Effectiveness of a mobile phone text messaging intervention on dietary behaviour in patients with type 2 diabetes: a post-hoc analysis of a randomised controlled trial
Sheikh Mohammed Shariful Islam, Elena S. George, Ralph Maddison
Contributions: (I) Conception and design: SMS Islam; (II) Administrative support: SMS Islam; (III) Provision of study materials or patients: SMS Islam; (IV) Collection and assembly of data: SMS Islam; (V) Data analysis and interpretation: SMS Islam, ES George; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors.
Background: Evidence suggests that mobile phone health (mHealth) programs may improve healthy behaviours and clinical outcomes in patients with type 2 diabetes mellitus (T2DM). However, data on mHealth dietary behaviour is scarce in low-and-middle-income countries. This study aims to determine the effectiveness of a text messaging program on dietary habits in patients with T2DM.
Methods: We performed a post-hoc analysis of a randomised controlled trial of text messaging intervention in 236 patients with T2DM recruited from a tertiary hospital. Data were collected on socio-demographics, mobile phone use, family and medical history, self-reported diseases, medication use, health-seeking behaviour, diet and physical activity. Dietary behaviour was assessed using a modified version of WHO STEPS and the Indian Migration Study Food Frequency Questionnaire. Intervention participants received one message/day over six months focusing on lifestyle modification. Dietary intake of fruits, vegetables, sugar beverages and teaspoons of sugar in tea/coffee were determined in serves-per-week and were analysed using Chi-square tests. Poisson regression models, adjusted for age, sex and baseline values following an intention-to-treat approach were performed and expressed as an estimate of effect size.
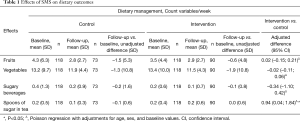
Results: At 6 months, the adjusted difference in vegetable consumption was −0.02 serves/week [95% confidence interval (CI): −0.11–0.06, P>0.05] and fruit intake was 0.02 serves/week (95% CI: −0.15–0.21, P>0.05). Consumption of sugar beverages reduced in both groups at 6 months with an adjusted difference of −0.34 serves/week (95% CI: −1.10–0.42, P>0.05). Teaspoons of sugar in tea reduced to 0.1±0.3 teaspoons/week in the control group, however, remained the same at 0.2±0.6 teaspoons/week in the intervention group with an adjusted difference of 0.94 teaspoons/week (95% CI: 0.04–1.84, P<0.05).
Conclusions: Our results suggest that a text messaging program did not significantly improve dietary behaviour in patients with T2DM. Further studies are warranted to explore the effectiveness of text messaging on dietary behaviour in adults with T2DM.
Trial Registration: German Clinical Trials Register DRKS00005188, http://www.drks.de.
Keywords: Type 2 diabetes mellitus (T2DM); diet; behaviour; mobile health; short message service
Received: 15 January 2020; Accepted: 08 July 2020; Published: 20 January 2021.
doi: 10.21037/mhealth-2020-3
Introduction
Type 2 diabetes mellitus (T2DM) is among the most prevalent non-communicable diseases worldwide, with low and middle-income countries being most affected most (1-3). The prevalence of T2DM in adults worldwide is expected to rise from 171 million in the year 2000 to 366 million in the year 2030 (4). Approximately 8.4 million of the world’s diabetes sufferers are in Bangladesh, placing Bangladesh in the top five countries for diabetes (5). Urban areas are the most affected, with a prevalence of 8.1%, compared to 2.3% in rural areas (6). Diabetes imposes a substantial economic burden on patients, their families and society as a whole (7,8). Along with financial hardship, T2DM poses a significant health risk to patients if left untreated who may develop complications such as neuropathy, nephropathy, retinopathy and an increase in the risk of mortality (9). Furthermore, people with T2DM also have higher rates of depression (10,11).
Current treatment for T2DM includes dietary and lifestyle modification, along with pharmacological interventions (12). Glycaemic control is the primary target for dietary changes, and it is widely accepted that excess or refined dietary carbohydrates are the main drivers for high blood glucose levels (13). Additionally, self-monitoring of diet, physical activity, and blood glucose can help to reduce the progression of T2DM and the potential for complications associated with uncontrolled diabetes (1). Interventions focusing on improving dietary and lifestyle behaviours have shown to improve health outcomes (14). However, adherence to a healthy diet and lifestyle in patients with T2DM is low (15).
