Leveraging standards-based, interoperable meHealth for universal health coverage
WHO defines eHealth as “the use of information and communication technologies for health” (1), and considers mHealth—the use of mobile phones as an information and communication technology (ICT) for health—to be a subset. The importance of mHealth should not be underestimated, noting that with more than 3.6 billion active subscribers worldwide (2), the mobile phone is by far the most prevalent “computing device” in both developed and developing country settings. We postulate that mHealth + eHealth = meHealth. This term denotes the full gamut of health-related ICT, including care delivery systems, insurance systems, health system management, and reporting and surveillance systems. The useful connotation that meHealth is about “me” reminds us that, to be effective, the overall national health system should maintain a person-centric view.
Connected systems are crucial for achieving universal health coverage (UHC)
Having the health system know about “me” is not easy. It means the various puzzle pieces of information about me have to be able to be fit together to construct “my” health picture. Globally, many countries are contending with how to make multiple information systems across the healthcare domain “speak the same language”. This ability of applications and systems to connect and share health information—to interoperate—supports important capabilities, including continuity of care, health system management and surveillance, and the financial transaction processing needed to support UHC.
The imperative for interoperability of health information systems is well stated by the UN Commission on Information and Accountability:
“The use of e-health and m-health should be strategic, integrated and support national health goals. In order to capitalize on the potential of ICTs, it will be critical to agree on standards and to ensure interoperability of systems. Health information systems must comply with these standards at all levels, including systems used to capture patient data at the point of care. Common terminologies and minimum data sets should be agreed on so that information can be collected consistently, easily shared and not misrepresented. In addition, national policies on health-data sharing should ensure that data protection, privacy, and consent are managed consistently” (3).
In many countries ICT systems are not yet in place at all healthcare facilities. In such a context, connectivity among systems is not the initial concern for policymakers. However, as the use of ICT inevitably increases, it often grows via uncoordinated investments by facilities, payers, ministries, and donors. These uncoordinated investments create unconnected information system silos. In this all-too-common situation, system-to-system inter-operability increasingly becomes a top-of-mind concern for the providers, patients, payers, and policymakers who need data to monitor and manage health services.
No interoperability without standards
How do disparate, siloed health information systems connect and share data with each other? This is a crucial point that must be appreciated: there is no inter-operability without standards. Some could argue that a point-to-point integration between two systems can be implemented without either party adopting standards—and this is true. Interoperability, however, can be thought of as many-to-many integration where the integrating parties do not know ahead of time with whom they will be connecting. To do this, there must first be agreement regarding how the connectivity will be achieved. This pre-agreement is accomplished via the adoption of standards.
By establishing a standards-based approach early in the process, a network effect can be created that unlocks value from the many individual, disparate meHealth investments. To support this network effect, it is important to develop a national framework of health-related norms and standards. The standards framework’s role is to define how new systems will connect with the others in the overall health ecosystem.
Even with a national standards framework in place, the development of national-scale infrastructure can, and should, be done over time. The pieces do not all need to be put in place at once. Rather, they can be brought together as national needs and systems evolve. Standards-based systems will be interoperable with each other, regardless of the underlying technology, as long as there is agreement regarding content, coding, and communication formats. This opens up opportunities. New, standards-based interfaces can be added onto existing (legacy) systems to connect them into the overall ecosystem.
The value proposition of a standards-based meHealth infrastructure
If interoperability is a challenge, what is the benefit from achieving it? To better understand the mechanics of this value proposition, it is important to understand how meHealth infrastructure supports the overall health system (Figure 1).
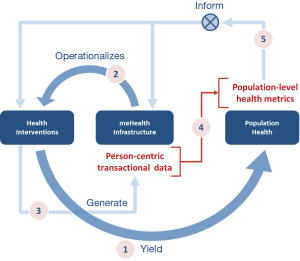
The meHealth infrastructure plays two key roles. First, it helps measure the health system’s performance. Person-centric transactions, if captured in a standards-based (hence computable) format, provide consistent, comparable data that can be collected and analyzed to determine how a nation is doing in delivering healthcare services and paying providers for services rendered. Secondly, the meHealth infrastructure provides a mechanism to exert process control, or feedback, upon the very system it measures. A health system that is metered and has feedback/feedforward process control loops can set itself on a path of continuous quality improvement. This can be incredibly effective over time.
Stakeholders: patients, providers, payers, and policymakers
Four key stakeholders provide information into and extract information from the meHealth infra-structure. Each has a different viewpoint on the healthcare value chain and on the infrastructure needed to support it.
- Policymakers—Policymakers establish the framework within which healthcare is provided to a country’s citizens. In this article, “policymaker” is a synonym for “ministry of health” or the jurisdictional entity responsible for the health of the population. Policymakers aggregate data from patients, providers, and payers to develop population-level metrics that inform their health and health economic policies.
- Patients—All of us (at one time or another) are patients. Patients are typically citizens, and sometimes voters or taxpayers. Policymakers have a fiduciary duty to this population. Patients receive care services from providers and are the beneficiary customers of the payers. Patients also may want to access information about their care via an electronic device (e.g., personal computer, or mobile phone).
