A content analysis of precede-proceed constructs in stress management mobile apps
Introduction
Half of Americans report their stress levels have increased in the past decade, yet they consistently under-utilize stress management techniques, reportedly due to lack of time (1). In the past several decades, 60% of clinicians have prescribed some form of self-help program or resource to accompany personal therapy (2), and many individuals are also seeking self-help programs independently (3,4). For example, one Australian study showed that approximately 70% of depressed respondents preferred self-prescribed self-management techniques as opposed to just 31% who sought professional help for their depression (5). However, in examining the efficacy of self-help programs, it is important to note that 95% of self-help books and 99% of internet sites are published without evidence demonstrating efficacy. While self-help programs may increase accessibility to stress-management, ineffective programs call into question the ethics of suggesting such programs that may lead to decreased self-efficacy among consumers and may actually complicate existing stress (6).
Fortunately, research has been conducted to test the efficacy of a limited number of self-help programs. Researchers from these studies report self-help treatments for mental health can be effective and may even be comparable to face-to-face treatments (7-9). For example, in a study of the effectiveness of self-help programs based on acceptance and commitment therapy, Fledderus et al. [2012] found that programs with minimal email contact with counselors were as effective as programs with extensive email contact, with both more effective than no treatment. The conclusion drawn from this study was that minimal email contact with a counselor was sufficient to make a self-help program as effective as on-site counseling (10). Another study echoed these findings by illustrating the effectiveness of an internet-delivered treatment with minimal feedback among people with depressive symptoms (11). Self-help treatments such as these may be particularly useful due to their cost-effectiveness (12) and ability to reach vulnerable populations, including adolescents (13), those living in rural or remote areas, and those for whom retaining anonymity is important (14). However, Newman [2011] has concluded that self-help therapy is generally effective, but only as effective as the program being utilized (12).
As technology access has evolved, primarily through decreased cost and increased network availability, it has increased accessibility to self-help stress management programs. While the pace of evaluation research has struggled to keep up with the development of new technology, numerous publications do demonstrate precedent for the use of technology in self-stress-management. In a study of soldiers with post-traumatic stress disorder (PTSD), one-third of participants who completed a self-managed program sustained high levels of recovery at 6 months from initiation. This study incorporated technology through the use of a website to educate participants on coping mechanisms. It also included user-driven assignments to measure knowledge and application. Additionally, participants had access to a therapist through phone calls or emails. Further development of internet based programs was recommended to decrease stigma and cost while increasing efficiency of treatment (15). Another randomized control trial showed that the use of personal data assistant (PDA) could speed rates of improvement by reducing therapist contact time. A follow-up study found clinician-guided therapy to be more effective than computer and telephone therapy (16).
More recently, researchers have tested the efficacy of mobile apps in improving stress (17,18). One review of such apps reported high inclusion of health behavior theory constructs and improved mental health outcomes, including decreased levels of depression and better stress and life satisfaction ratings (19). As mobile app technologies are becoming more accessible and physicians and other health care professionals have begun to use health apps in their practices (20,21), they may wish to recommend one of the now hundreds of stress management apps available to their clients. While recent reviews have analyzed the efficacy of mental health apps in changing behavior (22) and theoretical content in other health apps (23,24), no research to date has been conducted on the content of stress management apps available for download by mobile phone users. The purpose of this study was to provide a basic overview of health care and fitness apps related to stress management available through Apple’s iTunes App Store, which interface with the iPhone. Additionally, this study sought to appraise each app’s potential for influencing behavior change.
Methods
Design
This study involved a qualitative content analysis of descriptions of apps, which were provided by the apps’ developers and were accessed through the iTunes App Store. iPhone apps were chosen for this study because of their overwhelming popularity and versatility and use in previous content analyses (24). The Precede-Proceed Model (PPM) (25) was used to guide the coding of the apps. Two of the study authors designed the coding methodology and instrumentation following a preliminary review of apps. The study authors trained two research assistants to code the apps.