Among the digital health movement in health-care, web-based, and mobile phone interventions have been used to improve the delivery of health services and chronic disease management worldwide (4,16). Mobile phones have become widely available and accessible in many low-and-middle-income countries providing opportunities to reach a large proportion of the population at a low-cost (17,18). Mobile phone programs have been shown to be useful for supporting diabetes management, including diet and lifestyle education leading to an improvement in dietary behaviours and greater blood glucose control in patients with T2DM (19-22). Current text messaging interventions aimed at improving dietary practice have been used in various studies, including in healthy college students with poor eating habits and overweight adults involved in a weight loss program (23). A few studies have reported an improvement in dietary behaviours following a text messaging intervention (23,24), although a systemic review of the evidence showed mixed results (25). However, studies focusing on dietary behaviour in T2DM are limited, with most papers in disease management focusing on blood glucose control, rather than dietary behaviour changes specifically. In a randomised controlled trial, we have previously reported that a mobile phone text messaging program improved glycaemic control in patients with T2DM in Bangladesh (26). As a secondary outcome, we collected data on the dietary habits of the participants. In this study, we aimed to determine the effectiveness of a text messaging program on dietary behaviour among patients with T2DM in Bangladesh. We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/mh-2019-dhcd-04).
Methods
We performed a post-hoc analysis from a randomised controlled trial of text messaging intervention in patients with T2DM in Dhaka, Bangladesh. The study protocol and primary outcomes have been published elsewhere (26,27). In brief, patients attending the outpatient department of Bangladesh Institute of Health Sciences (BIHS) Hospital between September 2013 and August 2014 who met the eligibility criteria were invited to participate.
The eligibility criteria included; a confirmed diagnosis of T2DM by a physician within 5 years according to the World Health Organisation (WHO) standards (28), on oral medication therapy, having access to a mobile phone and able to retrieve and read text messages. All registered participants at the BIHS hospital received a free education session on diabetes management at enrollment as well as a free eye examination and foot check. Eligible participants who provided written informed consent were enrolled for the trial and randomised 1:1 ratio to receive either a text messaging intervention plus standard care (intervention) or standard care only (control) for 6 months. Randomisation was carried out using a central computer-generated list for patient ID numbers.
Data were collected at baseline (0 months) and post-intervention (6 months) using face to face interviews and structured questionnaires. The questionnaires contained information on socio-demographics, mobile phone use and habits, family history, medical history, self-reported diseases, medication history, tobacco use, health-seeking behaviour, mental health, physical activity, diet and disability. Participant’s dietary habits were analysed using a modified WHO STEPS (29) and Indian Migration Study Food Frequency Questionnaire (30) to ascertain food consumption and dietary patterns along with type and frequency of consumption of different foods (Table S1). Weekly vegetable and fruit consumption were determined as serves/week. Weekly sugar consumption was measured in serves of sugar beverages consumed per week (1 serve =330 mL of coca-cola/fanta/sprite) and teaspoons of sugar in tea or coffee. Anthropometric measurements including height and weight, and blood pressure were taken by a trained research assistant at baseline and 6 months in duplicate, using a standard protocol (27) and the mean data were reported. Glycated haemoglobin (HbA1c) was measured at baseline and 6 months using standard laboratory assays by investigators blinded to participant allocation.
Participants in the intervention group received a text message once a day for 6 months. These messages included content regarding medication compliance, health education about diabetes, its complications, diet, and physical activity. A total of 90 theory-based text messages were delivered during the intervention period containing information on diabetes education (n=43), medication adherence (9), diet (20), and physical activity (18). Examples of the messages are available elsewhere (27). A combination of national and two international guidelines for diabetes management (31-33) were used to generate a preliminary list of messages. The text messages were reviewed by a team of health professionals consisting of general physicians, an endocrinologist, an epidemiologist, a nurse, and an undergraduate student at three consensus meetings. The selected messages were based on the principles of behavioural change theories. Text message content was made suitable for the general population, following pre-testing feedback of the messages from 50 participants with diabetes from another diabetes centre in Dhaka city. Text messaging was delivered in partnership with Grameenphone Bangladesh using a web-based program capable of sending automated text messages to participants.
