Vinay N, Bobrie G, Ruelland A, et al. Automated interpretation of home blood pressure assessment (Hy-Result software) versus physician's assessment: a validation study. Blood Press Monit 2016;21:111-7. [Crossref] [PubMed]
- Postel-Vinay N, Steichen O, Pébelier E, et al. Home blood pressure monitoring and e-Health: investigation of patients' experience with the Hy-Result system. Blood Press Monit 2020;25:155-61. [Crossref] [PubMed]
- Postel-Vinay N, Shao JD, Pinton A, et al. Home Blood Pressure Measurement and Self-Interpretation of Blood Pressure Readings During Pregnancy: Hy-Result e-Health Prospective Study. Vasc Health Risk Manag 2022;18:277-87. [Crossref] [PubMed]
- Mancia G, Kreutz R, Brunström M, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens 2023;41:1874-2071. Erratum in: J Hypertens 2024;42:194. [Crossref] [PubMed]
- Stergiou GS, Skeva II, Zourbaki AS, et al. Self-monitoring of blood pressure at home: how many measurements are needed? J Hypertens 1998;16:725-31. [Crossref] [PubMed]
- Groenland EH, Bots ML, Visseren FLJ, et al. Number of measurement days needed for obtaining a reliable estimate of home blood pressure and hypertension status. Blood Press 2022;31:100-8. [Crossref] [PubMed]
- Vallée A, Gabet A, Grave C, et al. Patterns of hypertension management in France in 2015: The ESTEBAN survey. J Clin Hypertens (Greenwich) 2020;22:663-72. [Crossref] [PubMed]
- Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021;398:957-80. [Crossref] [PubMed]
- Perrine AL, Lecoffre C, Blacher J, et al. L’hypertension artérielle en France: prévalence, traitement et contrôle en 2015 et évolutions depuis 2006. Bull Epidémiol Hebd 2018;170-9.
- Olié V, Grave C, Gabet A, et al. Épidémiologie de l’hypertension artérielle en France: prévalence élevée et manque de sensibilisation de la population. Bull Épidémiol Hebd 2023;130-8.
- Kuritzky L. White coat hypertension: addressing the 10 most important questions. Curr Cardiol Rep 2012;14:678-83. [Crossref] [PubMed]
- Martínez MA, García-Puig J, Martín JC, et al. Frequency and determinants of white coat hypertension in mild to moderate hypertension: a primary care-based study. Monitorización Ambulatoria de la Presión Arterial (MAPA)-Area 5 Working Group. Am J Hypertens 1999;12:251-9. [Crossref] [PubMed]
- Fondation Recherche sur l’Hypertension Artérielle. Flash study. Available online: https://frhta.com/
- Data from IMS Pharmatrend Micro© 2021.
- Kronish IM, Kent S, Moise N, et al. Barriers to conducting ambulatory and home blood pressure monitoring during hypertension screening in the United States. J Am Soc Hypertens 2017;11:573-80. [Crossref] [PubMed]
- Shimbo D, Artinian NT, Basile JN, et al. Self-Measured Blood Pressure Monitoring at Home: A Joint Policy Statement From the American Heart Association and American Medical Association. Circulation 2020;142:e42-63. [Crossref] [PubMed]
- Dugelay G, Kivits J, Desse L, et al. Implementation of home blood pressure monitoring among French GPs: A long and winding road. PLoS One 2019;14:e0220460. [Crossref] [PubMed]
- Postel-Vinay N, Gardini M, Nogueira L, et al. Digital path of the hypertensive patient before a first visit in a tertiary care hypertension unit: a real-life pilot study. J Hypertens 2021;39:e217. [Crossref]
- Postel-Vinay N, Bobrie G, Asmar R, et al. Management of arterial hypertension: home blood pressure measurement is a cornerstone for telemonitoring and self-management. Mhealth 2023;9:18. [Crossref] [PubMed]
- Asmar R, Kollias A, Palatini P, et al. Devices for Home Blood Pressure Monitoring. In: Stergiou G, Parati G, Mancia G. editors. Home Blood Pressure Monitoring. Updates in Hypertension and Cardiovascular Protection. Cham: Springer; 2020:1-12.
- van der Hoeven NV, van den Born BJ, Cammenga M, et al. Poor adherence to home blood pressure measurement schedule. J Hypertens 2009;27:275-9. [Crossref] [PubMed]
Cite this article as: Postel-Vinay N, Gebara N, Asmar R, Stephan D, Lorthioir A, Amar L. Home blood pressure measurement self-reporting in real-life practices using the Hy-Result app: self-monitoring and digital pathway. mHealth 2024;10:13.