Sample
Apps included in this study sample came from the health and fitness category in iTune’s App Store and were identified as being related to stress management. The study sample was limited to English language apps within the healthcare and fitness category. Insomuch as free apps are frequently lite versions (a scaled down version with limited functionality) of paid apps (26), only paid apps were included in this study in order to access all available features for coding. Based upon these inclusion/exclusion criteria, the study sample included 259 apps.
Measurement
Each app was coded for basic descriptive information, such as the app’s name and price. Based upon the preliminary review of apps during study design, the authors concluded that some apps were either not intended to promote health or prevent disease, made claims that were not believable or plausible, or could not be recommended to a client for use in a professional setting. It should be noted that no standard exists for determining the face validity of apps. For this purpose, coders assessed each app to determine if, from the perspective of a health professional, the app was (I) intended to promote health or prevent disease; (II) believable or plausible; and (III) recommendable to a client for use to improve health or prevent disease.
Next, the PPM was used to code each app according to its level of influence for behavior change. PPM, which provides a continuous series of steps in the process leading to behavior change, is a widely accepted health education framework (25). PPM was used in this study to guide the coding of the apps on several important dimensions related to behavior change. On the basis of cumulative research on health and social behavior, hundreds of factors could be identified that have the potential to influence a given health behavior. PPM groups them according to the educational and organizational strategies likely to bring about behavior change. The three broad groupings are predisposing factors, enabling factors, and reinforcing factors. For this study, predisposing apps were those utilities likely to precede behavior and which were cognitive- or affective-based. Predisposing apps contained information related to attitudes, knowledge, awareness, beliefs, information, values, confidence, motivation, self-efficacy, etc. Apps were coded as enabling if they were intended to be utilized, or occurred, at or around the same time as the desired behavior and if they facilitated behavior through teaching a skill, providing a service, tracking behavior, or merely recording behavior. Reinforcing factors are the rewards received and the feedback the learner receives from others following adoption of the behavior, which may encourage or discourage continuation of the behavior. Apps were coded as reinforcing if they were interactive, interfaced with a social networking site (e.g., automatic upload to Facebook), provided encouragement from trainers/coaches, or included an evaluation based upon the user’s self-report.
Analysis
The final study sample was comprised of only apps that were coded as intending to promote health or prevent disease/injury, which resulted in 255 apps, or 98.5% of the total number of stress management apps available in the health and fitness category. Inter-rater reliability was computed between the two trained coders on a subsample of the final data set and the concordance exceeded 90%, which is a standard accepted in the literature (27).
Results
App price and credibility
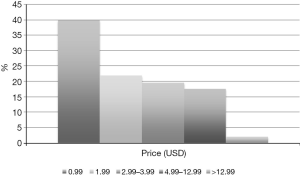
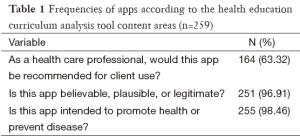
Most apps in this study sample had a price of $0.99 (Figure 1), with very few costing more than $12.99. Most apps in the study sample were coded to be believable, plausible or legitimate and all but 4 apps were determined to promote health or prevent disease. Coders concluded that only 63.3% would be of sufficient quality that they would recommend the app(s) for their own use or for client use (Table 1).
Full table
Theoretical classification of apps
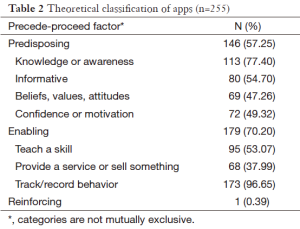
The majority of apps were coded as either predisposing or enabling (Table 2). Only 0.39% (or 1 app) was coded as reinforcing. Predisposing aspects of apps mostly involved the provision of knowledge or attempts to raise awareness (77.40%). Enabling apps were most commonly coded as tracking a behavior (96%) or teaching a skill (53%). The single reinforcing app integrated with a social networking site to provide social support. The app provided evaluations with feedback and coaching based on user input.
