Connected health: a review of the literature
In 1998, a brave cardiologist named Dean Ornish published a book called Love and Survival with a straightforward hypothesis and went on to defend, with scientific evidence, the notion that “love and intimacy are among the most powerful factors in health and illness” (1). He boldly declared, “I am not aware of any other factor in medicine—not diet, not smoking, not exercise, not stress, not genetics, not drugs, not surgery—that has a greater impact on our quality of life, incidence of illness, and premature death from all causes.” In the nearly two decades since his seminal work was made available for the general public, patients and researchers alike have focused on the knowledge that the people we surround ourselves with, providing support and being supported, matters deeply to our health and well-being. This field of inquiry has firmly established the criticality of social relationships for sustaining and improving health (2) and associated the lack of social integration with specific conditions such as cardiovascular disease, depression, cancer, infection, and mortality (3). Newer analytical techniques such as social network analysis are helping a fresh generation of researchers explore patterns of social connectedness through innovative procedures and algorithms that further expand our understanding.
For the purpose of this review, social support is defined as the various types of support or help people receive from others. Social support is generally classified into major categories such as emotional or instrumental support (4). Connection is included as a variable of interest as it reflects an emerging science and methodological route to discovering the impact of social support. It is possible that “connected health” describes today what social support was yesterday; when typed into a search engine, Google returns 156 million results. While it tends to be used interchangeably in modern parlance, the Merriam-Webster dictionary defines connection as “The act of connecting two or more things or the state of being connected; a situation in which two or more things have the same cause, origin, goal.” American researcher Brѐne Brown’s (5) definition of connection allows us to more clearly see the joining of the two concepts. Connection, she writes is “the energy that exists between people when they feel seen, heard, and valued; when they can give and receive without judgment; and when they derive sustenance and strength from the relationship.” Future research will undoubtedly focus on refining definitions that are so critical to our understanding of human health and wellness.
Connected health, which has its own URL managed by HIMMS (himssconnectedhealth.org) and twitter handle, is advancing an agenda to transform care delivery and create opportunities for self-management through the use of technology. Federal Meaningful Use standards, for example promote the use of health information technology (HIT) such as patient portals and secure email with a healthcare provider to promote the goals of enhanced patient and family engagement and supporting care coordination (6). The connected health movement relies fundamentally on patient-facing devices and technology, promising to support patients in their proactive, self-management efforts. Medical devices, purchasable over-the-counter, predate the connected-health movement and include blood pressure monitors and blood glucose meters. They were among the first devices to be connected through Bluetooth™ technology, transferring data to the cloud where it could be shared. There is increasing awareness that the newly liberated data produced by these re-appropriated devices, not traditionally available to healthcare providers, may have clinical utility. As a result, a plethora of connected products are making their way to market, including electrocardiographs, step and activity counters, sleep monitors, and calorie counters (7). As more and more technology is infused into our healthcare system, various authors have argued the merits of technology to support and connect patients, providers, and family caregivers. For the most part, their usefulness and accuracy have not yet been adequately established. The healthcare system will inevitably see more technological enhancements as a new generation of “digital native” consumers and practitioners permeate the system and researchers ought to work alongside them.
The goal of this integrative literature review was to identify and analyze research focused on the social support, or connection experienced by people with diabetes as they journey along a path of self-management. The hypothesis was that being connected to someone who cares is good for your health. Specific aims included: (I) describing the social support or connection metrics in use; (II) describing the types of HIT employed by the research community, if any, to connect patients and providers; and to (III) assess the state of the science in this area.
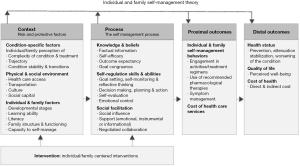
Conceptual framework
Diabetes is a chronic, non-infectious disease affecting over 29 million Americans, more than 9% of the population. It is the seventh leading cause of death and contributes greatly to morbidities such as hypertension, dyslipidemia, cardiovascular disease and death, heart attacks, strokes, kidney disease, blindness, and amputations. Diabetes management costs the United States an astounding $245 billion each year (8). One of the best ways to protect against the long-term devastating effects of diabetes is for a patient and family to engage in rigorous self-management. Ryan et al. (9-11) developed the Individual and Family Self-Management Theory (IFSMT) to outline the “process by which individuals and families use knowledge and beliefs, self-regulation skills and abilities, and social facilitation to achieve health-related outcomes” (10). Their model provides the conceptual framework for this review (Figure 1). Specifically, (I) the constructs social capital, social influence, and support were used to identify the problem and outline inclusion criteria for the review; (II) the range of evaluation outcomes (from engagement to health status and quality of life) encouraged the inclusion of a variety of studies that defined self-management as an outcome in broad terms; and (III) the emphasis on social elements in multiple places in the model deepened the understanding of social support versus connection that is discussed throughout this article.
