Are we there yet?!—a literature review of recent digital technology advances for the treatment of early psychosis
Introduction
Psychosis refers to a group of mental health conditions that affect a person’s thoughts, feelings and behavior and it is mainly characterised by hallucinations, delusions, thought disorder, negative symptoms and bizarre behaviour. It is considered one of the most impairing mental health disorders where for a significant portion of the course of the illness, the individual’s social and occupational functioning is markedly below the level achieved prior to the onset. The pre-psychosis period is the time interval between the first noticeable changes in behaviour, to the appearance of overt psychotic symptoms of diagnosable psychosis (also named full-blown psychosis) and it is called “clinical high risk” (CHR) (1). At this stage, many have already experienced a loss of cognitive and psychosocial functioning (2). The prodromal state period, which on average can last days up to 5 years (3), is a precious time to initiate treatment towards better prognosis as research has shown that reducing the duration of untreated psychosis (DUP) equipoised the effect of earlier disorder onset as a poor prognosis factor (4). Following the clinical staging model proposed by McGorry and colleagues [2006], where CHR encompasses stage I (subdivided into three sub-stages ‘a’ to ‘c’), after CHR comes stage II or full threshold first-episode of psychosis (FEP). It is considered the first acute phase or crisis, characterised by florid psychotic symptoms [sustained symptoms lasting four weeks or more as suggested by the NICE Quality standard 102 (5)], and it is often detected by primary care physicians, emergency departments, welfare agencies, specialist care agencies, or drug and alcohol services (6). Early interventions during stage II have also been shown to improve the outcome of FEP through DUP reduction, improvement of treatment response, well-being and social functioning as well as secondary prevention of illness progression [stage III, (7)]. Therefore, early detection and initial treatment strategy of CHR of psychosis and FEP has become a major goal of mental health services in order to delay the onset of full-blown psychosis, reducing unnecessary suffering and increasing the possibility of improved long-term outcomes (8). Early intervention for psychosis services (EIS), focusing on the special needs of young people and their families, are being implemented worldwide aiming to offer psychological and pharmacological interventions. Although preventive treatment altering the course of the illness (i.e., at CHR stage) and specialised comprehensive interventions for FEP can significantly improve disorder outcomes and their implementation is recommended (7), there are still some challenges to overcome. Main challenges include reaching individuals not accessing mental health services in order to improve detection of at-risk cases, optimising interventions and adapting them to young people new forms of communication, increasing the focus on social recovery instead of only ameliorating positive symptoms, or achieving long-term outcomes.
Digital technologies offer new opportunities for improving psychological interventions in an engaging and tailored way, as well as providing novel therapeutic contexts within which core psychological processes can be targeted in real time with immediate feedback. They can be more attractive and compelling to young people, offering them new forms of social interactions (e.g., on-line forums), flexible ways to access information and facilitating self-management (e.g., mobile apps and digital diaries) and delivering ecological valid treatments (e.g., exposure-based interventions using social virtual environments). One of the more promising technologies is virtual reality (VR). VR can be defined as technology that integrates real-time computer graphics, sounds and other sensory input to create a computer-generated world with which the user can interact (9). The ecological validity of this approach is strengthened by the sense of presence (the psychological sensation of “being there”) that individuals can experience in virtual environments (10). A key advantage of VR is that it offers researchers and clinicians the possibility not only of observing the user’s real-time behaviour when interacting with virtual agents, but also of controlling and modifying the environment and the responses of the avatars or simulated stimuli and tasks (11). The use of VR and avatars in the assessment and treatment of several dimensions of psychotic symptoms is promising (12), although research is limited to adult populations.
There is also a growing body of work and research exploring the potential of smartphone technologies to enhance therapy outcomes, improve medication adherence, and to promote self-management for people with psychosis. Mobile software applications (“apps”), sometimes combined with wearable devices (wrist band, watch or clothes connected to the phone gathering physiological information for extended periods), are the most common form of smartphone technology, also known as mHealth (or mobile Health). Smartphone technology has the potential to significantly improve mental healthcare, through extending the reach of services and providing adjunctive support to existing psychosocial interventions (13). A recent meta-analysis showed that more than 65% of people with psychosis own a smartphone, with an increase up to the 81% in the last decade, and that the majority of users are in favour of using mobile phones (>60%) to track or monitor their mental health (13). Mobile apps are providing a new form of the classic structured diary techniques in the form of momentary assessments, such as the Experience Sampling Method (ESM) (14) or Ecological Momentary Assessment (EMA) (15), defined as naturalistic methods to distribute surveys that individuals complete in the context of everyday life. Additionally, these methods have the advantage that the information is collected digitally and in real-time, using the person’s own device, and can be shared with the authorised clinician’s web-based dashboard (16). These forms of assessment can contribute to identifying the person’s individual risk factors or symptom patterns and identify treatment goals (17,18). Feedback on change in real time may then facilitate behavioural changes and improve therapy generalisation into the person’s daily life.