Participants randomised to the control arm were provided standard care and attended their appointment as usual. All assessments were completed at baseline and 6 months via face-to-face appointments.
Data were analysed using SPSS statistical software and presented as mean ± standard deviation and other summary statistics as appropriate. Descriptive analysis was used to report food consumption, including dietary choices, type, and frequency of consumption of different foods. Dietary change of fruits, vegetables, sugar beverages and teaspoons of sugar in tea and coffee were determined in serves per week and were analysed using Chi-square tests. Prevalence odds ratios were calculated, adjusting for potential confounding variables (gender, age, smoking habits, body mass index, socioeconomic status, family history of diabetes). The interaction between age and risk factors, obesity and diabetes risk factors, and nutritional status and risk factors were examined using the logistic regression model. The effectiveness of the intervention was examined by comparing the change in HbA1c level between intervention and control groups at 6 months. Associations between variables was tested using bivariate regression models. Multivariate linear, logistic, and Poisson regression models, adjusted for age, sex, and baseline values following an intention to treat approach were performed. For all models, the results are expressed as an estimate of effect size, with 95% confidence intervals (CI) and P values.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The ethics review committee (ERC) of the International Center for Diarrhoeal Diseases Research, Bangladesh (ICDDR, B) approved this study (ERC number: PR#13068). All patients enrolled completed the informed consent form.
Results
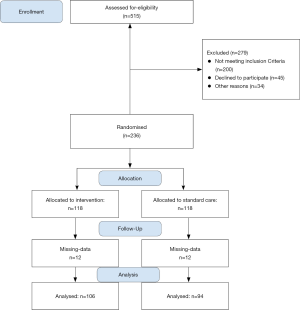
There were 236 patients with T2DM recruited for this study; of which 36 patients had missing data for HbA1c and were excluded from the analysis. A total of 200 participants (94 participants in the control group and 106 participants in the intervention group) were included in the post-hoc analysis (Figure 1). The mean ± SD age of participants was 48.1±9.7 years, and 54.2% were female, which is consistent with the general population living with T2DM in Bangladesh (34).
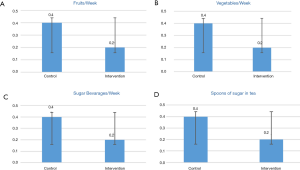
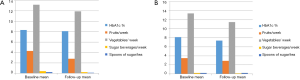
At baseline, no participants in either group met the recommended levels of fruit and vegetables as per the WHO guidelines (35). Participants reported an average vegetable consumption of 13.2±9.7 serves/week in the control group and 13.4±10.0 serves/week in the intervention group. Fruit consumption was higher in the control group (4.3±6.3 serves/week) compared to the intervention group (3.5±4.4 serves/week). The mean sugar beverages consumed was higher in the control group (0.4±1.3 serves/ week) than the intervention group (0.2±0.6 serves/week). However, the average use of sugar in tea or coffee per week was similar in both groups (0.2±0.5 vs. 0.2±0.4 tea-spoons), as shown in Figure 2.
As can be seen in Table 1, both groups showed a reduction in vegetable consumption at 6 months (−1.3±10.8 serves/week in control vs. −1.9±10.8 serves/week in intervention group). The adjusted difference between the intervention and control group in vegetable consumption was −0.02 serves/week (95% CI: −0.11–0.06, P>0.05). Fruit intake changed −1.5±5.3 serves/week in the control group and −0.6±4.8 serves/week in the intervention group with an adjusted difference of 0.02 serves/week (95% CI: −0.15–0.21, P>0.05). Figure 3 shows the dietary variables in the control and intervention groups at baseline and 6 months. Consumption of sugar-sweetened beverages reduced in both groups (−0.2±0.9 serves/week in control group and 0.1±0.7 serves/week in the intervention group) with an adjusted difference of −0.34 serves/week (95% CI: −1.10–0.42, P>0.05). Spoons of sugar in tea/coffee reduced to 0.1±0.3 teaspoons/week in the control group, but remained the same at 0.2±0.6 teaspoons/week in the intervention group, with an adjusted difference of 0.94 teaspoons/week (95% CI: 0.04–1.84, P<0.05).