Methods
Whittemore and Knafl (12) outline a process for conducting an integrative review of the literature, which facilitates the inclusion of multiple perspectives and diverse methodologies that in turn supports developing knowledge in emerging practice areas. The five steps used in this project were: problem identification, literature search, data evaluation, analysis, and presentation.
This review covered a 5-year period between 2009 and 2015. The databases searched were CINAHL (EBSCO Information Services, Ipswich, MA), PsychInfo (American Psychological Association, Washington, DC), and PubMed (National Library of Medicine, Washington, DC). Keywords used for searches focused on “diabetes” and “connect” or “social support” and “technology” (The term “health information technology” more commonly used to describe technology used in healthcare settings has not been formally mapped to each of three databases utilized in this review. Therefore, the more general term “technology” was used.). Recent studies published in peer reviewed, English-language journals that included adult research participants were included. Worldwide research was considered. Studies performed prior to September, 2009 were excluded because of the rapidly changing nature of the technology field.
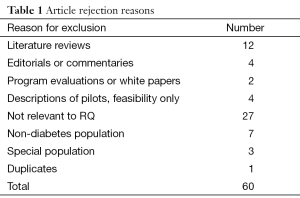
The literature search revealed 145 articles. Some articles were rejected immediately upon reviewing an abstract because they did not fit the search criteria. A large number of abstracts contained the term “social support” without ever having measured or defined social support as a variable within the study. Generous leeway was extended to include proxy measures for social support or connection but when the study clearly did not address either construct, the article was excluded. Ninety five remaining articles were read in their entirety to assess for inclusion. After the first reading, a total of 60 studies were rejected for a variety of reasons: when they described a special population with diabetes (e.g., neonates, people with serious mental illness or disabilities), did not use social support as a variable of interest, were reviews or duplicates (Table 1). In short, articles were included if they used social support or connection to assess a health outcome in the population of people with diagnosed diabetes, with or without using technology. This left a total of 35 articles included in the review. There were 15 (43%) descriptive or observational studies (13-27), 4 (11%) design or development studies (28-31), 3 (9%) quasi-experimental studies (2,32,33), 7 (20%) randomized controlled trials (34-40), and 6 (17%) qualitative studies (41-46) included in the review.
Full table
Articles were read multiple times. A master matrix was created with key research components so that cross-case comparisons about design, sample, setting, and results could be made. From the matrix and the articles, multiple data displays (47) were created to explore various methodological issues of interest such as sample, setting, operational definitions, technology type, and findings.
Results
Data matrices were used to examine all 35 articles, compare them, and analyze results. Frequencies and summaries were tabulated as appropriate. A content analysis approach (48) was used to synthesize findings and answer the research questions. In keeping with the research questions of this review as well as the integrative approach, this section includes the patterns of technology use by the patient community as well as findings pertinent to the state of the science.
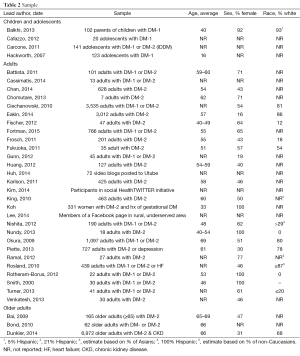
Sample
The 35 articles included samples that spanned ages from childhood and adolescents (n=4, 11%) through to older adults (n=3, 9%), the majority focusing on the adult population (n=28, 80%). Several small studies (focus groups, etc.) did not include information on the average age of participants and others provided information in a way that did not allow for extrapolation (e.g., a percentage of ages within a category). These studies represent patients of a variety of ages (Table 2). Females are well represented in this body of research. Studies tended to include largely all-white populations or be focused on specific non-white populations. Interestingly, studies performed outside of the US had a higher rate of non-reporting of race (n=9, 82%) than studies performed within the US (n=10, 42%). Two studies (6%) reported ethnicity instead of race (15,18).