The utilization of the internet as a source of information and support for people with psychosis and their relatives has also grown considerably (19), with the potential to significantly influence health related behaviors and decisions as well as the clinician-patient relationship (20). People with psychosis use the Internet and are able and willing to use mental health services on-line (e.g., peer-to-peer support) (21). The internet provides a great opportunity to deliver cost-effective and highly accessible interventions, independent of time and place at a self-determined pace. Results from a systematic review conducted by Alvarez-Jimenez and colleagues [2014] supported the acceptability and feasibility of internet-based interventions, with several studies providing encouraging preliminary results regarding their clinical and psychosocial potential (22).
Digital technology has the potential for radical change in terms of service delivery and development of new treatments (23) and health care providers around the world are adopting and adapting digital solutions to improve current challenges, such as long waiting times to access interventions and enhancement of existing therapies’ outcomes. The aim of the present literature review is to summarise main findings of relevant studies published during the last 10 years on the utilization of digital technologies (i.e., virtual reality, smartphone technology and web-based interventions) to enhance psychological treatment outcomes in early psychosis.
Methods
Search criteria
The database used to conduct the search was PubMed. Studies for review were identified following a keyword search for the terms ‘virtual reality’ OR ‘VR’ OR ‘smartphone’ OR ‘mobile-app’ OR ‘Internet-based’ OR ‘Web-based’ AND ‘clinical high risk for psychosis’, OR ‘ultra high risk for psychosis’ OR ‘first episode of psychosis’, OR ‘early psychosis’, OR ‘early intervention services’, from January 2009 to the 7th of June 2019.
Study selection
For the purpose of this review, three forms of digital technologies were selected: VR, mobile and internet-based interventions. Based on Rus-Calafell et al. [2017], VR based interventions were defined as interventions using immersive and interactive VR environments in three-dimensional (3D) graphics presented with a head-mounted display, or that they used 2D graphics on a computer screen but were interactive, meaning that participants could navigate through the environment using either a joystick or mouse/keyboard and where they would find sufficient elements in to interact with and had some feedback from (as a response of the interaction). Following Alvarez-Jimenez et al. [2014], internet-based interventions were defined as web-based interventions enabling peer-to-peer contact, patient-to-expert communication or interactive psycho-education/therapy; mobile-based interventions were defined as interventions delivered via mobile phones using SMS, MSS, mobile or web-applications.
Considered for inclusions were studies examining the usability, feasibility, acceptability or efficacy of user-centered, VR, smartphone or Internet-based psychological interventions, including participants meeting CHR for psychosis criteria, FEP criteria and/or interventions directed exclusively to individuals registered with early intervention for psychosis services (EIS).
Studies were included in the review if they: were written in English; contained original empirical findings, and were published in a peer-reviewed journal. In case of protocols’ publications, they were included only if trial outcomes were not yet published or if they differed considerably from previous pilot work from the same group. Studies were excluded from the review if they were assessment or observational studies; family-centered interventions; symptom monitoring not part of a psychological intervention or without personalized advice; reviews; not available in English; letters to editors; theses; or book chapters.
Research findings
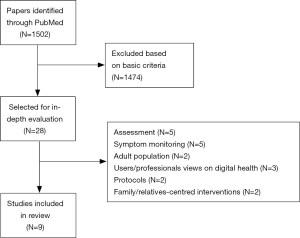
The initial screening (title and abstract) of 1,502 papers resulted in 28 articles being selected for in-depth evaluation. Majority of papers not selected for in-depth evaluation discussed cross-sectional results of different demographic and clinical factors associated with early psychosis, longitudinal assessment and transition to psychosis and implementation of early intervention services in different countries. Finally, nine articles were included in the present literature review. Figure 1 illustrates the articles selection process.