Full table
Discussion
Our results suggest that a text messaging program in people with T2DM did not significantly improve dietary behaviour, which is similar to another recent trial reporting no significant group differences for diet (36). The changes in diet indicated low adherence to the WHO dietary recommendations for fruit and vegetables (37) in both groups with no change in sugar beverages and added sugar intake. This indicates that diet was unlikely to have contributed to glycaemic improvements in this study. It is possible that improvements in glycaemic control observed in the original trial were due to improved medication adherence, clinic attendance, physical activity or motivation.
Dietary behaviour is difficult to change and may require multiple approaches. In a text messaging study in individuals with diabetes, a diet module was provided that patients could electively opt in to, this study indicated that 82% of participants who received healthy eating messages reported a positive impact on their dietary behaviour (38). Therefore, diet-specific content may be required to elicit changes in dietary behaviour. In this study, reduced compliance to the WHO dietary recommendations (37) may have been due to insufficient messages focusing on diet or participants focusing on reducing overall food consumption in order to lower blood glucose levels. A previous study in Bangladesh reported that people with T2DM were willing to pay to receive the mobile phone text messaging program for diabetes (39). Mobile phone text messaging might be a low-cost tool to reach a large population in LMICs.
A possible reason for the decrease in fruit and vegetable intake observed in the present study at follow-up in both groups may be a result of participants trying to simply reduce overall food consumption as an effort to lower blood glucose levels. It is a common misconception that sugar in fruit should be avoided by individuals with T2DM (40), which may have contributed to the observed reduction in fruit servings per week; despite being below the recommended intake. Previous reviews of text messaging for improving dietary behaviour have shown mixed results, with no consistent patterns (41). The null findings found in this study may be further explained by the characteristics of the participants. In previous studies that have demonstrated a beneficial effect of text messaging on dietary behaviour, study participants have tended to be more healthy and proactive, otherwise healthy but overweight adults or generally healthy adolescents with unhealthy eating patterns (42,43). Thus, a group of obese participants enrolled in a weight loss program may be more motivated to improve dietary habits following text messaging prompts, compared to a patient with T2DM who simply wants to control their disease, which they can do using medication.
Our study had several limitations; Firstly, this study involved secondary data analysis from a trial where the primary outcome was measured by changes in glycaemic control. Thus all findings can be considered as hypothesis-generating. Secondly, data collection took place in a single centre and may not be representative of the entire population. Therefore, caution is required when interpreting the results. Third, we did not collect details about dietary intake, which would allow quantification of macronutrients, such as amounts of dietary carbohydrates. If these were examined in detail, additional information regarding diet quality such as refined carbohydrate intake over whole grains, and carbohydrate distribution might have provided a more detailed picture of the potential for what occurred concerning dietary changes. Fourth, we were unable to measure if our participants received any further diabetic management education from external sources. As all our participants were registered patients, it may be assumed that they all received the same diabetic management education from BIHS. However, of note, this is unlikely to affect our results as all participants were randomised at baseline, and any differences should be by chance. Finally, the generalisation of the text messages used in the intervention may have hindered the ability of participants to reach their full potential in regards to improving dietary habits. If text messages contained more specific information about what makes up a healthy diet and how to achieve this and these were personalised to align with the study participants socioeconomic status and ethnicity, a more significant change in dietary variables may have been seen. The strength of the study is the randomised controlled design with a reasonable sample size in a low-and-middle-income setting.