Full table
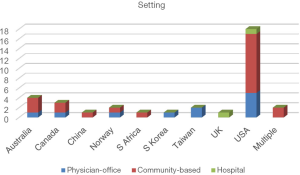
Setting
The included studies were performed in a variety of countries (Figure 2): 1 (3%) each from China (36), South Africa (32), South Korea (28), and the UK (43), 2 (6%) from Norway (25,31) and Taiwan (13,21), 3 (9%) from Canada (29,30,34), 4 (11%) from Australia (24,26,37,41), and 18 (51%) from the US (2,15-20,22,23,27,33,35,38-40,42,44,45). Two studies (6%) recruited participants from the World Wide Web and were therefore considered to be conducted in multiple countries (14,46). Only two studies (6%) recruited participants from hospital settings. Eleven studies (31%) recruited participants from the physician-office and 22 (63%) from the community.
Operational definitions
Social support was never formally defined in any of the 35 articles, although the concept was referenced liberally. Articles were included in this review when they assessed either social support or connection against a health outcome. As a result, some of the studies reported a social support measure and others assessed connection in different ways, 7 (20%) were judged to include both. Nonetheless, the instruments used to assess variables in these studies were diverse and are outlined in Table 3. To measure social support, 3 studies (9%) used author-defined scales, 4 (11%) used semi-structured interview questions, and 1 (3%) used field observation techniques. Connection measures (n=19, 54%) were focused on utilization rates (e.g., encounters with a coach, posts to an online community, texts to a peer supporter). Often the outcome measure of self-management or self-care was loosely defined.
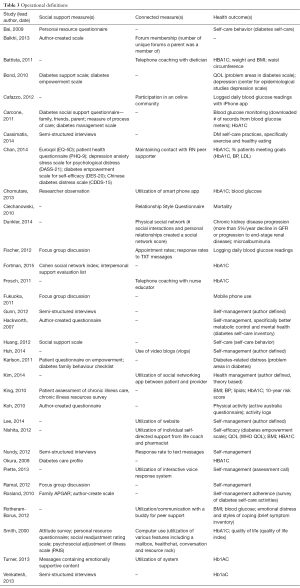
Full table
Technology use
The types of technology utilized in the studies varied greatly. Several studies used simple technologies such as the telephone, email messages, or text messaging. Others utilized website or mobile phone applications. IVR, a system whereby the patient interacts with a pre-recorded, automated, voice-mail message, was tested in one study (17). One study (46) evaluated video blogs (vlogs) posted to UTube, and three other studies evaluated the use of online forums (like Twitter) and other social network platforms (14,22,28). Fourteen studies (40%) did not use any technology (Table 4).
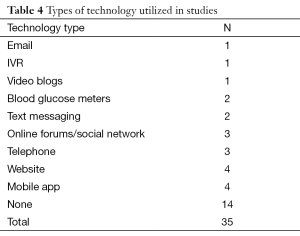
Full table
Selected findings
Selected findings related to the impact of social support and/or connection to health outcomes are presented in Table 5. Social support is significantly positively correlated with self-care behavior (15,21), taking diabetes medication (13), physical activity (13,26,44), and significantly negatively correlated with diabetes distress (25), as well as reductions in body mass index (39) and HbA1c (2,16,45).
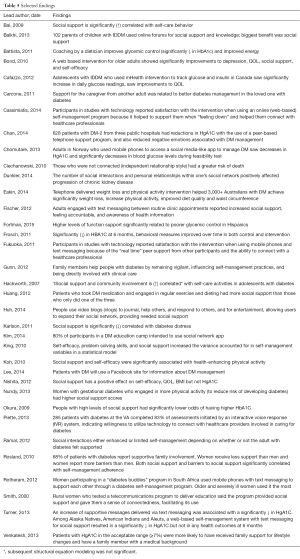
Full table
Connection is related to improved glycemic control (34), improved depression and quality of life (35), and reductions in HbA1C (31,36,38). In general connection is correlated with self-care activities in adolescents (30), improves weight loss through a telephone intervention (37), and is experienced when a family member remains vigilant (43). The number of social connections was negatively correlated with chronic kidney disease progression (14). Ciechanowski and colleagues (27) found that those who were least connected has a greater risk of death.