Full table
Conclusions
More than half of the apps in this study were established upon predisposing factors, which are primarily knowledge-based. If most stress management apps available are built primarily around predisposing factors, professionals should consider the added utility of these apps above and beyond traditional approaches (e.g., self-help guides and manuals and reference books). Upon first inspection, apps in the current study appear more affordable (i.e., just $0.99) than traditional approaches and are consistent with the price of apps studied in other disciplines (28). However, considering that all users access the app store via a device (e.g., iPhone, iPod, laptop) that contracts with a data service provider for a monthly fee, the actual price to the user may be higher. However, these higher costs may be offset by the convenience associated with being able to consolidate functions into a single device. For example, being able to read about risk factors for heart disease and make personal calls all in the same device may be very appealing to many users. Nevertheless, despite the convenience of modern mobile devices, the stress management apps included in this study do not extend beyond what may be accomplished through traditional approaches, which employ predisposing factors.
The most commonly coded theoretical classification of apps in the current study were those based upon enabling factors, such as teaching skills or tracking/recording actual behavior. Ravert, Calix and Sullivan [2010] (29) note that mobile devices may be used as a means to measure behavior in a convenient and immediate manner, which has historically been dependent on the users recalling and manually inputting data. Indeed, manual uploads to mobile devices regarding one’s behavior may be preferred to more traditional recording practices, namely pen and paper (30). Additionally, more automated processes introduce the possibility of harnessing the devices’ capabilities for monitoring, which alone may incentivize behavior change by allowing the user to report their behavior change progress (31).
Only one app in this study was found to include reinforcing factors, which are characterized by the provision of encouragement, evaluation, and the opportunity to interact with others. This finding is consistent with that of Abroms et al. [2011] who reported that few apps connect the user to outside sources, including social support systems (32). This appears to be a missed opportunity, given the capacity of emerging mobile device technology. Adapting from the PPM, the hallmark of reinforcing is the extent to which the apps connect the user with external systems or communities, such as social networking sites. As it relates to mobile devices, Heron and Smith [2010] have referred to this process as ecological momentary interventions (33), or as Intille, Kukla, Farzanfar and Bakr [2003] call it, ‘just-in-time’ (34). Such interventions refer to apps that adapt as a result of data obtained from the user. These uses might be thought of as real-time behavior change support, where users can receive reinforcement via a pre-programmed virtual coach or actual human interaction.
Fjeldsoe et al. [2009] have recognized the need for interventions utilizing mobile devices to be based upon theoretical principles (35). Public health professionals could partner with app developers to create apps that align with established behavior change theories (36), including those that would emphasize the reinforcing paradigm prominent in the PPM. Based upon the current study, existing stress management apps are limited in their inclusion of reinforcing factors, which are considered vital in facilitating behavior change. Theory is critical in public health interventions and research because it aids in understanding how and why individuals, groups, and organizations behave and change (37). Public health should take a more active role in the creation of health and fitness apps. Indeed, previous research has shown that mobile device interventions are most effective when they are based upon theory (38,39). These interventions will become increasingly more available as the technology’s penetration deepens (40) and could be a powerful tool for public health professionals in broadening their influence and in reaching previously isolated segments of the community (41).
Limitations
There are several limitations that should be considered when interpreting the results. First, the sample was collected in 2011 and may not represent the current sample of stress apps. However, as apps can be created by any third party and the number and types of apps available change daily, samples are arbitrary. This study provided a snapshot of apps available in the apps store. Second, the coders used the developers’ own descriptions of their apps in order to code them. It is possible that some developers either overstated or understated the capabilities of their apps, which would have resulted in a misclassification for the purposes of this study. Third, the apps represented in this study may not include all of the apps potentially relevant to stress management. Just as the coders for this study identified numerous apps that were not intended to address stress management, it is likely that many relevant apps were equally misclassified into other iTunes categories, which would have precluded their inclusion in this study. In addition, this study focused only on apps associated with iTunes and excluded apps associated with other platforms (e.g., Android apps). Lastly, the PPM guided the coding of the apps and appeared adequate to the researchers, but it is unclear to what extent these coding categories covered all of the types of the apps listed under this section in iTunes.