Smartphone technology-based interventions
A total of 7 studies exploring the feasibility, acceptability and effectiveness of mobile apps for smartphone to deliver psychological interventions in early psychosis were identified. Table 1 summarises the characteristics of these studies. From these seven studies, only 3 presented actual results of a completed trial (24-26), being only one of these three a single-blind randomised controlled study (24). Results of the three studies confirmed feasibility and acceptability of using mobile-based interventions in early psychosis, including also preliminary evidence for improvement of therapy targets, such as loneliness (25), negative symptoms, general psychotic symptoms and mood (24). Similarly, Lim et al. [2015] and Bucci et al. [2018] included a one training session at the beginning of the intervention to introduce and guide participants on the use of the app domains, contacted the participants by phone once a week, and in both cases engagement with the apps was monetarily incentivized. The two tested interventions are based on different cognitive approaches: positive psychology and cognitive-behavioural model. The App +Connect (25) includes 16 modules based on key concepts of positive psychology (e.g., positive emotions, three good things, gratitude, kindness), with their corresponding tasks and multi-media resources (i.e., shared videos using young people with lived experiences, expert videos featuring therapists or actor videos addressing questions related to interpersonal relationships), that the participants can complete within at least 31 days [see supplementary online resources in (25)]. The Actissist app (27) consists of two main parts: first part, which can be either followed by a prompt from the phone or self-initiated, focus on self-assessment through question answer exchanges on cognitive appraisals, belief conviction, emotions and associated behaviours about suspicious thoughts, voices, getting out, feeling criticised or cannabis consumption. Second part consists of supplementary content with several multi-media options that act in stand-alone fashion design to complement and support the feedback from the intervention. In contrast, Kim and colleagues [2018] included HYM as a continuation phase after completion of a group-Cognitive Behavioural Therapy for psychosis (CBTp) and their app allowed personal communication, real time personal advice and support from clinicians to participants, which also resulted in better case-management (26).

Full table
The rest of studies describe trial protocols, meaning trial results are not reported at this stage. The study by Traber-Walker and colleagues in Switzerland is the only one focusing on individuals at CHR for psychosis (28). Their intervention, Robin, will combine 16 face-to-face sessions with a therapist and a smartphone app that allows integrating contents of the therapy sessions (e.g., goals and specific coping strategies). The intervention follows CBTp and systemic approaches (28). The other smartphone-based intervention following a specific clinical stage framework is proposed by Barbeito et al. [2019] in Spain, focusing on adolescents at FEP stage who will be randomised either to an experimental intervention or treatment as usual condition (29). Those allocated to the experimental condition will have access to an app in addition to treatment as usual. The ThinkApp contains five modules: psychoeducation, recognition of symptoms and relapse prevention, problem-solving techniques, mindfulness and “contact wall” (similar to a forum or social space where users can share interests and experiences supervised by a therapist/moderator).
My journey 3 is the smartphone app designed by Steare and colleagues and it will be tested in a feasibility randomised trial including six EIS for psychosis in North London (30). Those allocated to the experimental intervention will receive one training session on the app and will be allowed to use it for a period of 12 months. The version of the app used in this study includes structured intervention components based on recovery and relapse prevention interventions. Although the number of contacts with clinicians is not controlled in the study, clinicians will be encouraged by the research team to discuss with participants recovery goals and relapse prevention plans in routine appointments and check on app usage. Similarly, Husain and colleagues will test the feasibility of the TechCare app with 12 service userd from the EIS for psychosis in Lancashire (31). The app is based on seminal work by Kingdon & Turkington on CBTp (32) in combination with participant tailored intelligent real-time therapy (iRTT): an intelligent machine learning algorithm which provides techniques in real time based on breach of assessment thresholds and recommendations on the most popular self-help interventions included in the app (e.g., thought-feeling-behaviour relationships, stress models, techniques for managing mood and goal setting).
Internet-based interventions
Two studies discussing the design, implementation and effectiveness of on-line psychological therapy for CHR and FEP individuals were identified in the literature search (33,34). Both interventions have been designed by the same research group in Australia and they focus on the enhancement of the person’s social functioning and social connectedness, as well as too sustain benefits of early intervention beyond discharge from specialist FEP services (33). These two on-line systems, HORYZONS and MOMENTUM, adopt a “Moderate On-line Social Therapy” (MOST) (35) conceptual model which integrates: (I) peer-to-peer on-line social networking; (II) individually tailored interactive psychosocial interventions; and (III) involvement of expert mental health and peer moderators to ensure the safety of the intervention. However, the content of the interventions differs as they target different groups.