Three studies (n=3, 9%) furthered our appreciation of the complexity of connection, especially when family was used to provide social support. Connections or social interactions were found to either improve or limit self-management in patients with diabetes depending on whether or not the adult felt supported (18). Rosland and colleagues (19) noted that women receive less family support than men do and also report more barriers to self-management than men. When caregivers of patients with diabetes are supported, the patient experiences better self-management (20).
Several studies (n=3, 9%) confirmed that patients, even elderly and sick patients, will use technology to connect with healthcare providers and others with the same condition (17,28,29). Social support was cited as the greatest benefit of an online forum (22,41), of text messages delivered between clinic encounters (33) and among peers (40,42,49) and with vlogs (46).
Discussion
The goal of this integrative literature review was evaluate research that attempted to change a health outcome by the provision of social support or connection, and to assess the ways in which they were successful. Sixty percent (n=21) of the studies included in this review used some form of technology to facilitate or enhance human connection. Findings that support the hypothesis, being connected to someone who cares is good for your health, will be discussed below in six subheadings, in keeping with the presentation style common to content analysis (47,50). These content areas address the first and second specific aims of this review. In the seventh and final subheading, the state of the science is addressed.
Being connected matters
The findings from this study suggest that being connected matters. In qualitative studies, when asked what factors are motivating for self-management activities, participants describe the social support they receive from their friends (51). People from all sociodemographic categories will go to great lengths utilizing unfamiliar technology because it helps them to connect with their healthcare providers and with others who manage the same condition as themselves. Connection is so important, in fact, that people who do not have robust social networks suffer adverse outcomes such as worsening disease states (14) and even premature death (41). Hence, “the social in medicine” as defined by Ljungdalh & Moller (52) has become a legitimate field of study. They explain that with “the WHO development of the bio-psycho-social model of health, the social was identified as a cause of people’s health condition .. An awareness of social factors influencing people’s mental and physical health grew from the statistical research pointing out that strong association between social position and health status. From this it followed that the endeavor of health promotion must be to … design intervention programs that would take these social factors into account.” It is no surprise then, that both the scholarly and popular literature (53,54) which measure the impact of being connected and supported to one’s health, are growing in popularity. The findings of this review support the notion that being connected to someone who cares, whether a layperson or a healthcare professional, matters. Future work in the field, then, ought to plan for social support and/or connection as a variable of interest when evaluating self-management strategies.
Connection to family matters the most
People experience support in numerous ways. Typically social support behavior is categorized in terms of being emotional (e.g., expressions of love or caring), instrumental (e.g., taking a casserole to a sick neighbor), informational (e.g., receiving advice or suggestions on parenting), or appraisal (e.g., someone asks you to recall the times you have been successful at meeting challenges in the past to summon the courage to move forward). While patients value support in all forms from their doctors and healthcare providers, it is social support from family that appears to matter the most. Particularly in people with diabetes, support from a loved one is related to better disease management. Family members undoubtedly help in numerous ways, but due to the complexity of diabetes self-management, supportive family members can directly influence practices such as taking medications, preparing healthy foods, or recording insulin levels. Families help by being directly involved in care (instrumental support) and by remaining vigilant (emotional and informational support) (43). In fact, people who have good glycemic control (e.g., HbA1C scores >7%) are more likely to have received family support for lifestyle changes and have a family member with some type of medical background (45) than those with poor glycemic control. These findings suggest that research focused on ways to support family members with chronic disease may be a sound strategy for improving the health of the chronically ill.
Connection is complex
Nonetheless, connection is complex and we ought to be cautious in assuming that all support is good support. Emerging research suggests that the support provided by a family member is judged to be supportive or not supportive by the patient, and that summative verdict changes outcomes (18). This finding might help to explain the plethora of standardized instruments used to measure social support; each one trying to define support in just the right way from the patient and family perspective. Furthermore, there are striking implications from Fortman’s work (23) which suggest that supporting the caregiver of the patient with diabetes has an impact on glycemic control, and not always a positive one (to ascertain why, it might be helpful to think of grandma who lovingly “supports” her family with a constant stream of cakes and cookies). This is reminiscent of the “three degrees of influence” that Christakis and Fowler (54-57) write about, whereby we commonly influence not only the people directly within our social network, but their friends, and their friend’s friends, as well. This is a virtually untapped area of scholarly research in the realm of chronic disease self-management and its implications have the potential to be incredibly powerful. The power of these findings suggest that social network theory ought to be taught in schools of public health, nursing, medicine, engineering, and informatics where technological solutions are conceived and developed.