Implications
There are many apps available to those desiring to promote health or prevent disease through stress management. Nevertheless, health education practitioners wishing to recommend the use of third-party apps for such devices as Apple’s iPhone should do so with discretion. It is recommended that practitioners be prudent when promoting the use of apps so as not to overstate their potential effectiveness, as it appears that most of the apps provide health-related information or make attempts at enabling behavior, with almost none including all factors of the PPM recommended for behavior change. Future research should extend recent work by Abroms et al. [2011] and actually test the efficacy of stress management apps in a rigorous randomized controlled study (32).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Stress in America: findings. Available online: https://www.apa.org/news/press/releases/stress/2010/national-report.pdf
- Quackenbush RL. The prescription of self-help books by psychologists: A bibliography of selected bibliotherapy resources. Psychotherapy 1991;28:617-7.
- Andrews G, Cuijpers P, Craske MG, et al. Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: a meta-analysis. PLoS One 2010;5:e13196. [PubMed]
- Rasmussen E, Ewoldsen DR. Dr. Phil and psychology today as self-help treatments of mental illness: a content analysis of popular psychology programming. J Health Commun 2013;18:610-23. [PubMed]
- Adams J, Sibbritt D, Lui CW. Health service use among persons with self-reported depression: a longitudinal analysis of 7,164 women. Arch Psychiatr Nurs 2012;26:181-91. [PubMed]
- Bernecker SL. Helping clients help themselves: Managing ethical concerns when offering guided self-help interventions in psychotherapy practice. Professional Psychology: Research and Practice 2014;45:111-19.
- Cuijpers P, Donker T, van Straten A, et al. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med 2010;40:1943-57. [PubMed]
- Berger T, Hämmerli K, Gubser N, et al. Internet-based treatment of depression: a randomized controlled trial comparing guided with unguided self-help. Cogn Behav Ther 2011;40:251-66. [PubMed]
- Vernmark K, Lenndin J, Bjärehed J, et al. Internet administered guided self-help versus individualized e-mail therapy: a randomized trial of two versions of CBT for major depression. Behav Res Ther 2010;48:368-76. [PubMed]
- Fledderus M, Bohlmeijer ET, Pieterse ME, et al. Acceptance and commitment therapy as guided self-help for psychological distress and positive mental health: a randomized controlled trial. Psychol Med 2012;42:485-95. [PubMed]
- Lappalainen P, Langrial S, Oinas-Kukkonen H, et al. Web-based acceptance and commitment therapy for depressive symptoms with minimal support: a randomized controlled trial. Behav Modif 2015;39:805-34. [PubMed]
- Newman MG, Szkodny LE, Llera SJ, et al. A review of technology-assisted self-help and minimal contact therapies for anxiety and depression: is human contact necessary for therapeutic efficacy? Clin Psychol Rev 2011;31:89-103. [PubMed]
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry 2010;10:113. [PubMed]
- Bennett K, Reynolds J, Christensen H, et al. e-hub: an online self-help mental health service in the community. Med J Aust 2010;192:S48-52. [PubMed]
- Litz BT, Engel CC, Bryant RA, et al. A randomized, controlled proof-of-concept trial of an Internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. Am J Psychiatry 2007;164:1676-83. [PubMed]
- Taylor CB, Luce KH. Computer- and internet-based psychotherapy interventions. Curr Dir Psychol Sci 2003;12:18-22.