Future work should include additional dietary measures to allow assessment of quantity and quality of diet including total carbohydrate intake and the balance of refined versus wholegrain intake, total intake and the balance of saturated, mono and poly-unsaturated and trans-fats. Ideally, a professional with relevant qualifications in the field of nutrition and dietetics should be included in the initial study team to ensure the most effective dietary variables are included for clinically relevant results. Tailoring of the intervention based on participants age, location and socioeconomic status should be considered, with adjustments to the intervention made accordingly. Further studies primarily focussed on text messaging interventions for improving dietary behaviour in patients with T2DM need to be explored using evidence-based theories (44,45). In this study, we did not consider the effects of a medication change, which might have impacted the results as any changes in medication could have affected glycemic control, irrespective of diet changes. Future studies in people with T2DM should consider including medication adherence and changes when assessing the impact of a dietary intervention on glycaemic control. Besides, the use of text messaging intervention on its own may serve populations where smartphone access is limited, such as in rural areas of Bangladesh and lower socioeconomic areas. If the intervention proves to be of benefit, it may help move standard diabetes care forward in becoming standard practice to included text reminders to all diabetes patients who own a mobile phone.
Conclusions
A mobile phone text messaging intervention did not improve dietary behaviour in adults with T2DM in an urban area in Bangladesh. Further studies with targeted messages for dietary behaviour are recommended.
Acknowledgments
We would like to thank Dr. Andreas Lechner of University Hospital Munich for his assistance and guidance in this research. SMSI has received grants from National Heart Foundation of Australia. We acknowledge the support from International Center for Diarrhoeal Diseases Research, Bangladesh (ICDDR,B), the German Academic Exchange Service (DAAD), the Federal Ministry for Economic Cooperation and Development (BMZ), and the Higher Education Excellence in Development Cooperation (Exceed).
Funding: This study was supported by the Center for International Health, Ludwig-Maximilians-UniversitΔt; the German Federal Ministry of Education and Research (BMBF); and ICDDR,B (GR#01014).
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Sheikh Mohammed Shariful Islam and Ralph Maddison) for the series “Digital Health for Cardiovascular Disease” published in the mHealth. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/mh-2019-dhcd-04
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ mh-2019-dhcd-04). The series “Digital Health for Cardiovascular Disease” was commissioned by the editorial office without any funding or sponsorship. SMSI served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of the mHealth from May 2015 to Apr 2021. RM served as the unpaid Guest Editor of the series. SMSI reports grants from German Federal Ministry of Education and Research (BMBF), grants and non-financial support from International Center for Diarrhoeal Diseases Research, Bangladesh (ICDDR,B), grants from Center for International Health, Ludwig-Maximilians-UniversitΔt, during the conduct of the study; grants from NHMRC, grants from National Heart Foundation of Australia, grants from High Blood Pressure Research Council of Australia, grants and personal fees from World Heart Federation, personal fees from US NIH, personal fees from WHO, outside the submitted work. Ralph Maddison reports grants from NHMRC, grants from National Heart Foundation of Australia, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors were accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The ethics review committee (ERC) of the International Center for Diarrhoeal Diseases Research, Bangladesh (ICDDR, B) approved this study (ERC number: PR#13068). All patients enrolled completed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ramadas A, Quek KF, Chan CKY, et al. Web-based interventions for the management of type 2 diabetes mellitus: A systematic review of recent evidence. Int J Med Inform 2011;80:389-405. [Crossref] [PubMed]
- Islam SMS, Purnat TD, Phuong NTA, et al. Non-Communicable Diseases (NCDs) in developing countries: a symposium report. Global Health 2014;10:81. [Crossref] [PubMed]
- Biswas T, Islam A, Rawal L, et al. Increasing prevalence of diabetes in Bangladesh: a scoping review. Public Health 2016;138:4-11. [Crossref] [PubMed]
- Pal K, Dack C, Ross J, et al. Digital Health Interventions for Adults With Type 2 Diabetes: Qualitative Study of Patient Perspectives on Diabetes Self-Management Education and Support. J Med Internet Res 2018;20:e40. [Crossref] [PubMed]
- Federation ID. IDF Diabetes Atlas. 5th ed. 2012.