Technology supports connection
The variety of techniques demonstrated in this body of research to support connection can be celebrated. Within these studies, there are nurse coaches, dietician coaches, family support, text messages, phone calls, interactive voice mails, nurse-mediated discussion forums, elaborately developed web content, Facebook pages, Twitter accounts, email messages and video blogs. The blend of traditional approaches with modern technology, however seemingly simple, was varied and thoughtfully constructed. Each serves to embrace the patient and make her feel as though she is being supported between office visits. Technology in this way can be seen as an extension of the healthcare provider. In a system that affords an American physician, on average 10 to 15 minutes per patient encounter (58,59), technology has the potential to extend the time spent with one’s doctor beyond the confines of the examination room. In a healthcare system that is focused on patient experience, technology has the potential to play an important part in patient perception and satisfaction.
Patients will use technology to connect
It is encouraging that patients are willing to interact with their healthcare teams in this way with technology, even if the technology appears to be as simple as answering the phone or replying to a text message. We learned from multiple studies performed with vulnerable populations that technology has the potential to level the playing field and bring much needed healthcare resources (emotional and informational support) to people in rural or socio-demographically disadvantaged regions. The fact that this holds true even for aged and racially diverse samples should encourage the use of technology in future research with disparate populations.
Connection with technology changes outcomes
In the population of patients with diabetes, moving the HbA1c to an acceptable range is one of the most meaningful things you can do to ensure long-term control of the disease with minimal risks and side-effects. Several studies demonstrated a positive impact on glycemic control with the use of technology to support patients in self-management; Turner and Rotheram-Borus (2,49) used supportive messages delivered by text messages, Chan et al. (36) used a telephone-based peer support system, Chomutare et al. (31) tested a social-media app on a smart phone, a specialized app helped adolescents in Canada to increase the number of daily blood glucose readings. Other related outcome variables also showed positive movement; Eakin’s (37) participants achieved weight loss and increased physical activity with a telephone-delivered program and Fukuoka’s (42) participants achieved weight loss, reductions in hip circumference, blood pressure and total cholesterol with a web-based program that was combined with in-person and telephone support. Technology studies have struggled in the past to move the needle on health-related outcomes, and so these results are encouraging and embolden future testing.
Connected Health is ready for testing
One of the goals of this literature review was to assess the state of the science. Prominent nurse researchers (60) suggest that disciplinary knowledge is built by first identifying and describing phenomena of interest and then by discovery through progressive levels of exploration, explanation, and prediction as knowledge and evidence is amassed. Identification research seeks to identify and name the phenomenon of interest. Description research seeks to define the prevalence, characteristics, frequency, or importance of the phenomena. Exploration research defines factors related to the phenomena (e.g., antecedents, process of experience, the nature of its evolution). Research in the explanation stage seeks to unearth underlying causes, causal pathways, theoretical explanations, meaning, or why a phenomenon exists. Finally, prediction and control research determines causation, directionality, the prevention or control of phenomena (60,61). In this sample of 35 articles, there were: 1 study (3%) at the identification level, 3 (9%) at the descriptive level, 22 (63%) at the exploration level, and 9 (26%) at the prediction level. The state of the science then, is firmly grounded in the exploratory level of knowledge, defining factors related to social support, connection, and health outcomes, seeking to understand the relationships between variables. The volume of exploratory research suggests that we are ready to move toward testing interventions that utilize these phenomena to achieve desired outcomes.
However, several factors may hinder our efforts. First, there is a lack of standardization when it comes to defining and measuring the phenomena of social support and connection. The research community would quicken the testing and dissemination of methods and findings if there were agreement on relevant definitions and standardized instruments of measurement. Second, self-management is a complex construct that does not lend itself to easy partitioning. We likely need more sophisticated study designs if we are to adequately assess which element of a comprehensive program is affecting the outcome (62), asking how exactly do the “interventions impact the psychosocial aspects of the lives of people with diabetes?” (63). Third, very few studies made use of a guiding theoretical framework, and none were judged to be in the explanatory stage. Social support is often seen as both a problem and a solution. Self-management is often seen as a process variable and an outcome measure. These facts alone suggest that we do not fully understand the phenomenon we are attempting to predict and control through randomized controlled trials. Authors such as Christakis, Fowler, and Pinker have convinced us that the science of connection is nuanced and complex, and that the people in our social networks influence us in a multitude of profound ways. There is an opportunity for future researchers to conduct theoretical work that will serve to advance the state of the science.