HORYZONS includes a first stage where the person is guided through psychoeducation models based on previous work of this group and targeting risk factors for psychosis relapse and salient domains in the early recover process (33). Another essential part of the system is ‘the café’ where users and moderators can post comments, information, upload files and ‘like’ different content. An information wall, which includes activity of individual users, homepage, a ‘job zone’ and other moderated social networking features are other components of the system. This online intervention adopts a positive psychology approach (36) where the users are guided and encouraged to identify, discuss and exercise key personal strengths within the online environment and in real-life to enhance self-esteem, foster social functioning (37) and reduce depression. The results of the pilot study were very encouraging, showing that the online system was feasible, engaging and say and showed preliminary positive effects on social connectedness and empowerment in young people with FEP.
MOMENTUM focus on promoting a circular relationship between wellbeing and functioning: by improving self-efficacy, social support, and subjective wellbeing there will be a reciprocal effect on each other that will motivate the young person to initiate and persist in social activities and improve overall social functioning (34). The interactive therapy modules (or ‘steps’) specifically address: (I) personal strengths, (II) mindfulness and (III) connecting through others. It also includes a moderated online social network (the café) to foster social support and a group problem solving function designed to promote self-efficacy and interpersonal problem solving (‘Talk it Out’). The system allows two type of moderation: expert and peer moderators. Results have shown that MOMENTUM is an engaging and safe on-line system for individuals at CHR for psychosis. Furthermore, results at follow-up have shown significant positive effects on social functioning that have been associated to changes in therapeutic targets such as strengths use, mindfulness skills and social support.
Virtual reality-based interventions
Although the search retrieved some original articles on the utilisation of VR in early psychosis, none of the articles met the inclusion criteria of the present review.
Discussion and clinical implications
To our knowledge, this is the first literature review focusing on psychological interventions using digital technology to treat people within the early clinical stages of psychosis.
Based on the results of the present literature review, the technology that has been wider used and applied to improve psychological treatments in early psychosis is mobile-based interventions, either on the form of blended therapy combining face-to-face therapy with mobile app or as tradition face-to-face therapy delivered and operationalised through smartphones apps. The majority of the studies exploring mobile-based interventions in early psychosis up to this date are protocol studies and feasibility studies with small samples, being the study conducted by Bucci et al. [2018] the only controlled randomised trial. This could be explained by the fact that RCT (considered the gold standard for efficacy testing) are very time-consuming and often do not allow the technology to be changed on the course of the study. This can have a detrimental effect on digital technologies as they require for constant updating and maintaining and can be quickly obsolete. All of the studies included in the present review used different mobile apps that have been design to target psychological mechanisms that may contribute to the onset or maintenance of psychotic symptoms, based on traditional CBT or third wave CBT approaches [described as new developments in CBT which emphasise the relevance of acceptance, mindfulness and emotions, the relationship, values, goals, and meta‐cognition (38)] and in the context of a psychological intervention. The literature search also retrieved some studies in early psychosis using mobile-based technology that can assist other forms of mental health support, such as symptom monitoring or medication adherence, not necessarily in the context of a theory-driven protocol-based psychological intervention (39-41). However, the study of the effects and mechanisms of change of mobile-based technology in the form of continuous monitoring of symptoms outside a treatment model deserve further attention in the research community (42). A step forward on smartphone apps for psychosis is the one proposed by Cella and colleagues, where they combine a self-assessment mobile phone app and a wrist worn device which continuously record heart rate variability (HRV) and electrodermal activity (EDA) in people with FEP, with the purpose of identifying relapse bio-signatures that can inform refined early interventions for psychosis (43). Finally, it is essential to highlight that all the studies testing smartphone-based interventions reviewed include acceptability and safety measures, with positive findings on those reporting study results. This is particularly interesting, as further research on users’ views have shown that data protection and safety is one of the major concerns of early psychosis service users (44), who also expressed that endorsement of the technology by a valid institution (e.g., university or health service) would serve them as a guarantee and would increase digital interventions uptake.