- Mattila E, Lappalainen R, Pärkkä J, et al. Use of a mobile phone diary for observing weight management and related behaviours. J Telemed Telecare 2010;16:260-4. [PubMed]
- Ahtinen A, Mattila E, Välkkynen P, et al. Mobile mental wellness training for stress management: feasibility and design implications based on a one-month field study. JMIR Mhealth Uhealth 2013;1:e11. [PubMed]
- Payne HE, Lister C, West JH, et al. Behavioral functionality of mobile apps in health interventions: a systematic review of the literature. JMIR Mhealth Uhealth 2015;3:e20. [PubMed]
- Franko OI. Smartphone apps for orthopaedic surgeons. Clin Orthop Relat Res 2011;469:2042-8. [PubMed]
- Oehler RL, Smith K, Toney JF. Infectious diseases resources for the iPhone. Clin Infect Dis 2010;50:1268-74. [PubMed]
- Donker T, Petrie K, Proudfoot J, et al. Smartphones for smarter delivery of mental health programs: a systematic review. J Med Internet Res 2013;15:e247. [PubMed]
- Cowan LT, Van Wagenen SA, Brown BA, et al. Apps of steel: are exercise apps providing consumers with realistic expectations?: a content analysis of exercise apps for presence of behavior change theory. Health Educ Behav 2013;40:133-9. [PubMed]
- West JH, Hall PC, Hanson CL, et al. There's an app for that: content analysis of paid health and fitness apps. J Med Internet Res 2012;14:e72. [PubMed]
- Green LW, Kreuter MW. Health promotion planning: an educational and environmental approach. Mountain View: Mayfield Publishing Company, 1991.
- Lister C, West JH, Cannon B, et al. Just a fad? Gamification in health and fitness apps. JMIR Serious Games 2014;2:e9. [PubMed]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159-74. [PubMed]
- Shuler C. iLearn; a content analysis of the iTunes App Store’s Education Section, New York: The Joan Ganz Cooney Center at Sesame Workshop, 2009.
- Ravert RD, Calix SI, Sullivan MJ. Research in brief: using mobile phones to collect daily experience data from college undergraduates. Journal of College Student Development 2010;51:343-52.
- Boushey CJ, Kerr DA, Wright J, et al. Use of technology in children's dietary assessment. Eur J Clin Nutr 2009;63 Suppl 1:S50-7. [PubMed]
- Higgins JP. Smartphone applications for patients' health and fitness. Am J Med 2016;129:11-9. [PubMed]
- Abroms LC, Padmanabhan N, Thaweethai L, et al. iPhone apps for smoking cessation: a content analysis. Am J Prev Med 2011;40:279-85. [PubMed]
- Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 2010;15:1-39. [PubMed]
- Intille SS, Kukla C, Farzanfar R, et al. Just-in-time technology to encourage incremental, dietary behavior change. AMIA Annu Symp Proc 2003.874. [PubMed]
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 2009;36:165-73. [PubMed]
- Chambers CD, Hughes S, Meltzer SB, et al. Alcohol consumption among low-income pregnant Latinas. Alcohol Clin Exp Res 2005;29:2022-8. [PubMed]
- Glanz K, Rimer BK. 1995. Theory at a glance: a guide to health promotion practice. 2nd edition. Bethesda, MD: National Cancer Institute, 2005.
- Fjeldsoe BS, Miller YD, Marshall AL. MobileMums: a randomized controlled trial of an SMS-based physical activity intervention. Ann Behav Med 2010;39:101-11. [PubMed]
- Riley WT, Rivera DE, Atienza AA, et al. Health behavior models in the age of mobile interventions: are our theories up to the task? Transl Behav Med 2011;1:53-71. [PubMed]
- Smith A. Mobile Access 2010. Available online: http://www.pewinternet.org/files/old-media//Files/Reports/2010/PIP_Mobile_Access_2010.pdf
- Crilly JF, Keefe RH, Volpe F. Use of electronic technologies to promote community and personal health for individuals unconnected to health care systems. Am J Public Health 2011;101:1163-7. [PubMed]
Cite this article as: Payne HE, Wilkinson J, West JH, Bernhardt JM. A content analysis of precede-proceed constructs in stress management mobile apps. mHealth 2016;2:5.