Limitations
The limitations of this study include (I) the possibility that studies were unintentionally left out of the sample or inappropriate inclusion of studies that biased results; (II) failure to search other, relevant databases; (III) a limited 5-year time span; (IV) publication bias; (V) improper definition of terms used in the search; and (VI) the potential of reviewer bias.
Conclusions
The research studies collected in this integrative review serve to underscore the importance of social support and connection in patients with diabetes as they journey through their life’s work of self-managing chronic disease. Clearly, being connected to someone who cares is good for your health. Implications for practice include a willingness to utilize technology to reach patients between appointments, and ensuring appropriate family support mechanisms are in place through suitable patient and family engagement strategies. Members of the HIT community are well positioned to support this work as varied patient populations in a variety of countries and settings have shown a willingness to utilize HIT to connect with each other and with their healthcare providers.
Acknowledgements
The author wishes to acknowledge funding from Project HoneyBee (http://www.sustainablehealth.org/honeybee/) through the Center for Sustainable Health at Arizona State University in support of this manuscript and the scholarship of Dr. Michael Birt who constructed the research hypothesis, “Being connected to someone who cares is good for your health”. In addition, Kevin Uchimura, BSE, MS, manages a database of connected health devices for Project HoneyBee and provided a summary of those devices for this article.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Ornish D. Love and survival: the scientific basis for the healing power of intimacy. New York, NY: Harper CollinsPublishers; 1998.
- Turner JW, Robinson JD, Tian Y, et al. Can messages make a difference? The association between e-mail messages and health outcomes in diabetes patients. Human Communication Research 2013;39:252-68. [Crossref]
- Yang YC, Boen C, Mullan Harris K. Social relationships and hypertension in late life: evidence from a nationally representative longitudinal study of older adults. J Aging Health 2015;27:403-31. [Crossref] [PubMed]
- Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory, research, and practice. 4 ed. San Francisco: Jossey-Bass; 2008.
- Brown B. The gifts of imperfection. Center City: Hazelden Publishing; 2010.
- Centers for Medicare and Medicaid Services. Electronic Health Records (EHR) Incentive Programs [updated 04/10/2014 9:51 AM]. Available online: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/ehrincentiveprograms/
- Uchimura K. Database of connected health devices [online]. Email to Karen Colorafi (karen.colorafi@asu.edu) 2016 Feb 5 [cited 2016 Feb 5].
- Association AD. Statistics about diabetes: data from the national diabetes statistics report, 2014 (released June 10, 2014). Available online: diabetes.org/diabetes-basics/statistics
- Ryan P, Pumilia NJ, Henak B, et al. Development and performance usability testing of a theory-based, computerized, tailored intervention. Comput Inform Nurs 2009;27:288-98. [Crossref] [PubMed]
- Ryan P, Sawin KJ. The individual and family self-management theory: background and perspectives on context, process, and outcomes. Nurs Outlook 2009;57:217-25.e6.