As stated before, the two identified psychological online intervention for early psychosis have been designed by the same clinical and research group at the E-Health division of Orygen, the National Centre of Excellence in Youth Mental Health in Australia. These pioneer interventions use social media platforms that put together psychoeducational therapy units with a forum-like feature that allows users to talk about their personal problems and find peer-support. HORYZONS and MOMENTUM are tailored to FEP and CHR therapy targets and have been proven feasible, acceptable and engaging. Although they have only been tested in small feasibility studies, results are very encouraging and the MOST technology is also being implemented to support young people recovering from depression and carers of young people with mental health issues. Further developments of this technology could even incorporate advanced computational and artificial intelligence methods, such as chatbots (a computer programme that mimics conversation with users via a chat interface, either text or voice based) or individualised therapy suggestions based on linguistic analysis of newsfeed postings (35). The Australian group has recently published the protocol of the randomised controlled trial of HORYZONS (45), which includes 170 people with FEP, and the results of this study are expected by the end of 2019 or beginning of 2020. In terms of other online tools to support detection and intervention for early psychosis, the literature search retrieved two studies describing online platforms for the screening of early signs of psychosis and detection of CHR (46) and to monitor conversion to full-blown psychosis (47).
Based on our literature search, there is a clear lack of studies exploring the potential of VR-based interventions for early psychosis. Nonetheless, the search retrieved four studies using VR to assess different psychological processes associated to paranoid ideation in people at CHR for psychosis conducted by the research team lead by Dr. Lucia Valmaggia at the Institute of Psychiatry, Psychology and Neuroscience VR Lab (48-51). This group has also developed a virtual school canteen environment that aims to assess early signs of psychosis in young adolescents, which is currently been tested in a school-based sample (Gayer-Anderson et al., in preparation). It is important to point out that relevant clinical trials using VR technology to treat psychosis are including or have included participants being referred from EIS (52,53). These studies are using VR environments as a mean to expose people with psychosis to feared situations with the objective to drop defence behaviours and relearning safety, and test harm expectations. Crucially VR environments also allow ‘embodied’ cognitive processes to be targeted ‘in action’, such as in AVATAR therapy (54,55), with the ultimate aim that improvements made in VR environments will generalise to real-life contexts. Different forms of VR involving other users and or social processes, such as collaborative virtual environments or self-embodiment paradigms, could also help to improve social functioning in early psychosis.
Finally, it is important to stress the limitations of the present literature review. Firstly, only one database has been used to do the search of studies relevant to the main topic of this review. Nonetheless, based on the purpose of providing a general summary or overview of the selected topic and considering the scope of the selected database, the procedure followed is valid to generate qualitative data to provide a state-of-the-art overview. Secondly, the present review does not include a formal assessment of the quality of the studies reviewed. Ultimately, the definition of “early psychosis” has been formulated based to the clinical staged model proposed by McGorry and colleagues (6) instead of on traditional categories of psychosis. This model can be defined as a refined form of diagnosis with the advantages of taking into account the extent of progression of the condition at a particular point in time, where a person lies along the continuum of the course of illness (56), and guiding treatment selection (57).
Future research: Are we there yet?!
Young people often fail to engage adequately with services preventing them from obtaining long-term benefits from treatment (58). Main reasons for this issue are (I) young people do not reach out for help due to stigma associated to mental health, (II) lack of knowledge of specialist services and (III) because clinicians who do not acknowledge their experiences are unable to adequately address their needs (59). Digital health technologies have the potential to improve these barriers by offering young people innovative and flexible platforms to share their experiences and feel supported, bringing new ways to work with clinicians and researchers, allowing for a more precise assessment and enhancing positive change of the person’s daily performance. From the descriptive results of this literature review, we can say that the development and application of digital health interventions in early psychosis are still in their infancy. Results deriving from the reviewed studies showed that it is feasible to use digital technologies to deliver psychological interventions in early psychosis, with participants expressing high levels of acceptability and willingness to use them to support their progress and recovery. However, future research should explore the implementation of these technologies with larger samples and controlled designs.
The enthusiasm for technology of young people is undeniable, with data generated by independent survey companies highlighting that around 97% of youth are connecting to internet daily (60) or that around two-thirds of young adults (18-34) own smartphones, being also the group more likely to use social media (e.g., Facebook) (61). Most of the interventions described in the present review have included service users in the design and development of the interventions, either in the form of focus groups or live experiences advisory panels. Taking into account the rapid evolution of the technology and the growing expertise between young people on their usage, this seems to be a crucial step to ensure that the technology will include the right functionalities and delivery options, which will potentially enhance user engagement. The views of clinicians and other mental health professionals involved in the recovery process of the young people with psychosis must also be taken into account when designing these tools. These professionals should also have protected time to be trained on digital technologies, to ensure their implementation in routine care practices.