- Hussain A, Rahim MA, Azad Khan AK, et al. Type 2 diabetes in rural and urban population: diverse prevalence and associated risk factors in Bangladesh. Diabet Med 2005;22:931-6. [Crossref] [PubMed]
- Shariful Islam SM, Lechner A, Ferrari U, et al. Healthcare use and expenditure for diabetes in Bangladesh. BMJ Global Health 2017;2:e000033. [Crossref] [PubMed]
- Safita N, Islam SMS, Chow CK, et al. The impact of type 2 diabetes on health related quality of life in Bangladesh: results from a matched study comparing treated cases with non-diabetic controls. Health Qual Life Outcomes 2016;14:129. [Crossref] [PubMed]
- Pavkov ME, Bennett PH, Knowler WC, et al. Effect of youth-onset type 2 diabetes mellitus on incidence of end-stage renal disease and mortality in young and middle-aged Pima Indians. JAMA 2006;296:421-6. [Crossref] [PubMed]
- Islam SMS, Ferrari U, Seissler J, et al. Association between depression and diabetes amongst adults in Bangladesh: a hospital based case–control study. J Glob Health 2015;5:020406. [Crossref] [PubMed]
- Islam SMS, Rawal LB, Niessen LW. Prevalence of depression and its associated factors in patients with type 2 diabetes: a cross-sectional study in Dhaka, Bangladesh. Asian J Psychiatr 2015;17:36-41. [Crossref] [PubMed]
- Basevi V, Di Mario S, Morciano C, et al. Comment on: American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care 2011;34(Suppl. 1):S11-S61. Diabetes Care 2011;34:e53-author reply e54. [Crossref] [PubMed]
- Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013;97:505-16. [Crossref] [PubMed]
- Hu FB, Manson JE, Stampfer MJ, et al. Diet, Lifestyle, and the Risk of Type 2 Diabetes Mellitus in Women. N Engl J Med 2001;345:790-7. [Crossref] [PubMed]
- Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract 2011;65:314-22. [Crossref] [PubMed]
- Rose T, Barker M, Maria Jacob C, et al. A Systematic Review of Digital Interventions for Improving the Diet and Physical Activity Behaviors of Adolescents. J Adolesc Health 2017;61:669-77. [Crossref] [PubMed]
- Islam SMS, Peiffer R, Chow CK, et al. Cost-effectiveness of a mobile-phone text messaging intervention on type 2 diabetes–a randomized-controlled trial. Health Policy and Technology 2019.
- Islam SMS. Awareness and Self-Reported Health Hazards of Electromagnetic Waves from Mobile Phone Towers in Dhaka, Bangladesh: A Pilot Study. Advances Public Health 2014;2014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a meta-analysis. Diabet Med 2011;28:455-63. [Crossref] [PubMed]
- Quinn CC, Butler EC, Swasey KK, et al. Mobile Diabetes Intervention Study of Patient Engagement and Impact on Blood Glucose: Mixed Methods Analysis. JMIR Mhealth And Uhealth 2018;6:e31. [Crossref] [PubMed]
- Chow CK, Ariyarathna N, Islam SMS, et al. mHealth in Cardiovascular Health Care. Heart Lung Circ 2016;25:802-7. [Crossref] [PubMed]
- Shariful Islam SM, Chow C, Redfern J, et al. Effect of text messaging on depression in patients with coronary heart disease: A sub study analysis from the TEXT ME randomised controlled trial. BMJ Open 2019;9:e022637. [Crossref] [PubMed]
- O'Brien LM, Palfai TP. Efficacy of a brief web-based intervention with and without SMS to enhance healthy eating behaviors among university students. Eating Behaviors 2016;23:104-9. [Crossref] [PubMed]
- Kaptein M, Ruyter BD, Markopoulos P, et al. Adaptive Persuasive Systems: A Study of Tailored Persuasive Text Messages to Reduce Snacking. ACM Trans Interact Intell Syst 2012;2:1-25. [Crossref]
- Cole-Lewis H, Kershaw T. Text messaging as a tool for behavior change in disease prevention and management. Epidemiol Rev 2010;32:56-69. [Crossref] [PubMed]
- Shariful Islam SM, Niessen LW, Ferrari U, et al. Effects of Mobile Phone SMS to Improve Glycemic Control Among Patients With Type 2 Diabetes in Bangladesh: A Prospective, Parallel-Group,Randomized Controlled Trial. Diabetes Care 2015;38:e112-3. [Crossref] [PubMed]
- Islam SMS, Lechner A, Ferrari U, et al. Mobile phone intervention for increasing adherence to treatment for type 2 diabetes in an urban area of Bangladesh: protocol for a randomized controlled trial. BMC Health Serv Res 2014;14:586. [Crossref] [PubMed]
- Organization WH. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WHO/IDF consultation. 2006.