- Ryan P. Integrated Theory of Health Behavior Change: background and intervention development. Clin Nurse Spec 2009;23:161-70. [Crossref] [PubMed]
- Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs 2005;52:546-53. [Crossref] [PubMed]
- Huang MC, Hung CH, Stocker J, et al. Outcomes for type 2 diabetes mellitus patients with diverse regimens. J Clin Nurs 2013;22:1899-906. [Crossref] [PubMed]
- Dunkler D, Kohl M, Heinze G, et al. Modifiable lifestyle and social factors affect chronic kidney disease in high-risk individuals with type 2 diabetes mellitus. Kidney Int 2015;87:784-91. [Crossref] [PubMed]
- King DK, Glasgow RE, Toobert DJ, et al. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care 2010;33:751-3. [Crossref] [PubMed]
- Okura T, Heisler M, Langa KM. Association between cognitive function and social support with glycemic control in adults with diabetes mellitus. J Am Geriatr Soc 2009;57:1816-24. [Crossref] [PubMed]
- Piette JD, Rosland AM, Marinec NS, et al. Engagement with automated patient monitoring and self-management support calls: experience with a thousand chronically ill patients. Med Care 2013;51:216-23. [Crossref] [PubMed]
- Ramal E, Petersen AB, Ingram KM, et al. Factors that influence diabetes self-management in Hispanics living in low socioeconomic neighborhoods in San Bernardino, California. J Immigr Minor Health 2012;14:1090-6. [Crossref] [PubMed]
- Rosland AM, Heisler M, Choi HJ, et al. Family influences on self-management among functionally independent adults with diabetes or heart failure: do family members hinder as much as they help? Chronic Illn 2010;6:22-33. [Crossref] [PubMed]
- Idalski Carcone A, Ellis DA, Weisz A, et al. Social support for diabetes illness management: supporting adolescents and caregivers. J Dev Behav Pediatr 2011;32:581-90. [Crossref] [PubMed]
- Bai YL, Chiou CP, Chang YY. Self-care behaviour and related factors in older people with type 2 diabetes. J Clin Nurs 2009;18:3308-15. [Crossref] [PubMed]
- Balkhi AM, Reid AM, McNamara JP, et al. The diabetes online community: the importance of forum use in parents of children with type 1 diabetes. Pediatr Diabetes 2014;15:408-15. [Crossref] [PubMed]
- Fortmann AL, Roesch SC, Penedo FJ, et al. Glycemic control among U.S. Hispanics/Latinos with diabetes from the HCHS/SOL Sociocultural Ancillary Study: do structural and functional social support play a role? J Behav Med 2015;38:153-9. [Crossref] [PubMed]
- Hackworth NJ, Hamilton VE, Moore SM, et al. Predictors of diabetes self-care, metabolic control, and mental health in youth with type 1 diabetes. Australian Psychologist 2013;48:360-9.
- Karlsen B, Oftedal B, Bru E. The relationship between clinical indicators, coping styles, perceived support and diabetes-related distress among adults with type 2 diabetes. J Adv Nurs 2012;68:391-401. [Crossref] [PubMed]
- Koh D, Miller YD, Marshall AL, et al. Health-enhancing physical activity behaviour and related factors in postpartum women with recent gestational diabetes mellitus. J Sci Med Sport 2010;13:42-5. [Crossref] [PubMed]
- Ciechanowski P, Russo J, Katon WJ, et al. Relationship styles and mortality in patients with diabetes. Diabetes Care 2010;33:539-44. [Crossref] [PubMed]
- Kim HH, Seo HJ. HealthTWITTER initiative: design of a social networking service based tailored application for diabetes self-management. Healthc Inform Res 2014;20:226-30. [Crossref] [PubMed]
- Lee R, Whitley HP. Use of social media to support patients with diabetes mellitus. Consult Pharm 2014;29:53-7. [Crossref] [PubMed]
- Cafazzo JA, Casselman M, Hamming N, et al. Design of an mHealth app for the self-management of adolescent type 1 diabetes: a pilot study. J Med Internet Res 2012;14:e70. [Crossref] [PubMed]
- Chomutare T, Tatara N, Årsand E, et al. Designing a diabetes mobile application with social network support. Stud Health Technol Inform 2013;188:58-64. [PubMed]
- Rotheram-Borus MJ, Tomlinson M, Gwegwe M, et al. Diabetes buddies: peer support through a mobile phone buddy system. Diabetes Educ 2012;38:357-65. [Crossref] [PubMed]
- Fischer HH, Moore SL, Ginosar D, et al. Care by cell phone: text messaging for chronic disease management. Am J Manag Care 2012;18:e42-7. [PubMed]
- Battista MC, Labonté M, Ménard J, et al. Dietitian-coached management in combination with annual endocrinologist follow up improves global metabolic and cardiovascular health in diabetic participants after 24 months. Appl Physiol Nutr Metab 2012;37:610-20. [Crossref] [PubMed]