Considering the global effort on stablishing early intervention services, integrating the clinical staging framework and coordinating speciality care programmes for young people at early stages of psychosis (7), it is clear that both research and clinical communities must continue working together on the design and adaptation of digital technologies that can improve access to psychological support, service users’ engagement and enhancement of treatment outcomes.
Acknowledgments
The authors would like to thank all the researchers that provided updated information on the status of their research and shared unpublished material.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Yung AR, McGorry PD. The initial prodrome in psychosis: descriptive and qualitative aspects. Aust N Z J Psychiatry 1996;30:587-99. [Crossref] [PubMed]
- Joa I, Gisselgård J, Brønnick K, et al. Primary prevention of psychosis through interventions in the symptomatic prodromal phase, a pragmatic Norwegian Ultra High Risk study. BMC Psychiatry 2015;15:89. [Crossref] [PubMed]
- Häfner H. Special issue "Schizophrenia in Childhood and Adolescence". Eur Arch Psychiatry Clin Neurosci 1995;245:57-60. [Crossref] [PubMed]
- Schultze-Lutter F, Rahman J, Ruhrmann S, et al. Duration of unspecific prodromal and clinical high risk states, and early help-seeking in first-admission psychosis patients. Soc Psychiatry Psychiatr Epidemiol 2015;50:1831-41. [Crossref] [PubMed]
- National Institute for Health and Care Excellence. Bipolar disorder, psychosis and schizophrenia in children and young people. Available online: www.nice.org.uk
- McGorry PD, Hickie IB, Yung AR, et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry 2006;40:616-22. [Crossref] [PubMed]
- Fusar-Poli P, McGorry PD, Kane JM. Improving outcomes of first-episode psychosis: an overview. World Psychiatry 2017;16:251-65. [Crossref] [PubMed]
- Harrigan SM, McGorry PD, Krstev H. Does treatment delay in first-episode psychosis really matter? Psychol Med 2003;33:97-110. [Crossref] [PubMed]
- Gregg L, Tarrier N. Virtual reality in mental health: a review of the literature. Soc Psychiatry Psychiatr Epidemiol 2007;42:343-54. [Crossref] [PubMed]
- Slater M. A note on presence terminology. Presence Connect 2003;3:3.
- Schulteis MT, Rothbaum BO. Ethical issues for the use of virtual reality in the psychological sciences. In: Bush S, Drexler M, editor. Ethical issues in clinical neuropsychology. Lisse, NL: Swets & Zeitlinger, 2002:243-80.
- Rus-Calafell M, Garety P, Sason E, et al. Virtual reality in the assessment and treatment of psychosis: a systematic review of its utility, acceptability and effectiveness. Psychol Med 2018;48:362-91. [Crossref] [PubMed]
- Firth J, Cotter J, Torous J, et al. Mobile Phone Ownership and Endorsement of "mHealth" Among People With Psychosis: A Meta-analysis of Cross-sectional Studies. Schizophr Bull 2016;42:448-55. [Crossref] [PubMed]
- Myin-Germeys I, Oorschot M, Collip D, et al. Experience sampling research in psychopathology: opening the black box of daily life. Psychol Med 2009;39:1533-47. [Crossref] [PubMed]
- Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 2010;15:1-39. [Crossref] [PubMed]
- Ben-Zeev D, Brenner CJ, Begale M, et al. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull 2014;40:1244-53. [Crossref] [PubMed]
- Myin-Germeys I, Birchwood M, Kwapil T. From environment to therapy in psychosis: a real-world momentary assessment approach. Schizophr Bull 2011;37:244-7. [Crossref] [PubMed]
- Reininghaus U, Depp CA, Myin-Germeys I. Ecological Interventionist Causal Models in Psychosis: Targeting Psychological Mechanisms in Daily Life. Schizophr Bull 2016;42:264-9. [Crossref] [PubMed]
- Haker H, Lauber C, Rössler W. Internet forums: a self-help approach for individuals with schizophrenia? Acta Psychiatr Scand 2005;112:474-7. [Crossref] [PubMed]
- Schrank B, Sibitz I, Unger A, et al. How patients with schizophrenia use the internet: qualitative study. J Med Internet Res 2010;12:e70. [Crossref] [PubMed]