- Organization WH. WHO STEPS surveillance manual: the WHO STEPwise approach to chronic disease risk factor surveillance: Geneva: World Health Organization 2005.
- Bowen L, Bharathi AV, Kinra S, et al. Development and evaluation of a semi-quantitative food frequency questionnaire for use in urban and rural India. Asia Pac J Clin Nutr 2012;21:355-60. [PubMed]
- Dyson PA, Kelly T, Deakin T, et al. Diabetes UK evidence‐based nutrition guidelines for the prevention and management of diabetes. Diabetic Med 2011;28:1282-8. [Crossref] [PubMed]
- Association AD. Standards of medical care in diabetes—2012. Diabetes Care 2012;35:S11-63. [Crossref] [PubMed]
- Conditions NCCfC. Type 2 diabetes: national clinical guideline for management in primary and secondary care (update). Royal College of Physicians (UK); 2008.
- (NIPORT) DNIoPRaT. Bangladesh Demographic and Health Survey 2011. 2011. Available online: http://www.measuredhs.com/publications/publication-FR265-DHS-Final-Reports.cfm. Accessed 23rd September 2018.
- Organization WH. Healthy Diet. World Health Organization, World Health Organization. 2018. Available online: http://www.who.int/news-room/fact-sheets/detail/healthy-diet. Accessed 23rd September 2018.
- Dobson R, Whittaker R, Jiang Y, et al. Effectiveness of text message based, diabetes self management support programme (SMS4BG): two arm, parallel randomised controlled trial. BMJ 2018;361:k1959. [Crossref] [PubMed]
- Organization WH. Global strategy on diet, physical activity and health: a framework to monitor and evaluate implementation. 2006.
- Dobson R, Carter K, Cutfield R, et al. Diabetes Text-Message Self-Management Support Program (SMS4BG): A Pilot Study. JMIR mHealth uHealth 2015;3:e32. [Crossref] [PubMed]
- Shariful Islam SM, Lechner A, Ferrari U, et al. Mobile phone use and willingness to pay for SMS for diabetes in Bangladesh. J Public Health (Oxf) 2016;38:163-9. [Crossref] [PubMed]
- Islam SMS, Biswas T, Bhuiyan FA, et al. Patients’ perspective of disease and medication adherence for type 2 diabetes in an urban area in Bangladesh: a qualitative study. BMC Res Notes 2017;10:131-8. [Crossref] [PubMed]
- Müller AM, Alley S, Schoeppe S, et al. The effectiveness of e-& mHealth interventions to promote physical activity and healthy diets in developing countries: A systematic review. Int J Behav Nutr Phys Act 2016;13:109. [Crossref] [PubMed]
- Kerr DA, Harray AJ, Pollard CM, et al. The connecting health and technology study: a 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int J Behav Nutr Phys Act 2016;13:52. [Crossref] [PubMed]
- Siopis G, Chey T, Allman-Farinelli M. A systematic review and meta-analysis of interventions for weight management using text messaging. Journal of Human Nutrition and Dietetics 2015;28:1-15. [Crossref] [PubMed]
- Cho Y-M, Lee S, Islam SMS, et al. Theories applied to m-health interventions for behavior change in low-and middle-income countries: a systematic review. Telemedicine and e-Health 2018;24:727-41. [Crossref] [PubMed]
- Ricci-Cabello I, Bobrow K, Islam S, et al. Examining development processes for text messaging interventions to prevent cardiovascular disease. JMIR Mhealth Uhealth 2019;7:e12191. [Crossref] [PubMed]
Cite this article as: Islam SMS, George ES, Maddison R. Effectiveness of a mobile phone text messaging intervention on dietary behaviour in patients with type 2 diabetes: a post-hoc analysis of a randomised controlled trial. mHealth 2021;7:10.