- Bond GE, Burr RL, Wolf FM, et al. The effects of a web-based intervention on psychosocial well-being among adults aged 60 and older with diabetes: a randomized trial. Diabetes Educ 2010;36:446-56. [Crossref] [PubMed]
- Chan JC, Sui Y, Oldenburg B, et al. Effects of telephone-based peer support in patients with type 2 diabetes mellitus receiving integrated care: a randomized clinical trial. JAMA Intern Med 2014;174:972-81. [Crossref] [PubMed]
- Eakin EG, Winkler EA, Dunstan DW, et al. Living well with diabetes: 24-month outcomes from a randomized trial of telephone-delivered weight loss and physical activity intervention to improve glycemic control. Diabetes Care 2014;37:2177-85. [Crossref] [PubMed]
- Frosch DL, Uy V, Ochoa S, et al. Evaluation of a behavior support intervention for patients with poorly controlled diabetes. Arch Intern Med 2011;171:2011-7. [Crossref] [PubMed]
- Nishita C, Cardazone G, Uehara DL, et al. Empowered diabetes management: life coaching and pharmacist counseling for employed adults with diabetes. Health Educ Behav 2013;40:581-91. [Crossref] [PubMed]
- Smith L, Weinert C. Telecommunication support for rural women with diabetes. Diabetes Educ 2000;26:645-55. [Crossref] [PubMed]
- Cassimatis M, Kavanagh DJ, Smith AC. Perceived needs for a supported self-management of type 2 diabetes: a qualitative investigation of the potential for a web-based intevention. Australian Psychologist 2014;49:75-85. [Crossref]
- Fukuoka Y, Kamitani E, Bonnet K, et al. Real-time social support through a mobile virtual community to improve healthy behavior in overweight and sedentary adults: a focus group analysis. J Med Internet Res 2011;13:e49. [Crossref] [PubMed]
- Gunn KL, Seers K, Posner N, et al. 'Somebody there to watch over you': the role of the family in everyday and emergency diabetes care. Health Soc Care Community 2012;20:591-8. [Crossref] [PubMed]
- Nundy S, Dick JJ, Solomon MC, et al. Developing a behavioral model for mobile phone-based diabetes interventions. Patient Educ Couns 2013;90:125-32. [Crossref] [PubMed]
- Venkatesh S, Weatherspoon L. Social and health care provider support in diabetes self-management. Am J Health Behav 2013;37:112-21. [Crossref] [PubMed]
- Huh J, Liu LS, Neogi T, et al. Health vlogs as social support for chronic illness management. ACM Trans Comput Hum Interact 2014;21:23. [Crossref] [PubMed]
- Miles MB, Huberman AM, Saldana J. Qualitative data analysis: a methods sourcebook. Third ed. Thousand Oaks: Sage; 2014.
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277-88. [Crossref] [PubMed]
- Rotheram-Borus MJ, Tomlinson M, Gwegwe M, et al. Peer support through a mobile phone system. The Diabetes Educator 2012;38:357-65. [Crossref] [PubMed]
- Sandelowski M, Leeman J. Writing usable qualitative health research findings. Qual Health Res 2012;22:1404-13. [Crossref] [PubMed]
- Hansen E, Landstad BJ, Hellzén O, et al. Motivation for lifestyle changes to improve health in people with impaired glucose tolerance. Scand J Caring Sci 2011;25:484-90. [Crossref] [PubMed]
- Ljungdalh AK, Møller JE. The social in medicine: social techniques in patient education. Health (London) 2012;16:418-33. [Crossref] [PubMed]
- Pinker S. The village effect. Toronto: Random House; 2014.
- Christakis NA, Fowler JH. Connected: the surprising power of our social networks and how they shape our lives. New York: Little, Brown and Company; 2009.
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370-9. [Crossref] [PubMed]
- Fowler JH, Christakis NA. Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. BMJ 2008;337:a2338. [Crossref] [PubMed]
- Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med 2008;358:2249-58. [Crossref] [PubMed]
- Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med 1999;14 Suppl 1:S34-40. [Crossref] [PubMed]
- Statista. Amount of time U.S. primary care physicians spent with each patient as of 2015 2015. Available online: http://www.statista.com/statistics/250219/us-physicians-opinion-about-their-compensation/
- Polit D, Beck C, Hungler B. Essentials of nursing research. Philadelphia, Pennsylvania: Lippincott, Williams, & Wilken; 2001.
- Polit DF. Statistics and data analysis for nursing research. 2 ed. San Francisco: Pearson; 2010.
- Stellefson M, Chaney B, Barry AE, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res 2013;15:e35. [Crossref] [PubMed]
- Tan CC, Cheng KK, Wang W. Self-care management programme for older adults with diabetes: an integrative literature review. Int J Nurs Pract 2015;21 Suppl 2:115-24. [Crossref] [PubMed]
Cite this article as: Colorafi K. Connected health: a review of the literature. mHealth 2016;2:13.