- Naslund JA, Aschbrenner KA, Marsch LA, et al. The future of mental health care: peer-to-peer support and social media. Epidemiol Psychiatr Sci 2016;25:113-22. [Crossref] [PubMed]
- Alvarez-Jimenez M, Alcazar-Corcoles MA, González-Blanch C, et al. Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 2014;156:96-106. [Crossref] [PubMed]
- Bhugra D, Tasman A, Pathare S, et al. The WPA-Lancet Psychiatry Commission on the Future of Psychiatry. Lancet Psychiatry 2017;4:775-818. [Crossref] [PubMed]
- Bucci S, Barrowclough C, Ainsworth J, et al. Actissist: Proof-of-Concept Trial of a Theory-Driven Digital Intervention for Psychosis. Schizophr Bull 2018;44:1070-80. [Crossref] [PubMed]
- Lim MH, Gleeson JF, Rodebaugh TL, et al. A pilot digital intervention targeting loneliness in young people with psychosis. Soc Psychiatry Psychiatr Epidemiol 2019. [Crossref] [PubMed]
- Kim SW, Lee GY, Yu HY, et al. Development and feasibility of smartphone application for cognitive-behavioural case management of individuals with early psychosis. Early Interv Psychiatry 2018;12:1087-93. [Crossref] [PubMed]
- Bucci S, Barrowclough C, Ainsworth J, et al. Using mobile technology to deliver a cognitive behaviour therapy-informed intervention in early psychosis (Actissist): study protocol for a randomised controlled trial. Trials 2015;16:404. [Crossref] [PubMed]
- Traber-Walker N, Gerstenberg M, Metzler S, et al. Evaluation of the Combined Treatment Approach "Robin" (Standardized Manual and Smartphone App) for Adolescents at Clinical High Risk for Psychosis. Front Psychiatry 2019;10:384. [Crossref] [PubMed]
- Barbeito S, Sánchez-Gutiérrez T, Mayoral M, et al. Mobile App-Based Intervention for Adolescents With First-Episode Psychosis: Study Protocol for a Pilot Randomized Controlled Trial. Front Psychiatry 2019;10:27. [Crossref] [PubMed]
- Steare T, O'Hanlon P, Eskinazi M, et al. App to support Recovery in Early Intervention Services (ARIES) study: protocol of a feasibility randomised controlled trial of a self-management Smartphone application for psychosis. BMJ Open 2019;9:e025823. [Crossref] [PubMed]
- Husain N, Gire N, Kelly J, et al. TechCare: mobile assessment and therapy for psychosis - an intervention for clients in the Early Intervention Service: A feasibility study protocol. SAGE Open Med 2016;4:2050312116669613. [Crossref] [PubMed]
- Kingdon D, Turkington D. Cognitive-behavioral therapy of schizophrenia. New York: Guilford Press, 1994.
- Alvarez-Jimenez M, Bendall S, Lederman R, et al. On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophr Res 2013;143:143-9. [Crossref] [PubMed]
- Alvarez-Jimenez M, Gleeson JF, Bendall S, et al. Enhancing social functioning in young people at Ultra High Risk (UHR) for psychosis: A pilot study of a novel strengths and mindfulness-based online social therapy. Schizophr Res 2018;202:369-77. [Crossref] [PubMed]
- D'Alfonso S, Santesteban-Echarri O, Rice S, et al. Artificial Intelligence-Assisted Online Social Therapy for Youth Mental Health. Front Psychol 2017;8:796. [Crossref] [PubMed]
- Seligman ME, Rashid T, Parks AC. Positive psychotherapy. Am Psychol 2006;61:774-88. [Crossref] [PubMed]
- Hall PL, Tarrier N. The cognitive-behavioural treatment of low self-esteem in psychotic patients: a pilot study. Behav Res Ther 2003;41:317-32. [Crossref] [PubMed]
- Hayes SC, Hofman SG. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry 2017;16:245-6. [Crossref] [PubMed]
- Eisner E, Bucci S, Berry N, et al. Feasibility of using a smartphone app to assess early signs, basic symptoms and psychotic symptoms over six months: A preliminary report. Schizophr Res 2019;208:105-13. [Crossref] [PubMed]
- Kumar D, Tully LM, Iosif AM, et al. A Mobile Health Platform for Clinical Monitoring in Early Psychosis: Implementation in Community-Based Outpatient Early Psychosis Care. JMIR Ment Health 2018;5:e15. [Crossref] [PubMed]
- Niendam TA, Tully LM, Iosif AM, et al. Enhancing early psychosis treatment using smartphone technology: A longitudinal feasibility and validity study. J Psychiatr Res 2018;96:239-46. [Crossref] [PubMed]