- Providers—Providers operationalize care delivery by providing health services to patients and maintaining health information about them. The providers coordinate patient care with other providers as needed. Many providers are independent businesses that must manage their own operations and finances.
- Payers—Payers operationalize the financial elements of the health care system. Payers enroll patients as beneficiaries. They procure care services from the providers on behalf of their patient beneficiaries. They also must take on the actuarial task of ensuring the financial sustainability of the care program.
Making high-utility health infrastructure investments
The meHealth infrastructure “footprint” and maturity differ by country. In some countries, meHealth investments are highly fragmented, focused on primary-care delivery, and funded by multiple sources. In others, the investments are being driven by UHC initiatives addressing health financing. Although these investment strategies might logically be divided into chronological phases, in reality the investments are usually being made simultaneously with few linkages between them, despite needing similar data and infrastructure.
Regardless of the starting point, each country needs to:
- Articulate a health strategy;
- Articulate a meHealth strategy, aligned with the health strategy and sensitive to the existing ICT landscape in the country;
- Develop an implementation plan for a national infrastructure that operationalizes the strategy;
- Secure funding to implement the plan.
In what ways should these ideas inform a country’s health-related ICT investments? The key is to expect each investment to serve the broad, cross-cutting requirements of the overall health system. Reusable, standards-based meHealth infrastructure can and should be shared by the care delivery, insurance or payer, and “eGovernment” systems. Such shared infrastructure can then be leveraged by end-user applications that support transaction processing and management analytics on behalf of patients, providers, payers, and policymakers.
How do we get from “here” to “there”?
A recommended approach—called the “storytelling approach”—connects a country’s characteristic health stories to the data and data sharing patterns that are needed to tell these stories. It may be employed to express top-level health workflow requirements in terms that an IT professional can work from to select interoperability profiles (4).
The following implementation-focused recommendations are intended to inform policy-makers embarking on meHealth infrastructure projects. These recommendations, informed by country implementation experiences, fall into three broad categories:
(I) Storyboard: Develop a set of characteristic user stories that illustrate both the care workflows and the health insurance workflows common to the country. These stories should be aligned with the country’s health strategic goals [e.g., if improving maternal health outcomes is a strategic goal for the Ministry of Health (MOH), draft stories describing maternal care delivery activities].
Stack: Based on the requirements and the constraints in the country, choose a “stack of standards.” Countries can mitigate risk by selecting one of the three internationally balloted stacks of standards: HL7v3 (5), OpenEHR (6), and IHE (7).
Scope: Narrow the initial implementation scope and grow the scope over time. Any country embarking on a national-scale eHealth infrastructure effort will be well served by focusing on a few key areas. A “crawl, walk, run” strategy is usually best.
Concluding remarks
Wherever a country may be on its eHealth/mHealth journey and whatever its infrastructure implementation agenda, a broad view of the health system should be maintained to prevent siloed unconnected investments. As UHC initiatives are launched and payment processing systems are planned, ICT requirements related to care delivery should be taken into account, even if today those payments are covered by donors. Likewise, financial payment mechanisms should be considered a key requirement during the analysis and design phase of any new care delivery initiative.
A meHealth infrastructure must be a bridge between the policies that apply to care delivery and those that apply to health-system financing. This shared infrastructure will also support the data analytics that enable disease surveillance, public health reporting, UHC progress monitoring, and overall health system management.
For more information, refer to the complete article “Connecting Health Information Systems for Better Health: leveraging interoperability standards to link patient, provider, payer and policymaker data” (8) developed by the Joint Learning Network (JLN) for UHC.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- WHO Health topics. eHealth. Available online: http://www.who.int/topics/ehealth/en/
- Definitive data and analysis for the mobile industry. Available online: https://gsmaintelligence.com/
- Commission on information and accountability for Women’s and Children’s Health. Keeping Promises, Measuring Results. Available online: http://www.who.int/topics/millennium_development_goals/accountability_commission/Commission_Report_advance_copy.pdf
- Adebesin F, Kotzé P, Ritz D, et al. A Method for Selecting E-Health Standards to Support Interoperability of Healthcare Information Systems. Available online: http://hufee.meraka.org.za/Hufeesite/staff/the-hufee-group/paula-kotze-1/publications/a-method-for-selecting-e-health-standards-to-support-interoperability-of-healthcare-information-systems
- HL7 Version 3 Product Suite. Available online: https://www.hl7.org/implement/standards/product_brief.cfm?product_id=186
- Example openEHR Templates. Available online: https://openehr.atlassian.net/wiki/display/healthmod/Example%20openEHR%20Templates
- IHE. Available online: http://www.ihe.net/Profiles/
- JLN Information Technology Technical Initiative. Connecting Health Information Systems for Better Health. Available online: http://jointlearningnetwork.org/resource/connecting-health-information-systems-for-better-health
Cite this article as: Hesp C, Althauser C, Ritz D. Leveraging standards-based, interoperable meHealth for universal health coverage. mHealth 2015;1:5