- Bucci S, Schwannauer M, Berry N. The digital revolution and its impact on mental health care. Psychol Psychother 2019;92:277-97. [Crossref] [PubMed]
- Cella M, He Z, Killikelly C, et al. Blending active and passive digital technology methods to improve symptom monitoring in early psychosis. Early Interv Psychiatry 2019. [Crossref] [PubMed]
- Bucci S, Morris R, Berry K, et al. Early Psychosis Service User Views on Digital Technology: Qualitative Analysis. JMIR Ment Health 2018;5:e10091. [Crossref] [PubMed]
- Alvarez-Jimenez M, Bendall S, Koval P, et al. HORYZONS trial: protocol for a randomised controlled trial of a moderated online social therapy to maintain treatment effects from first-episode psychosis services. BMJ Open 2019;9:e024104. [Crossref] [PubMed]
- McDonald M, Christoforidou E, Van Rijsbergen N, et al. Using Online Screening in the General Population to Detect Participants at Clinical High-Risk for Psychosis. Schizophr Bull 2019;45:600-9. [Crossref] [PubMed]
- Brodey BB, Girgis RR, Favorov OV, et al. The Early Psychosis Screener for Internet (EPSI)-SR: Predicting 12 month psychotic conversion using machine learning. Schizophr Res 2019;208:390-6. [Crossref] [PubMed]
- Valmaggia LR, Day FL, Kroll J, et al. Bullying victimisation and paranoid ideation in people at ultra high risk for psychosis. Schizophr Res 2015;168:68-73. [Crossref] [PubMed]
- Valmaggia LR, Day F, Garety P, et al. Social defeat predicts paranoid appraisals in people at high risk for psychosis. Schizophr Res 2015;168:16-22. [Crossref] [PubMed]
- Shaikh M, Ellett L, Dutt A, et al. Perceived ethnic discrimination and persecutory paranoia in individuals at ultra-high risk for psychosis. Psychiatry Res 2016;241:309-14. [Crossref] [PubMed]
- McDonnell J, Stahl D, Day F, et al. Interpersonal sensitivity in those at clinical high risk for psychosis mediates the association between childhood bullying victimisation and paranoid ideation: A virtual reality study. Schizophr Res 2018;192:89-95. [Crossref] [PubMed]
- Freeman D, Lister R, Waite F, et al. Automated psychological therapy using virtual reality (VR) for patients with persecutory delusions: study protocol for a single-blind parallel-group randomised controlled trial (THRIVE). Trials 2019;20:87. [Crossref] [PubMed]
- Pot-Kolder RM, Geraets CN, Veling W, et al. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry 2018;5:217-26. [Crossref] [PubMed]
- Craig TK, Rus-Calafell M, Ward T, et al. AVATAR therapy for auditory verbal hallucinations in people with psychosis: a single-blind, randomised controlled trial. Lancet Psychiatry 2018;5:31-40. [Crossref] [PubMed]
- Rus-Calafell M, Garety P, Ward T, et al. Confronting Auditory Hallucinations Using Virtual Reality: The Avatar Therapy. Stud Health Technol Inform 2015;219:192-6. [PubMed]
- van Os J, Linscott RJ, Myin-Germeys I, et al. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med 2009;39:179-95. [Crossref] [PubMed]
- McGorry PD, Purcell R, Hickie IB, et al. Clinical staging: a heuristic model for psychiatry and youth mental health. Med J Aust 2007;187:S40-2. [Crossref] [PubMed]
- Burns J, Birrell E. Enhancing early engagement with mental health services by young people. Psychol Res Behav Manag 2014;7:303-12. [Crossref] [PubMed]
- Gronholm PC, Thornicroft G, Laurens KR, et al. Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: a systematic review. Psychol Med 2017;47:1867-79. [Crossref] [PubMed]
- Pew Research Center, Washington DC (2014). Available online: https://www.pewinternet.org/2014/02/27/the-web-at-25-in-the-u-s/12-internet-users-in-/
- Pew Research Center, Washington DC (2018). Available online: https://www.pewresearch.org/global/2019/02/05/in-emerging-economies-smartphone-adoption-has-grown-more-quickly-among-younger-generations/
Cite this article as: Rus-Calafell M, Schneider S. Are we there yet?!—a literature review of recent digital technology advances for the treatment of early psychosis. mHealth 2020;6:3.